NEWS
"But You Don't Look Sick" - A Photo Journal
By Vasiliki-Rafaela Vakouftsi from Greece.
“But you don’t look sick”. How many times I have heard this? Maybe I don’t look sick to you but I am sick and my daily life is far from what you may think.
I tried to captures in pictures my daily routine as a chronic patient and I’m going to share them with you.
First of all, let me tell you some things about me. My name is Vasiliki-Rafaela, I’m a musician and I have Crohn’s Disease, Adrenal Insufficiency, Psoriasis and Psoriatic Arthritis. I have written a book about my journey with Crohn’s and a book about my life with Adrenal Insufficiency. Also, I really like traveling and I really miss it with the pandemic.
Now let’s start with the hospital visits…
...the hospital stays and therapies…
...the hospital stays and therapies…
...take the pills, medicines and supplements…
...and maybe today is the day of the week for the injection for Crohn’s…
...or maybe I need the emergency shot for Adrenal Insufficiency…
And now it’s time for a walk.. Don’t forget to carry the pills with me...
...and of course my medical ID…
Back at home again.. Really exhausted...Let’s check the e-mails and read a book before going to sleep
That’s a little idea of how my daily life is. But, you’re right. So before saying “You don’t look sick” think of what is behind the image and what you cannot see…
Invisibile Disabilities
When we hear the word disability, our mind goes to a wheelchair, mobility problems, deformities and everything else obvious.
But is disability always visible?
The answer is no. Disability is not always visible.
Society's prejudice and stereotypes about disability want the individual to show obvious signs of disability. Inadequate information, distorted perception and misinformation perpetuate these stereotypes. People with chronic diseases, such as some autoimmune diseases, but also other diseases, often have nothing in their appearance that openly displays their disability.However, people with these diseases experience a form of disability, vital functions of their body are affected and their lifestyle is shaped accordingly. The professional status of the individual and / or his socialization and integration into society can also be affected. They depend on expensive treatments, they need several hospitalizations, surgeries, etc.And as if that were not enough, they have to fight a battle as "invisible" in a society full of prejudices and stereotypes, a society that discriminates against their disability.
I do not think there is anyone who does not want to be healthy; everyday life is hard in a society that daily degrades your dignity. Almost every day you have to prove yourself, and explain again and again..because you have an invisible disability. And to be treated in the worst way, because you do not fit the mold they have as a given.
Is the state responsible for this situation? Of course state has a great responsibility.It is the state that has the obligation to educate and sensitize the citizens about the various forms of disability, to cultivate mutual respect. It is the state that has the obligation to ensure the conditions for the integration of people with disabilities in society, to give people with disabilities equal opportunities for education and work, insurance and care. And above all, the state is the one that, in the difficult economic and social conditions in which we live, has a DEBT to protect people with disabilities and to defend their rights.
People with disabilities do not ask for sadness and pity, they ask for equal treatment.
But let's start with something basic: Let us not judge others by their appearance. We never know what battle they are fighting and what is hidden behind their appearance and their smile.
Calling in Sick and IBD
Hustle culture - committing your life to your job and career - has become normalized and even expected in young adults. After graduating university, many find their self worth linked to their career, earning promotions, competing with coworkers, and impressing your boss. As a twenty something year old with Inflammatory Bowel Disease, the struggle to balance work with your health is never ending.
Those with a chronic illness understand not to take life for granted and that each day can be as unpredictable as the next, but we often forget this and get caught up in prioritizing a career over our own health and wellbeing. Calling in sick to work is inevitable, everyone has to do it at some point in their lives, whether it’s for a mental health day, the flu, or a flare-up. Yet, there are so many negative stigmas around missing work and around prioritizing your body.
The feelings of guilt that come with calling in sick to nurture your body, whether you see your body deteriorating, know a flare is coming, or if a flare comes out of the blue, can be overwhelming. The stigma associated with hustle culture and calling in sick can feel disheartening. I have always had a hard time taking a sick day, and I always felt like I was letting my boss and coworkers down and that I wasn’t worthy of employment. Intense feelings of frustration and annoyance invaded my mind when debating whether to call in sick and these intrusive thoughts caused my body more stressors on top of being physically ill. I often remind myself that prioritizing my body is my number one job. Without my health, I wouldn’t have a job and I wouldn’t be able to participate in all the amazing experiences life has to offer.
A helpful comparison to calling in sick is the safety instructions reviewed when boarding a flight, right before take off. The flight attendant always reviews the emergency instructions, stating that if the plane were to lose oxygen, you are always to put on your own oxygen mask before helping someone else. Putting yourself first will enable you to not only succeed at your job, but also to succeed in other aspects of life. If you were to ignore your body’s signals that you need rest, you will become more sick and risk the most important thing, your health.
You are not weak, undeserving, or less important than your colleagues and friends because you need to call in sick more often than the average person. You are strong, resilient, and brave. We battle a viciously unpredictable disease that many do not understand. Do not let your worth be measured by whether you call in sick. I challenge you to listen to your body and honour what your body is saying, you never know how far you will fly until you respect and love yourself and with that includes respecting your body’s limits.
Recently, I took two sick days at work due to a small flare up and my boss and coworkers were overly supportive. Although feelings of guilt surfaced when I was making this decision, the second I returned to work, everyone showed how much they cared about my wellbeing.
If you are experiencing toxicity in the workplace, contact the Human Resources department. If your company does not have a HR department, set up a meeting with your boss or manager. If you continue to be pressured to not take sick days, to put your job before your health, this may be time to look for another job and boss that cares about you and allows you to put your health first.
On this note, being able to call in sick has undeniable privilege. Many people across the world are unable to call in sick without suffering financially or being penalized at work. Openly having these hard conversations during the hiring process or with your HR department will contribute to breaking the stigma and providing accommodations for those that are chronically ill. It’s important to speak with your boss or HR representatives regarding sick leave, paid sick days, and working from home options. Speak up to your government representatives and express the need for a handful of mandatory paid sick days across your province or state.
Celebrating Black History Month in the IBD Community
“Representation creates trust, so why aren’t there more people who look like me included in research and education?” This quote by Melodie Narain-Blackwell brilliantly describes the feelings that so many Black and brown IBD patients have. In recognition of Black History Month, what can we as a chronic illness community do to support our fellow Black IBD patients this month? Standing in solidarity with this marginalized community, helping amplify their voices, and acknowledging their experiences are ways to starting bridging those gaps.
It is important to support BIPOC patients by recognizing the additional barriers that minorities, especially those in the Black community, face when navigating medical care and public health. Historically, Black people have been marginalized, abused, experimented on, and underrepresented in medical trials and research. Being seen as easily disposable, Black people have had to endure the systemic injustices of medical discrimination and medical racism. Crohn’s and ulcerative colitis are chronic diseases that statistically occur less frequently in African-Amercian populations. Statistics also show that Black people are more likely to not have their symptoms believed or validated, which has ushered a crisis of misdiagnoses. It is clear that implicit bias and antiquated medical beliefs are factors in the hesitation that Black people experience in the medical field. This phenomenon has led to an inherent distrust of medical institutions and treatment in the black community. As IBD patients we understand that having the right diagnosis and starting treatment is vital for healing and longevity. This concern is magnified in the Black community due to the systemic injustices previously mentioned.
When I first started to become ill in 2019, I did have some internal generational trauma that made me hesitant when seeking medical care. After months and months of pain I finally decided to go to the hospital to get some answers. When speaking to the doctor about symptoms, I vividly remember feeling an overwhelming sense of unease rattle through my bones. What happens if my experiences and symptoms aren't taken seriously? How can I truly convey the severity of how I feel? Although I did not receive a proper diagnosis from the hospital, I was lucky enough to have the staff members at the hospital believe and validate me. I was privileged that this was not an overtly terrible experience, but it does not take away from any reservations I had, as well as the reservations that countless other Black people have.
We must acknowledge and hold space for Black people within the IBD community through advocacy. Having a diverse range of anecdotes and stories will only propel this community to further embrace the lived experiences of so many Black and brown people who are voiceless. Education and conscious activism will only lead to more positive intersectional change.
In recognition and celebration of Black History Month, here are a few black pioneers in the IBD community as well as Gastroenterology:
Sadye Beatryce Curry was the first female African-American gastroenterologist in the United States. On top of her endless list of accomplishments, she was a founding member of the Leonidas Berry Society for Digestive Disease as well as the first woman to be elected chair for the Internal Medicine Section of the National Medical Association.
Leonidas Berry was the first African-American gastroenterologist in the United States as well as a pioneer for the advancement of endoscopy procedures. Dr. Berry also invented the gastroscopy scope. Leonidas Berry has a passion for bridging the gap of racial problems in public health.
Gary Richter is a gastroenterologist and currently runs Consultative Gastroenterology in Atlanta, and has become the first African-American president of the Medical Association of Atlanta.
Melodie Narain-Blackwell is the founder of Color of Crohn’s and Chronic Illness (COCCI) which is a nonprofit focused on increasing quality of life for minorities who battle IBD and related chronic illnesses.
Pandemic, Lockdown, Isolation and Chronic Illness
It has been almost a year now and we are still in the middle of a pandemic waiting for our lives to return to normal. However, reality may never be the same again.
So much has changed, but it seems like nothing and it makes it difficult to feel the comfort of real security.
My return - and the return of many other patients with chronic conditions- to normality may be further away than most of you. But I know that all this is equally difficult for all of us.
They say that only the elderly and people with underlying diseases are at risk. The vulnerable population.
But what happens when you are the vulnerable?
I belong to those who they call vulnerable. I never hid my illness nor was I afraid of the stigma.
I look young and healthy, but I’m not!
I’m immunosuppressed, which makes me vulnerable to any kind of infection.
We have been in lockdown for months. This is certainly not easy, nor is isolation.
I understand that it is difficult to change your daily life, but do you know how many times we, the vulnerable, have changed our daily lives not because we wanted to, but because our health imposed it?
How many times have we canceled a plan at the last minute, favorite foods we stopped eating, parties we missed and much more?
For those of us who are vulnerable, it is not so foreign to stay home, since we have spent long stays in our home and before COVID-19.
I am in quarantine for a long time. It is not easy, it dissolves your mood, your body. Staying home is unbearable for everyone.
Isolation, despair.
And it is now that we are all looking for ways to balance our security with our contact with the world.
All of this is not so foreign to me. I have some chronic illnesses that require me every day to choose what to do and what not to do. Even before the pandemic, I was very careful, evaluating what was safe to do and what was not.
I do not understand big differences in my own life now with quarantine; that I am not allowed to be touched, that I can not go to the hospital and maybe two or three more things.
And recently I made a finding that has a lot in common with today's reality.
I realized that my illnesses will never leave me, while a cure seems like a distant dream for now.
Yes, I can take steps to improve every day, but what I thought as “normal” in previous years may never come again. For many years I waited for the cure to continue my life. Now that I accepted that I would carry my diseases with me, I gained freedom. My goal now is not to be cured, but to live better.
So as I realized that it is not realistic to wait for the cure to live, so is the pause we have entered because of COVID-19 until our life is “normal” again.
And this is the real challenge: how to move on and stop waiting to get back to normal.
Stay safe!
Planning with Crohn's
Stay with me for this one – I promise it won’t be as boring as it sounds! If you immediately switch off when you hear the world ‘plan’, or indeed ‘regime’ or ‘strategy’, you’re not the only one! There are, however, benefits to planning when you live with a chronic condition like Crohn’s Disease – and more importantly, if your plans become routines, then they’re more likely to become second nature, and you’ll find yourself doing those tasks subconsciously. Here, I will share some of my planning tips, which you may just find helpful. It’s all about finding what works for you so that you can manage to fit in all of the things you want to do, despite your health condition(s).
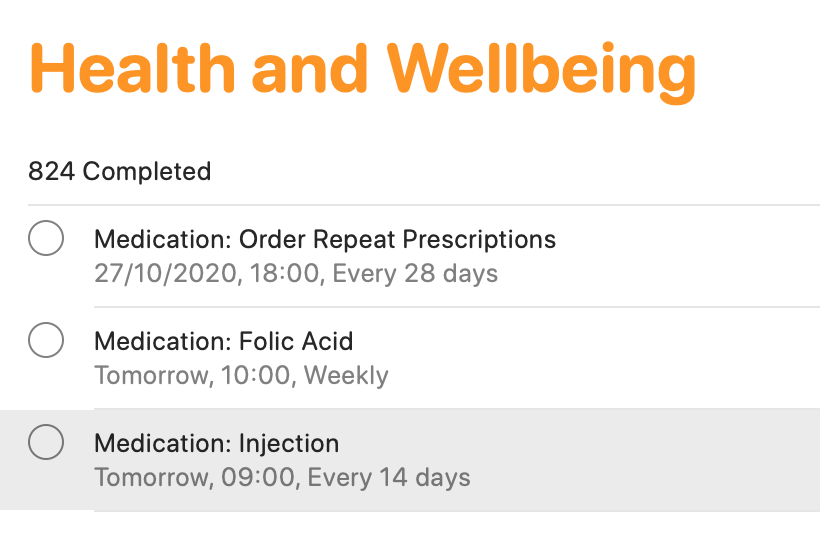
Smartphone apps
There are tons of smartphone apps available to help you keep lists, plan activities and so on! I keep it fairly simple, making use of macOS/iOS Calendar, Reminders and Notes (or the same apps on other operating devices). The calendar function is ideal for noting down all of your appointments. This helps for looking to the future, but also looking back at when and where different events occurred. The reminders app is an absolute lifeline for me. I have separate folders for different activities (e.g. university, health, work, voluntary commitments and so on). I add in activities, and a date/time (or location) reminder. This definitely helps me to keep track of everything that I need to do. If I didn’t, I would definitely forget! From a health tracking perspective, this is ideal as a reminder for booking in my next vitamin B12 injection which takes place every three months, as well as for when I need to ring up my doctor to arrange routine blood tests, when I need to self-inject my treatment, and when I need to order my repeat prescription. You may think that you’ll remember everything, but when you are busy with ‘life’, on top of ‘brain fog’ which many of us can relate to, it’s easy to forget. I know I have done that in the past, particularly when it came to self-injecting my treatment. I would remember that I need it on Tuesday for example, which would be the two-week dose period. However, I would have a busy day at college, would forget when I came home, and then in bed at night, I would suddenly remember, and think ‘I’ll have it tomorrow’. But then tomorrow became the weekend, and before I knew it, it may be a whole week later and I still hadn’t given myself my injection. I knew that was no good, but I just needed to do something about it – which I did!
Finally, Notes are brilliant! Again, I have different folders for a whole variety of different items. ‘Health’ is one of those. I use notes for keeping track of how I have been feeling, as well as for noting down points to discuss with my healthcare teams. I also use notes to keep track of discussions held with healthcare professionals, either face-to-face or over the phone. It’s just another good way to have information at your fingertips to help with your care, while the discussions are still ‘fresh’ in your head.
Scheduling in rest days
We all know what it’s like to live with a condition like Crohn’s – we have so much robbed away from us. As a result, when you are feeling on the better side, you will naturally try to fit in everything that you can. I know that I have been there! Though sometimes, it really doesn’t pay off. That’s why I try to give myself time and space to just ‘do nothing’ – because I know that’s what my body needs. In pre-pandemic times, I would avoid booking in too many back-to-back travels, so that I always had some time to recover. In the current climate, I do my best to block off certain days where I’ll have meetings, keeping overs ‘free’ to do work at my own pace, and also take it easy. It’s all about being in control, as much as possible, so that you give your body (and importantly, your mind) the time and space to breathe.
Leaving the house with everything that you need
Phone. Wallet/purse. Keys. Mask! The list goes on – but it’s really important to have everything that you need to hand. As well as the usual items that most of us require these days, I also have supplies in my backpack and car for every eventuality. This includes painkilling tablets and gel, anti-spasmodic tablets to help with cramps, laxative tablets if I notice a blockage, anti-diarrhoeal tablets if the opposite happens, lactase enzyme to help me digest products containing lactose and the RADAR key to access locked accessible toilets. This list can go on and will depend on personal circumstances. I always find it best to have everything stored in one bag, so you can ‘grab and go’. It may feel excessive, but you will thank yourself later on when you’re not caught short.
Knowing your triggers and avoiding them
Although everyone is different, we all have some kind of trigger which can worsen how we feel. For me, I know that stress is a key trigger for worsening symptoms. That’s why I try to minimise stress as much as is practically possible – although that is much easier said than done! That’s why you’ll generally see me planning to do work well in advance of deadlines, for example, and seemingly ‘being on top’ of everything. In reality, it’s much harder to do, and I do find myself rushing for deadlines still – but at least I have minimised that as much as is practically possible. I am also my own worst enemy. As a perfectionist, I place huge amounts of pressure on myself to succeed and to do everything to the very best of my abilities. While it’s a good quality to have, it isn’t when it impacts on your health. So, it’s really important to be kind to yourself, and to re-evaluate your workload if you find yourself totally swamped and feeling ill. Nothing is worth more than your health.
Do you have any other planning tips which help you to live with your condition whilst getting through life? Let us know in the comments and on social media!
Explaining Chronic Pain
This article is sponsored by Gali Health.
One of the most troubling and tricky feelings of the human condition is pain. It’s the body’s warning signal that something is wrong. It always seems to show up unexpectedly. It’s the world’s worst party guest. Seriously, it could at least bring a party gift, or an extra bag of chips and salsa to share. Instead, it interrupts the flow of midnight ragers and days of routine alike. Pain is the ultimate consumer. It takes, absorbs, and swells, without giving any of itself up. To make it even more complicated, pain comes in more hues, flavors, and shapes than can be counted. Pain is a universal experience, but the experience of pain is unique to each individual.
There is round, smooth, aching pain that rolls around the body all day. There’s sharp, jagged pain that cuts, stabs, and leaves a metallic taste on the tongue. There’s pain that shapeshifts. It howls like a werewolf, then sizzles like the sting from an insect. I could go on, but the list of the types of pain is again endless. That said, living with a chronic illness like IBD means tasting an entire buffet’s worth of pain types. Despite the fact that pain is so specific, and individual, people often try to measure and compare pain. As a chronically ill individual, it can be frustrating to have your pain compared, and rationalized by others. For instance, people will often compare the abdominal pain from ulcerative colitis, or Crohn’s disease to a stomach ache. In reality, chronic pain is much different from everyday pain.
When the pain from chronic illnesses is compared to pain from other illnesses, a large part of the context is ignored. Patients with chronic illnesses and pain have to confront pain oftentimes on a daily basis, and manage pain oftentimes without a totally effective treatment. The pain from a stomach ache, or a stubbed toe will eventually fade, and if it doesn’t, there is generally an effective treatment available. With a chronic illness, no such treatment necessarily exists. There is no timeline for recovery from the pain. Instead, it can be endless and unclear with multiple trials of various treatments required in order to find relief. In essence, chronic pain has no end deadline.
Despite this, the chronically ill often live normal lives everyday. Patients and pain sufferers go to college, go to work, and even to social events despite their pain. It’s especially important to remember this, because for all of its flavors, pain can be quite invisible. Dealing with pain is a challenge, and a burden, but millions of people around the world surmount the obstacle of pain everyday. Accommodations for patients make living with this weight easier, and enable us to be more active members in our communities. Still more work needs to be done to improve the quality of life for those dealing with pain. The compassionate way to treat the chronically ill, is the most inclusive way and the way that eliminates the disadvantages of the disabled. In the future, I hope all pain is treated with the utmost consideration and care for the individual. After all, if that was the case, there would be a lot less physical, and mental pain in this world.
This article is sponsored by Gali Health
Gali Health is an AI-based personal health assistant app helping people with inflammatory bowel diseases (IBD) proactively manage their condition. Gali gathers knowledge from daily interactions and health monitors to tailor support and information to your specific IBD experience.
My IBD Life - Ode to Despair
I sat down to write this article with the intent of describing some personal experiences with my family and friends during a period of progressing sickness that eventually led to surgery. It’s very hard for me to segregate various aspects of that time. I was struggling on many fronts. Everything seems so intertwined. I probably would have managed better, if the only thing I had to worry about had been my health. Sometimes, I wonder if I could live through that again. The worst parts of that period were the nights. Serially failing medications had brought me to a point where I was living with severe chronic pain and total incontinence. Every night I would go through a sequence of muffled crying, screaming, and dancing, to wither and end up on the floor like a lifeless body. I did that deliberately to tire myself out and fall asleep. Every night it was the same routine. Some nights, the urge to end it all was too strong to resist. I dreaded the nights and took up a night job to cope. I thought if I forced my mind to concentrate on a job, it would help with the pain. I’d suffocate at work, and even had “accidents” at work, despite wearing diapers. Everyone around me in my home or outside was oblivious to what I did to myself in my room in the dark. My coping mechanisms bordered on the psychotic. I would strangulate my body parts to make them numb. I would try to substitute the pain with another kind of pain by using an excessively hot pad. The pain was too much. The blood was too much. The nights were too long. The thing that hurt more than the pain was that every medication would make a mockery of my attempts to live. Early promising results followed by a rapid decline leading to increased symptoms were a pattern. At my core, I’m not a very hopeful person. My life circumstances have molded me into a deeply introverted and pessimist personality. My mind constantly tries to simulate everything that can go wrong and I try my best to put control measures in place. With this disease though, I was helpless. I read vehemently, but I was not a doctor. I forced myself to cultivate hope with every new medication. However, I always ended up dejected. Sometimes, I felt like a bloody soldier struggling to stand straight, kneeling on the ground against his sword, and waiting for all of it to get over.
As I started reminiscing those nights, my intents changed. I wanted to describe that cycle of hope and consequent despair to someone. It resulted in me writing a poem which I’m sharing here.
They tell me the war is over and we won.
They tell me that the night is at last, gone.
They tell me the sun’s rising on the horizon.
They tell me, they tell me it’s a new dawn.
They tell me the same things again and again.
And each time they say it, I believe them.
I hide from my fears, behind a translucent curtain.
Weak ropes of hope bear the weight of my pain.
Soon it all comes crashing down to the ground.
And I see them again. The blood-hungry hounds.
Dread sets into me as they approach and surround.
Every inch of me bleeds. My screams resound.
And when it’s all over, I look down from the edge.
Frail, pale, broken, and defeated, after the rampage.
No antidote to my ailment, my soul feels caged.
Desperate, I am prepared to embrace the only escape.
“Stop! Don’t!” I hear a voice break the silence.
I recognize the voice. It’s them. Once again.
They praise my resilience. Talk about Providence.
Promise me there’s a reason for my existence.
They look to infuse me with hope and faith.
They tell me tales of the fierce and brave.
Why then I don’t believe what they say?
Oh! It’s because, soon after ...
They tell me the war is over and we won.
They tell me that the night is at last, gone.
They tell me the sun’s rising on the horizon.
They tell me, they tell me it’s a new dawn.
There was a time when I tried to capture my pain in words. I was better at writing then. With time, the writing started to feel like a futile exercise. The nights never went away. Instead, I now try to repress those experiences in some corner of my brain as I have done with other traumatic incidents that I have lived through.
My doctor once told me that there were only 2 patients other than me under his care, with a severity of disease that was similar to mine. I felt sad, but then I realized it’s a good thing that more people do not go through such experiences. However, I’m sure there are enough like me in my country which has a population of 1.3 billion, but I’m not sure if everyone is as lucky as me. The mental health of patients with Inflammatory Bowel Disease has never been a priority in the Indian Healthcare system. It’s time that we begin to provide holistic support to young adults with inflammatory bowel diseases to enable them to manage this disease better and come out of the experience with as little residual trauma as possible.
Please stay safe and take care. See you next month. :)
IBD and Anxiety
When you are first diagnosed with Inflammatory Bowel Disease you learn quickly that the brain and gut function as one. They are deeply connected. Even if you don’t have IBD, you can look to feelings like butterflies in your stomach when you are nervous, excited, or in love. IBD has given me the superpower of identifying an instinctual trust of my gut. One thing you commonly hear when talking about how to manage your IBD is that you have to manage your stress levels. Since the brain and gut are so connected, the chances that a flare up will occur when you’re stressed are high. Truthfully, being able to manage your stress is a very privileged thing to be able to do and that’s a conversation that needs to be had. Outside forces and systems of oppression exist heavily in our world today. We are not functioning in a world that allows you to thrive and prioritize both your mental and physical health. For most people, there is always a tremendous amount of stressors that you cannot escape. Things like finances, unstable households, going to school, and working all cause a great deal of stress.
Today, I want to specifically talk about how managing stress levels and IBD feels increasingly impossible when you have clinical anxiety and/or PTSD, as these are so often linked with IBD.
I was diagnosed with IBD at a young age. My physical health was always prioritized over my mental health. This was more pronounced, I think, because mental health is not a thing that is necessarily often invested in for young children. As a child, it was very difficult for me to identify what I was feeling and what triggered these feelings. Specifically, with my anxiety, I did not know what a neutral state of mind meant. I didn’t know what my anxiety looked or felt like till around my sophomore year of college. After going on anxiety medication for a bit, I was able to understand what intrusive thoughts were and how they occupied my life.
The baseline for my anxiety is intrusive thoughts, but it can also manifest itself in different ways just based on the things I am doing in my life at the time. For example, my anxiety can manifest itself in ways such as crying in social settings, having an obsession with time (i.e. constantly looking at the clock or leaving hours early for events), and, when things are more extreme, staying in my room for days on end. For me, it is so important to specifically state how my anxiety manifests because for so long I did not know what it meant. I think it is important that we normalize talking about everything that anxiety can bring with it, not just generalizing or downplaying it. So often, I think anxiety is talked about in very loose terms and given very simple fixes for how to “handle it.” This, in return, can oftentimes belittle the situation.
When these more intense and intrusive moments occur, my IBD flares up. So, I often question how I am to manage my stress when I often cannot control my anxieties. In the past, I would become stressed when I experienced my anxieties because I did not know what was wrong. Now, they still stress me out, even though I know that it is anxiety.
For me, and I think many others, anxiety is something that I have to constantly cope with on the daily. If I am not ten steps ahead of it, it will simply swallow me whole.
IBD and anxiety can feel overwhelming and scary, but what has helped me is knowing that I am not alone. Having these two conditions together is not uncommon, and what feels very isolating and full of despair is not the case. Medication has helped me in the past and therapy is a forever process for me. I also keep a bullet journal of coping skills I have used in the past - identifying coping mechanisms that worked and ones that did not. This list gives me a place to turn to when I feel as though nothing could help and it's easily accessible. I have also found solace in being in a community of people who understand. Explaining anxiety or IBD to someone who has not gone through it can be very exhausting and this goes for many other varying identities as well! When I do find the energy, making art is another space for me to process my anxiety, whether that be through a conceptual piece or just painting a canvas with one color over and over again.
What are ways you cope with your anxiety?
Judging Symptoms with Crohn’s
Sometimes, it feels like all gastro symptoms are inflammaotry bowel disease (IBD)-related… especially being symptomatic with IBD for so long. However, it’s not always case – which can cause a great of confusion, as well as making life just that bit more complicated!
As well as Crohn’s disease, I also have gastroesophageal reflux disease (GERD), irritable bowel syndrome with constipation (IBS-C), an internal rectal prolapse and lactose intolerance. I was diagnosed with Crohn’s disease in 2008, after several years of experience gastro-related symptoms. So, at that point, I assumed that everything I had experienced was the result of Crohn’s. What I failed to realise, and what wasn’t explained very well at the time, was that I also had GERD. I was suddenly prescribed all of this medication, without being properly informed of the purpose of each different medication.
Over time, and with the right treatment, I became more informed, and I was able to get my Crohn’s disease under control, to the point where I was deemed to be in clinical remission. This was concluded by considering blood tests for inflammation (CRP and ESR), colonoscopy and gastroscopy results, small bowel MRI scan results and faecal calprotectin results, each of them done at different frequencies over different periods of time. This happened gradually over a few years, and in the process, I learned more and more about my body. However, I began to struggle with more gastro-related symptoms, which I initially thought were a Crohn’s flare, but soon realised were not exactly the same as before my Crohn’s diagnosis. I felt bloated and constipated, I had abdominal pain, and I was passing mucus. It became clear that I most likely had IBS-C. The problem I found with IBS was that there was no quick and easy fix for it – not that there has been a quick and easy fix for Crohn’s disease, but at least I was able to take some treatment which helped control the inflammation. With IBS, I felt very much in the dark. Recommendations were an anti-spasmodic to relieve cramping, laxatives to ease constipation, and avoiding foods which seemed to make me ‘worse’. I watched what I ate very closely, and soon identified certain green vegetables as a trigger, as well as milk products, which I tried to reduce.
Little did I know, but the milk products weren’t just a trigger for worsening my IBS symptoms, but I was also lactose intolerant. I was diagnosed in 2015 – some seven years after my Crohn’s diagnosis. This only happened after one doctor felt there was something else going on and decided to test for lactose intolerance and Helicobacter Pylori infection – and thank goodness they did! I’ve managed to cut most forms of lactose completely out of my diet since, and when I can’t, I have found a lactase enzyme supplement I can take immediately before eating or drinking something containing lactose, to help me avoid those unpleasant symptoms.
I thought that was going to be it when it came to gastro problems. Then, something else came along! Originally blamed on my IBS-C, I noticed I was struggling more with constipation, despite eating a balanced and healthy diet, and doing everything else ‘right’. A couple of healthcare professionals didn’t really acknowledge my perspective, and just said I need to take laxatives permanently – something which I do take, but often feels like a ‘quick fix’ or ‘cover the wound with a plaster’, without understanding the underlying reason for these changes. Many blame IBD, plus IBS for constipation, without necessarily looking further. It sometimes feels as though assumptions are an easier option in the medical world, but not for those of us living with these symptoms. Moreover, I had observed changes beyond those I had learned to notice by living with IBD and IBS-C.
Cutting a very long story short, I ended up going for a proctogram which revealed I had an internal rectal prolapse – which is basically when your rectum folds in on itself. It wasn’t the most dignifying procedure – much like most gastro-linked investigations. Dignity often goes straight out of the window! However, this finding did explain the sharp shooting pains I had been having in my rectum, as well as the mucus I had been passing, the ‘fresh’ blood I had noticed, and why it sometimes felt as though there was a physical obstruction – because there was. The verdict was ‘there’s not much we can do’ – something I think we’re all too used to hearing. There are surgical options, but they come with risks and they more or less said they would not be considering that option for somebody of my age. So, I was sent away with pelvic floor exercises, and the notion that ‘I just have to live with it’ – which I do. At least I received an answer for the symptoms I had been experiencing, even if I don’t have an answer as to ‘why’ I have a rectal prolapse. My current hypothesis is that it is something to do with hypermobility, which has consistently been overlooked – but that’s a whole different story!
All of these different symptoms, and the conditions subsequently diagnosed, have taught me so much. I have learned to really listen to what my body is telling me – which is not easy but does improve with time. I’m not always right, but my judgement certainly seems to be stronger now, after all of these years with IBD, IBS-C, GERD, a prolapse and lactose intolerance. I am much better at distinguishing as to ‘what’ is causing ‘what’ – although it’s impossible to always be ‘right’! You just tune into what you are feeling, almost like detective work. You place pieces of the puzzle together to help you build the picture of what you think is happening. Your previous experiences and your observations guide you, alongside being proactive in terms of knowing clinical indicators, recognising new triggers, stressors or symptoms, and then being proactive in seeking the right input from the right healthcare professionals. It comes more naturally after years of having to take things into your own hands to get answers. For example, I now know that the abdominal pain and cramping that I frequently experience is when I am perhaps a little constipated as a result of IBS-C and my internal rectal prolapse; so I adjust certain parts of my diet and take additional laxatives when I begin to notice patterns changing, early on. Likewise, the ‘whale’ noises and ‘washing machine sensation’ immediately indicate that I’ve consumed something containing lactose without realising – like the time I ate a gorgeous cheesy pizza, and then realised I hadn’t taken my lactase enzyme… I suffered for the next few hours!
These conditions, in one sense, sensitise us to be more receptive to how our bodies work. I don’t think I would have been as knowledgeable or as ‘switched on’ as I am if I hadn’t been diagnosed with them – and I wish more people recognised this, particularly certain healthcare professionals. I often have grievances with professionals who rely solely on certain clinical indicators for disease remission. For example, those who just use CRP as an indicator as to whether you are in remission or not. This has happened to me in the past when I was evidently in the middle of an IBD flare, but at that point in time, I was not confident at self-managing my health. As it turned out, my faecal calprotectin was off the scale, and so some additional treatment helped me out immensely. What did I learn? Nobody knows my body better than myself. Healthcare professionals can help me the most when they listen to what I am saying, acknowledge my expertise, and then work with me to identify what is really happening, and then plan with me as to what to do to help manage symptoms so that I can get on with my life, and most importantly, have a good quality of life. So, when anybody questions what you are thinking or feeling, remind them of this point, and hopefully, they will change their approach so that it is supportive, rather than a hindrance.