In Malaysia, Crohn’s disease is also known as “Western Disease” or “Rich People Disease.” The reason behind this is mainly because Crohn’s is a rare disease in Asia, particularly in Malaysia, as compared to Western countries. Many in Malaysia have never heard of this disease. Therefore, they are not aware of the Crohn’s and colitis patients’ struggles with their pain, medical procedures and psychological issues.
At the beginning stage, I had no one to guide me. I had no idea on how to handle my newly diagnosed disease. With no medical background, no one in the family or friends with similar conditions, I struggled to cope with this disease and my normal life. Can you imagine the struggles I faced as a first year university student with my condition? I was alone and I didn’t even understand what was going on and my normal was no longer a normal. The internet was my only resource for information other than my doctor. By reading everything I could find in the internet, I slowly started to understand this disease. Back then, there wasn’t even a support group for Crohn’s in Malaysia as the disease is relatively unknown to Malaysians. In fact, I didn’t even known about any other Crohn’s patients until I met one almost a year later after my diagnosis. My gastro doctors encouraged me and other patients to start a group so we could create a support system to each other. Now, newly diagnosed Crohn’s patients or caregivers in Malaysia have access to few channels that they could use to discuss, ask, guide and support each other going through this painful disease.
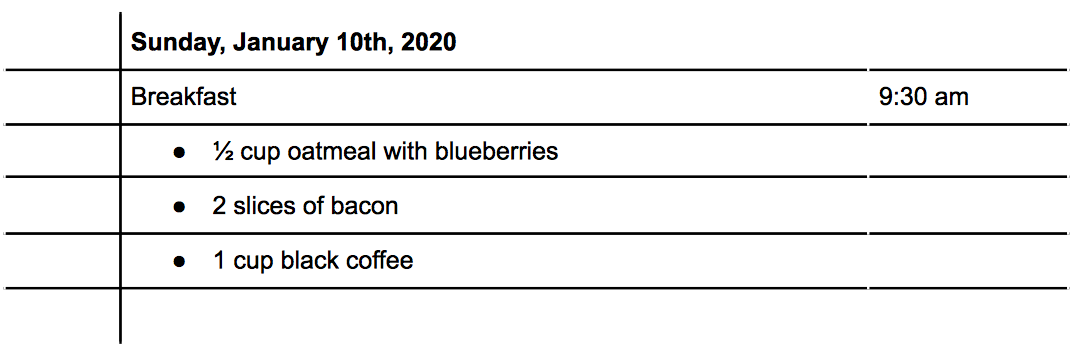
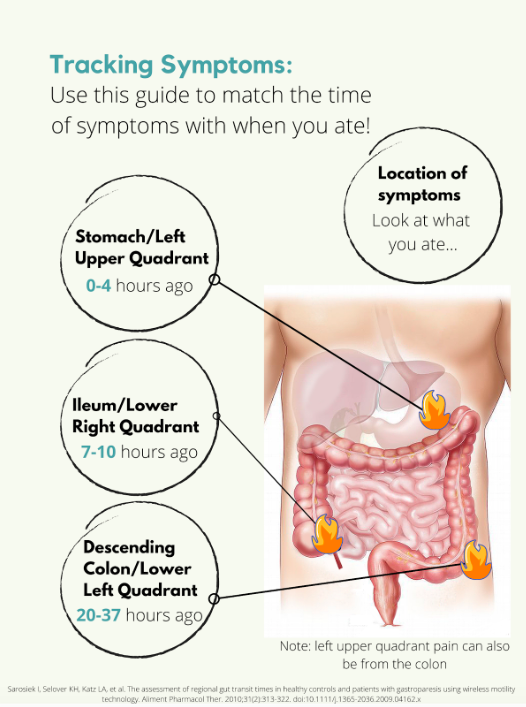
Living with chronic disease, I had to adjust and adopt to new diet and lifestyle. Changes in diet were mostly trial and error in the beginning. I had to monitor my consumption and take note of any changes. Why did I have to monitor those changes? It is simply because I wanted to avoid flare ups that were caused by certain food that I consume. For me, I found that my Crohn’s is mostly under control when I avoid foods that contain eggs. So I have to ensure my daily food consumption is egg free. If I didn’t, I’d have to visit toilet frequently the whole day. Precaution is needed for Crohn’s patients because flare ups can happen in any situations, therefore any heads up is a good one to have.
Apart from my diet, I had made some massive changes to my daily activities too. Since I’m an Ostomate, I have to ensure that I don’t partake often in hardcore sports in order to avoid stoma prolapse.
The understanding and acceptance of IBD in society is still a challenge for me. Most of them, as I mentioned above, do not know about Crohn’s disease. I remember one of my friends asking me “Sara, is your disease infectious?”. At that time, I just laughed and say “No, it doesn’t”. The lack of awareness, although understandable, is a huge disappointment when someone I confided in is not taking any initiative to understand it.
Stress is another thing that I started to consciously manage. What is the connection between Crohn’s and stress? Well, stress generally affects a person emotionally and mentally as it damages a person’s emotional equilibrium. But it also affects the person’s health. Even a person without chronic disease can feel their health being affected by high stress levels. So, anyone with chronic health issues, such as IBD patients, have higher chances of having a relapse and flare when they are stressed. It is imperative that I recognize my stress inducers, my stress level, my tolerance level and ways to reduce stress so that I do not have chronic flare ups. Although it is impossible to live stress free all the time, I believe that I should try to manage stressful situations to the best of my abilities.
Navigating relationship with Crohn’s is complicated and challenging. Crohn’s has created ups and downs in my relationships with my family, friends and loved ones. In the beginning it was really hard to explain to them my condition. They did not understand the condition or why and how I got this disease in the first place at all. It took a while for my family to accept my condition and now they are slowly getting used to it. They are a great support for me at the moment, and my heartfelt thanks.
Dealing with Crohn’s is tough enough and unfortunately, Crohn’s is not something that we can ignore or that it will disappear one day. Every single day is a challenge for me because I go through physical and psychological pain. I have to survive, improve my quality of life and live my life as normal as possible; I hope more people will become aware of Crohn’s disease, of patients’ struggles, and accept their conditions. Be kind even if you don’t see someone’s struggle, their pain or their decreasing health.