NEWS
Challenges as a Crohn's Warrior in Malaysia
In Malaysia, Crohn’s disease is also known as “Western Disease” or “Rich People Disease.” The reason behind this is mainly because Crohn’s is a rare disease in Asia, particularly in Malaysia, as compared to Western countries. Many in Malaysia have never heard of this disease. Therefore, they are not aware of the Crohn’s and colitis patients’ struggles with their pain, medical procedures and psychological issues.
At the beginning stage, I had no one to guide me. I had no idea on how to handle my newly diagnosed disease. With no medical background, no one in the family or friends with similar conditions, I struggled to cope with this disease and my normal life. Can you imagine the struggles I faced as a first year university student with my condition? I was alone and I didn’t even understand what was going on and my normal was no longer a normal. The internet was my only resource for information other than my doctor. By reading everything I could find in the internet, I slowly started to understand this disease. Back then, there wasn’t even a support group for Crohn’s in Malaysia as the disease is relatively unknown to Malaysians. In fact, I didn’t even known about any other Crohn’s patients until I met one almost a year later after my diagnosis. My gastro doctors encouraged me and other patients to start a group so we could create a support system to each other. Now, newly diagnosed Crohn’s patients or caregivers in Malaysia have access to few channels that they could use to discuss, ask, guide and support each other going through this painful disease.
Living with chronic disease, I had to adjust and adopt to new diet and lifestyle. Changes in diet were mostly trial and error in the beginning. I had to monitor my consumption and take note of any changes. Why did I have to monitor those changes? It is simply because I wanted to avoid flare ups that were caused by certain food that I consume. For me, I found that my Crohn’s is mostly under control when I avoid foods that contain eggs. So I have to ensure my daily food consumption is egg free. If I didn’t, I’d have to visit toilet frequently the whole day. Precaution is needed for Crohn’s patients because flare ups can happen in any situations, therefore any heads up is a good one to have.
Apart from my diet, I had made some massive changes to my daily activities too. Since I’m an Ostomate, I have to ensure that I don’t partake often in hardcore sports in order to avoid stoma prolapse.
The understanding and acceptance of IBD in society is still a challenge for me. Most of them, as I mentioned above, do not know about Crohn’s disease. I remember one of my friends asking me “Sara, is your disease infectious?”. At that time, I just laughed and say “No, it doesn’t”. The lack of awareness, although understandable, is a huge disappointment when someone I confided in is not taking any initiative to understand it.
Stress is another thing that I started to consciously manage. What is the connection between Crohn’s and stress? Well, stress generally affects a person emotionally and mentally as it damages a person’s emotional equilibrium. But it also affects the person’s health. Even a person without chronic disease can feel their health being affected by high stress levels. So, anyone with chronic health issues, such as IBD patients, have higher chances of having a relapse and flare when they are stressed. It is imperative that I recognize my stress inducers, my stress level, my tolerance level and ways to reduce stress so that I do not have chronic flare ups. Although it is impossible to live stress free all the time, I believe that I should try to manage stressful situations to the best of my abilities.
Navigating relationship with Crohn’s is complicated and challenging. Crohn’s has created ups and downs in my relationships with my family, friends and loved ones. In the beginning it was really hard to explain to them my condition. They did not understand the condition or why and how I got this disease in the first place at all. It took a while for my family to accept my condition and now they are slowly getting used to it. They are a great support for me at the moment, and my heartfelt thanks.
Dealing with Crohn’s is tough enough and unfortunately, Crohn’s is not something that we can ignore or that it will disappear one day. Every single day is a challenge for me because I go through physical and psychological pain. I have to survive, improve my quality of life and live my life as normal as possible; I hope more people will become aware of Crohn’s disease, of patients’ struggles, and accept their conditions. Be kind even if you don’t see someone’s struggle, their pain or their decreasing health.
Planning with Crohn's
Stay with me for this one – I promise it won’t be as boring as it sounds! If you immediately switch off when you hear the world ‘plan’, or indeed ‘regime’ or ‘strategy’, you’re not the only one! There are, however, benefits to planning when you live with a chronic condition like Crohn’s Disease – and more importantly, if your plans become routines, then they’re more likely to become second nature, and you’ll find yourself doing those tasks subconsciously. Here, I will share some of my planning tips, which you may just find helpful. It’s all about finding what works for you so that you can manage to fit in all of the things you want to do, despite your health condition(s).
Smartphone apps
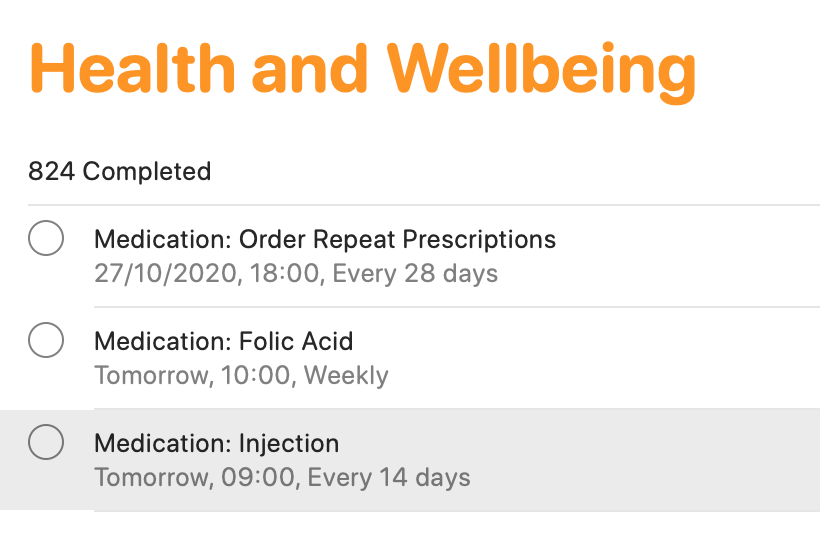
There are tons of smartphone apps available to help you keep lists, plan activities and so on! I keep it fairly simple, making use of macOS/iOS Calendar, Reminders and Notes (or the same apps on other operating devices). The calendar function is ideal for noting down all of your appointments. This helps for looking to the future, but also looking back at when and where different events occurred. The reminders app is an absolute lifeline for me. I have separate folders for different activities (e.g. university, health, work, voluntary commitments and so on). I add in activities, and a date/time (or location) reminder. This definitely helps me to keep track of everything that I need to do. If I didn’t, I would definitely forget! From a health tracking perspective, this is ideal as a reminder for booking in my next vitamin B12 injection which takes place every three months, as well as for when I need to ring up my doctor to arrange routine blood tests, when I need to self-inject my treatment, and when I need to order my repeat prescription. You may think that you’ll remember everything, but when you are busy with ‘life’, on top of ‘brain fog’ which many of us can relate to, it’s easy to forget. I know I have done that in the past, particularly when it came to self-injecting my treatment. I would remember that I need it on Tuesday for example, which would be the two-week dose period. However, I would have a busy day at college, would forget when I came home, and then in bed at night, I would suddenly remember, and think ‘I’ll have it tomorrow’. But then tomorrow became the weekend, and before I knew it, it may be a whole week later and I still hadn’t given myself my injection. I knew that was no good, but I just needed to do something about it – which I did!
Finally, Notes are brilliant! Again, I have different folders for a whole variety of different items. ‘Health’ is one of those. I use notes for keeping track of how I have been feeling, as well as for noting down points to discuss with my healthcare teams. I also use notes to keep track of discussions held with healthcare professionals, either face-to-face or over the phone. It’s just another good way to have information at your fingertips to help with your care, while the discussions are still ‘fresh’ in your head.
Scheduling in rest days
We all know what it’s like to live with a condition like Crohn’s – we have so much robbed away from us. As a result, when you are feeling on the better side, you will naturally try to fit in everything that you can. I know that I have been there! Though sometimes, it really doesn’t pay off. That’s why I try to give myself time and space to just ‘do nothing’ – because I know that’s what my body needs. In pre-pandemic times, I would avoid booking in too many back-to-back travels, so that I always had some time to recover. In the current climate, I do my best to block off certain days where I’ll have meetings, keeping overs ‘free’ to do work at my own pace, and also take it easy. It’s all about being in control, as much as possible, so that you give your body (and importantly, your mind) the time and space to breathe.
Leaving the house with everything that you need
Phone. Wallet/purse. Keys. Mask! The list goes on – but it’s really important to have everything that you need to hand. As well as the usual items that most of us require these days, I also have supplies in my backpack and car for every eventuality. This includes painkilling tablets and gel, anti-spasmodic tablets to help with cramps, laxative tablets if I notice a blockage, anti-diarrhoeal tablets if the opposite happens, lactase enzyme to help me digest products containing lactose and the RADAR key to access locked accessible toilets. This list can go on and will depend on personal circumstances. I always find it best to have everything stored in one bag, so you can ‘grab and go’. It may feel excessive, but you will thank yourself later on when you’re not caught short.
Knowing your triggers and avoiding them
Although everyone is different, we all have some kind of trigger which can worsen how we feel. For me, I know that stress is a key trigger for worsening symptoms. That’s why I try to minimise stress as much as is practically possible – although that is much easier said than done! That’s why you’ll generally see me planning to do work well in advance of deadlines, for example, and seemingly ‘being on top’ of everything. In reality, it’s much harder to do, and I do find myself rushing for deadlines still – but at least I have minimised that as much as is practically possible. I am also my own worst enemy. As a perfectionist, I place huge amounts of pressure on myself to succeed and to do everything to the very best of my abilities. While it’s a good quality to have, it isn’t when it impacts on your health. So, it’s really important to be kind to yourself, and to re-evaluate your workload if you find yourself totally swamped and feeling ill. Nothing is worth more than your health.
Do you have any other planning tips which help you to live with your condition whilst getting through life? Let us know in the comments and on social media!
What to Expect When a Loved One Gets Diagnosed with IBD
Navigating an IBD diagnosis is not easy. It can be messy and emotional and very tiring. The person diagnosed with IBD will be feeling many emotions, probably all at once. But it’s not just hard on the diagnosed individual; it can be very hard on their loved ones as well. It can be difficult to figure out what to expect and what to say and how to act when you find out someone was diagnosed with Crohn’s disease or ulcerative colitis. Hopefully this article will provide some insight into what to expect when that diagnosis happens.
The first few hours and days after your loved one gets diagnosed with IBD can be very confusing. You are processing their diagnosis, while trying to be there for them as well. While everyone processes it differently, there are likely some common reactions you can expect. Here are a few things to keep in mind:
Be prepared to simply be there for them. Whether they want to talk about it or not; whether they want you to accompany them to appointments or infusions; whether they want someone to sit with them while they are sick. And even if they don’t want any of that, make sure that they just know that you will be there if/when they do. Be there for them when they are ready to talk to you. Tell them you are there if they need anything and be ready to back it up with your actions. There is nothing worse than empty words.
Be prepared for them to become experts on their own bodies. They will become very familiar with their symptoms and will likely know when something is not right. Learn to trust that. If they tell you they think something is wrong, don’t try to argue with it.
Be willing to learn with them. For me, I read up a lot on my diagnosis. I read others’ stories, I read articles, I read medical journals. And I wanted my friends and family to understand some of what I was learning. So, be willing to read the articles they send you. Educate yourself on their disease. Don’t be afraid to be educated.
Be ready for the hard days. The days when their medication isn’t working. The days when their Prednisone is making them miserable. The days when they are in the hospital. Not every day will be hard, but some will be. So be prepared when they come. Remind your loved one that it won’t last forever.
Also be ready for the good days! The days when they find out they’re in remission. The day when they try a food they haven’t been able to eat in a while and it goes well. The days when they feel like themselves. Just as the bad days come and go, the good days will come, too.
Be ready for the doctors’ appointment. Especially when your loved one is first diagnosed and they are working to get control of the disease, there will be a lot of doctors’ visits. There will be ER visits and hospital stays. There might be infusions they have to go to on a regular basis. They may or may not want you to come. Be ready to support them either way. With COVID, they may have wanted you to come and you may not be able to. If that’s the case, try to get creative with ways to make them feel like you’re there. FaceTime them, call them, text them. Do something to make them not feel so alone.
Ultimately, be ready for a journey. It isn’t always easy and there will be really hard days. But your loved one is now part of a community that is welcoming and ready to help when they want. There will be people that they can relate to and that can understand them in ways that someone without IBD can’t understand. Encourage them to reach out to people they see on social media. Encourage them to ask questions and not be afraid to speak up. The IBD community is a great one and people are always willing to help!
Navigating a loved one’s IBD diagnosis can be a daunting thing. It is a lot to process and there is a lot of unknown. But by just being supportive and being attentive to your loved one, things will probably go a lot better than you expect them to.
Judging Symptoms with Crohn’s
Sometimes, it feels like all gastro symptoms are inflammaotry bowel disease (IBD)-related… especially being symptomatic with IBD for so long. However, it’s not always case – which can cause a great of confusion, as well as making life just that bit more complicated!
As well as Crohn’s disease, I also have gastroesophageal reflux disease (GERD), irritable bowel syndrome with constipation (IBS-C), an internal rectal prolapse and lactose intolerance. I was diagnosed with Crohn’s disease in 2008, after several years of experience gastro-related symptoms. So, at that point, I assumed that everything I had experienced was the result of Crohn’s. What I failed to realise, and what wasn’t explained very well at the time, was that I also had GERD. I was suddenly prescribed all of this medication, without being properly informed of the purpose of each different medication.
Over time, and with the right treatment, I became more informed, and I was able to get my Crohn’s disease under control, to the point where I was deemed to be in clinical remission. This was concluded by considering blood tests for inflammation (CRP and ESR), colonoscopy and gastroscopy results, small bowel MRI scan results and faecal calprotectin results, each of them done at different frequencies over different periods of time. This happened gradually over a few years, and in the process, I learned more and more about my body. However, I began to struggle with more gastro-related symptoms, which I initially thought were a Crohn’s flare, but soon realised were not exactly the same as before my Crohn’s diagnosis. I felt bloated and constipated, I had abdominal pain, and I was passing mucus. It became clear that I most likely had IBS-C. The problem I found with IBS was that there was no quick and easy fix for it – not that there has been a quick and easy fix for Crohn’s disease, but at least I was able to take some treatment which helped control the inflammation. With IBS, I felt very much in the dark. Recommendations were an anti-spasmodic to relieve cramping, laxatives to ease constipation, and avoiding foods which seemed to make me ‘worse’. I watched what I ate very closely, and soon identified certain green vegetables as a trigger, as well as milk products, which I tried to reduce.
Little did I know, but the milk products weren’t just a trigger for worsening my IBS symptoms, but I was also lactose intolerant. I was diagnosed in 2015 – some seven years after my Crohn’s diagnosis. This only happened after one doctor felt there was something else going on and decided to test for lactose intolerance and Helicobacter Pylori infection – and thank goodness they did! I’ve managed to cut most forms of lactose completely out of my diet since, and when I can’t, I have found a lactase enzyme supplement I can take immediately before eating or drinking something containing lactose, to help me avoid those unpleasant symptoms.
I thought that was going to be it when it came to gastro problems. Then, something else came along! Originally blamed on my IBS-C, I noticed I was struggling more with constipation, despite eating a balanced and healthy diet, and doing everything else ‘right’. A couple of healthcare professionals didn’t really acknowledge my perspective, and just said I need to take laxatives permanently – something which I do take, but often feels like a ‘quick fix’ or ‘cover the wound with a plaster’, without understanding the underlying reason for these changes. Many blame IBD, plus IBS for constipation, without necessarily looking further. It sometimes feels as though assumptions are an easier option in the medical world, but not for those of us living with these symptoms. Moreover, I had observed changes beyond those I had learned to notice by living with IBD and IBS-C.
Cutting a very long story short, I ended up going for a proctogram which revealed I had an internal rectal prolapse – which is basically when your rectum folds in on itself. It wasn’t the most dignifying procedure – much like most gastro-linked investigations. Dignity often goes straight out of the window! However, this finding did explain the sharp shooting pains I had been having in my rectum, as well as the mucus I had been passing, the ‘fresh’ blood I had noticed, and why it sometimes felt as though there was a physical obstruction – because there was. The verdict was ‘there’s not much we can do’ – something I think we’re all too used to hearing. There are surgical options, but they come with risks and they more or less said they would not be considering that option for somebody of my age. So, I was sent away with pelvic floor exercises, and the notion that ‘I just have to live with it’ – which I do. At least I received an answer for the symptoms I had been experiencing, even if I don’t have an answer as to ‘why’ I have a rectal prolapse. My current hypothesis is that it is something to do with hypermobility, which has consistently been overlooked – but that’s a whole different story!
All of these different symptoms, and the conditions subsequently diagnosed, have taught me so much. I have learned to really listen to what my body is telling me – which is not easy but does improve with time. I’m not always right, but my judgement certainly seems to be stronger now, after all of these years with IBD, IBS-C, GERD, a prolapse and lactose intolerance. I am much better at distinguishing as to ‘what’ is causing ‘what’ – although it’s impossible to always be ‘right’! You just tune into what you are feeling, almost like detective work. You place pieces of the puzzle together to help you build the picture of what you think is happening. Your previous experiences and your observations guide you, alongside being proactive in terms of knowing clinical indicators, recognising new triggers, stressors or symptoms, and then being proactive in seeking the right input from the right healthcare professionals. It comes more naturally after years of having to take things into your own hands to get answers. For example, I now know that the abdominal pain and cramping that I frequently experience is when I am perhaps a little constipated as a result of IBS-C and my internal rectal prolapse; so I adjust certain parts of my diet and take additional laxatives when I begin to notice patterns changing, early on. Likewise, the ‘whale’ noises and ‘washing machine sensation’ immediately indicate that I’ve consumed something containing lactose without realising – like the time I ate a gorgeous cheesy pizza, and then realised I hadn’t taken my lactase enzyme… I suffered for the next few hours!
These conditions, in one sense, sensitise us to be more receptive to how our bodies work. I don’t think I would have been as knowledgeable or as ‘switched on’ as I am if I hadn’t been diagnosed with them – and I wish more people recognised this, particularly certain healthcare professionals. I often have grievances with professionals who rely solely on certain clinical indicators for disease remission. For example, those who just use CRP as an indicator as to whether you are in remission or not. This has happened to me in the past when I was evidently in the middle of an IBD flare, but at that point in time, I was not confident at self-managing my health. As it turned out, my faecal calprotectin was off the scale, and so some additional treatment helped me out immensely. What did I learn? Nobody knows my body better than myself. Healthcare professionals can help me the most when they listen to what I am saying, acknowledge my expertise, and then work with me to identify what is really happening, and then plan with me as to what to do to help manage symptoms so that I can get on with my life, and most importantly, have a good quality of life. So, when anybody questions what you are thinking or feeling, remind them of this point, and hopefully, they will change their approach so that it is supportive, rather than a hindrance.
Emotions and IBD
There are a lot of emotions that come with the diagnosis of any chronic illness, or even any major life change. But laying on the operating table, under the haze and fading twilight of the anesthesia medication exiting my veins, I felt nothing. The echoing silence of the room was heavy all around me. I expected to feel an overflowing stream of emotions flow over me, but instead the most striking sensation of my diagnosis was emptiness. It could have been the drugs dulling my system and my perception of the world. Yet, over time, I’ve started to think that the cause of the void-like feeling around my diagnosis was something incredibly real, and not artificial. The feeling of change is oftentimes so big that it feels like nothing.
In that hospital room, so much had changed with a simple test. The scale of the moment was beyond comprehension. My parents and I communicated without words, because anything that could have been said would have failed. All the periods, letters, and adjectives in the world would never be enough to frame that point in time. So, somehow and instead, I just knew that I had ulcerative colitis without being told. Shock, and the whole experience, was such a surreal feeling. To know that something has snapped, or broken, or ended, but to be unable to directly confront that realization is off-putting. It was easier to not speak the change aloud, because to speak it into the world would make it extra real.
In the weeks after my diagnosis, it was as if a light switch had been switched back on. All of the fear, grief, and anger I had missed earlier suddenly now surrounded me. The trauma of illness is such a widespread and varied experience, but it can be difficult to describe and discuss. It’s isolating to feel different, and to feel like you’ve lost a piece of yourself. Health is something that most people take for granted or don’t think about. So when it’s taken away from you, its absence becomes the dominant part of your everyday life. The shift in my lifestyle to one focused on health had a significant impact on my mental health. I was in an environment, my freshman year of college, where everyone seems to be testing the limits of their independence. Thus, to feel completely dependent on my unstable day-to-day health felt unfair and tragic.
It’s a challenge to have the energy to battle painful, and draining symptoms on a daily basis. I learned that adjusting to my illness, and all of the treatment that comes with it, was a major part of my healing journey. On top of that, I realized that acknowledging the emotions I was experiencing was an important part of accepting my illness. It’s normal and natural to be angry, to grieve, and even to be nostalgic for your life prior to diagnosis. In fact, for me, it was the first step towards opening up and connecting with others in the chronic illness community. My experiences, feelings, and my relationship towards my health has been full of highs and lows. Most of all, I’ve learned that the negative and positive emotions I’ve encountered from dealing with illness are all valid. They’ve helped me grow, learn, and evolve as an individual. Every journey is different, and that is perfectly okay.
Studying with Crohn's
By Simon Stones
I feel as though I’ve been studying for most of my life – well, there is some truth in that! After 22 years in education, it is safe to say that I am well and truly ready for the formality of it all to end… though I know I’ll never stop learning in life!
There’s no right or wrong way to go through education, especially once you reach the end of your compulsory education. Add into the mix one or more chronic conditions like inflammatory bowel disease, and things can feel a little more complicated– especially when deciding on what you want to do, and the way in which you want to do it. Moreover, what works for one person won’t necessarily work for another – which is it’s so important to do what’s right for you.
I went straight from compulsory education to University, where I completed a four-year Bachelor’s degree in Biomedical Sciences, before going straight to a three-year PhD in healthcare. Some may say it’s sensible to get all of your education done at once. Some may say I was lucky to be able to progress through the ranks one after another. Some may also say I must be slightly bonkers. In all honestly, it’s a good mix of the three, especially the last one!
My thirst for learning really began during childhood, while living with juvenile idiopathic arthritis. As a result of my restricted mobility at the time, I struggled to participate in sport. It is here when I channeled my energy into my academic learning – my body wasn’t much use, but I had a brain and I wanted to use it. Living with a chronic condition throughout my childhood had, in one sense, conditioned me to be inquisitive and desperate to learn. Although I missed quite a lot of time at school through being at the hospital and being unwell, I never gave in. I would always be working – it could be reading, completing workbook exercises, or writing. Every appointment, every infusion, every day sat in bed unable to move. In one sense, it gave me a purpose at a time in life when a lot of things didn’t seem to be going my well.
When I was diagnosed with Crohn’s disease at the age of 14, I was just about to embark on the final two years of secondary school here in the UK, where I would complete my first set of important exams, known as GCSEs. At the time, I wanted to become a science teacher, and so I knew it was essential for me to do well in my exams. Everyone kept telling me that I would pass, but being the perfectionist I am, I didn’t want to just ‘pass’ – I wanted to ‘the best’. Others often assumed that because of my health problems, getting a ‘pass’ would be ‘amazing’. This was often well intended but came across as a little patronising. I asked myself why should I achieve less than what I am capable of, just because of my health? It was this mindset which pushed me through. Don’t get me wrong – the stress of the exams in their own right, plus the stress I placed myself under, wasn’t helpful towards my health, and a regular pattern around exams would be a flare-up of symptoms. The same went for my A-Levels, the qualifications required for most University courses.
Over time, I tried my best to develop strategies to help to me manage my stress, while making sure everything was in place to help me achieve my potential without being at a disadvantage from my health conditions. It is often easier said than done, but planning has been fundamental to me limiting the stress I’ve found myself under while studying. In practice, this meant keeping on top of work, writing up notes as soon as possible, and looking ahead at what needed to be done by when. I also made sure that my school and college were fully aware of my health conditions, and that I had access to all the support I needed. This included extra time and the option of rest breaks in exams if needed, as well as being in a room away from the main exam hall that was near to an accessible toilet. Nowadays, with increasing use of technology, I would hope it is easier for students to keep in closer contact with their teachers/tutors, as well as be able to access different pieces of work electronically. This was starting to happen when I was at college between 2010 and 2012, but a lot has changed since then!
“It always seems impossible until it’s done.”
I started University in September 2012, originally studying Biology with a view to becoming a science teacher. I had toyed with the idea of studying Medicine, but I came to the decision that it wasn’t for me at the time. Sometimes I wish I had pursued the Medicine route, but I’ve certainly no regrets. After one year of Biology, I decided to focus my degree on Biomedical Sciences. It was during this period that I began my patient advocacy journey and found my love for research. Inevitably, the first few years of my degree involved quite a lot of work in the labs, which I thoroughly enjoyed and found fascinating. However, on a number of occasions, I did have some issues. While experiencing flares with both my Crohn’s disease and arthritis, in addition to experiencing quite severe cramps and pain while also in remission, I found it challenging to be on my feet constantly while performing tests in the lab. I always had a lab chair nearby, but it wasn’t always practical to be sat down. There were many times when I would be wishing for time to pass quickly so I could get my work done and sit down to get some relief. These experiences helped me to decide that being in the lab 24/7 in the future wouldn’t be for me, despite my love for science and research. Thankfully during my third year, I spent a year on secondment with a pharmaceutical agency, where I was able to use my knowledge and love of science in a way to inform medical communications and the drug development process. Like most things in life, you learn along the journey… coming across the things you least expected doing that you learn to love the most.
While I loved my time at university, I certainly wouldn’t want to repeat the undergraduate degree process! While it was worthwhile and an incredible experience, it was demanding. Thankfully, I graduated in 2016 with a first-class degree.
I then found myself at another crossroad. Do I take a graduate job and leave studying behind, or do I go on to do a PhD? Most people tend to undertake a Master’s degree before a PhD… but I guess I’m not most people. I came across a three-year funded PhD place in healthcare, focussed on supporting children with long-term conditions. I felt as though it was screaming out to me, ‘please apply!’ I decided that I would only apply for this PhD, and if I didn’t get it, then I’d look for a graduate job. I genuinely didn’t believe I would do, but with some luck, I received that wonderful call on Thursday 9th June 2016 – the afternoon after delivering a talk at the European Rheumatology Congress in London. I couldn’t believe my luck!
Fast forward nearly four years, and I am near the very end of my PhD – writing up my PhD thesis on a topic that is so close to my heart – supporting young people with juvenile idiopathic arthritis and their families to manage their health and wellbeing. It’s like a dream. The PhD study experience has been a very different one to everything before. Unlike school, college and an undergraduate Bachelor’s to a degree, a PhD doesn’t feel like ‘studying’. It certainly feels more like a working job, but one where you’re wandering around in the dark. It’s also quite an isolating and lonely journey, though I have been blessed with wonderful supervisors, supportive colleagues, and great friends and family.
As I’m writing up my 80,000 to 100,000-word PhD thesis (yes, I know, it’s going to be a book!), I’ve been doing an awful lot of reflecting, thinking about what worked well, what didn’t work well, and what I would do differently if I was to repeat the PhD again, or do another PhD… which I can guarantee is not going to happen! During this thought process, I feel blessed to have been given the opportunities that I have received over the years, but I also acknowledge that the majority of those achievements have been down to guts and perseverance – and I should be proud of that.
Sadly, it has also highlighted many of the cracks where people with chronic conditions fall through along the academic journey – and how attitudes and practices need to change so that others aren’t discriminated against by an ableist culture which doesn’t recognise and support people of all backgrounds to achieve their goals. We can do this by speaking up, highlighting our needs, and making sure others support us in doing what is needed. Never feel as though you are making a nuisance of yourself, or that you are demanding unachievable things – and if you are made to feel like this, don’t give up, seek support, and fight for what you are entitled to.
What have you experienced as an IBD patient because of the pandemic?
Photo by Bruno Cervera from Pexels
Today the Crohn’s and Colitis Young Adult Fellows joined together to share what they’ve experienced as an IBD patient during this global pandemic. So we asked our fellows how they have been affected by the pandemic as IBD patients and this is what they want to tell you!
“Thankfully, I’ve not had too many problems during the pandemic. My IBD is relatively well controlled at the moment, but I still fall in the group of people in England who are strongly recommended to stay at home, because I am immunosuppressed. Therefore, I haven’t taken any chances. I was able to get my medications delivered to the house, and I now have weekly food deliveries too - though trying to get a slot is harder than you think! My regular follow-up appointments at the hospital have been cancelled until further notice, but I am doing okay at the moment so there’s no need for their input. I have the IBD helpline and email address should I need them - but hopefully not! The only other problem I’ve had is arranging for my three-monthly vitamin B12 injection, which I’ve had for around 10 years due to malabsorption. My surgery has deemed this ‘non-essential’, and are only injecting those with consistently low levels. Clearly, I don’t fall in that category, because I’ve been on regular treatment for so long. They have suggested oral supplements which I would need to buy myself, but the problem of malabsorption - so the supplements are unlikely to be of any benefit.”
Simon Stones
“Though I am not on any immunosuppressive medication, I have felt heightened awareness of the fact that I have an autoimmune disease and an overactive immune system in general. When I realized how serious the pandemic was, my anxiety spiked not only because of the reality that was to come but regarding how many people dismissed the repercussions of proper, careful social distancing or #stayinghome. I was lucky that I was able to communicate with my GI provider and get refills of medications I use during flares and on a regular basis without having a last-minute visit. I only leave my house for essential needs such as groceries (once per week max), prescriptions or to get out of the house to exercise so I can regroup physically and mentally.”
Rachael Whittemore
“As someone who is immunosuppressed, I have been experiencing heightened anxiety because of the pandemic. I have been fortunate to work from home and have the privilege of having family nearby that can transport my groceries to me, but that being said, I still feel the fear and frustration upon seeing the news every day and knowing that there are many people who are not taking this as seriously as I feel they should. I began isolating before the quarantine was in full swing, because of my compromised immune system, and have only been in public to go to the pharmacy drive-in (while wearing a mask of course!). I am trying to channel my anxiety into healthy outlets, such as my art, to avoid prompting a stress-induced flare. All I feel that I can do at this time is stay at home.”
Lucy Laube
“As someone with IBD who’s living in a developing country, the major challenges stem from the lack of robust health infrastructure. Thankfully, I’m not in a flare and neither am I on any medication. However, I do have an ileostomy which requires constant maintenance. I have been facing difficulties in acquiring bags and other components of my ostomy. Luckily, I was able to procure a small amount of these components before the lockdown, but at an inflated rate. I’m also having difficulties procuring basic things like cotton and micropore tape. This keeps me in a constant state of anxiety. I am constantly checking apps to see if I can get the essentials at reasonable rates. Additionally, there is no easy access to any form of basic healthcare in case of an emergency, and that makes me nervous.”
Nikhil Jayswal
“To already live in a body and in a life that inherently holds so much unknown and vulnerability when it comes to my health, and to have that sense of uncertainty that constantly exists within myself now amplified throughout the world, to have that unknown intensified to this extent, has brought even more challenges and emotions to the surface. It feels like the unpredictability that comes with living life with a chronic illness has multiplied tenfold. I am immunosuppressed, and the only time I have gone anywhere except for my house or my backyard was to get blood work taken to check on my levels. While every precaution was taken in doing so, and it is a privilege to have such access, it was still an anxiety-ridden experience. I am incredibly grateful that I am not currently flaring and that I have the ability to be in contact with my GI provider through telehealth services, but I think it’s important for people to realize that IBD doesn’t just “stop” or “slow down” during a pandemic.”
Rachel Straining
“As someone who is immmunocompromised due to the medications I am on, I am always cautious of when I go out and am in large groups of people. With the pandemic, this caution has increased tenfold. I am fortunate enough to be staying with my parents right now. They go grocery shopping so that I do not have to go to the stores. I limit the number of places I have to go. When I do go out, I wear masks and gloves. I come home and immediately put my clothes in the washer and take a shower. I sanitize everything that I buy. When I’ve had to go for my infusions, I have to go through multiple check points to ensure I do not have the virus. All of my doctor appointments have been virtual. Although my health is not perfect right now, I am thankful to not be flaring like I was at this point last year, as I was in the ER every couple weeks. While the rest of the world seems to want to jump into reopening, I get anxious thinking about the ramifications of opening too soon. I cannot control how anyone else responds to this and who follows quarantine and who does not. But I can continue to do my part and stay at home.”
Samantha Rzany
“When you live with a chronic illness, you’re often forced to make compromises for your health. You have to take on a second job as the captain of your health. Since the pandemic began, navigating the healthcare system has become more difficult and uncertain. Chaos is a part of any illness that remits and flares, but when chaos is the defining state of the global world, it can cause undue stress. Personally, I’ve had to postpone doctor’s appointments, and alter my treatment plan to cope with our new reality. It’s been difficult to choose not to participate in activities I enjoy doing, like socializing with friends, but I know that I have to make sacrifices to protect my health and the lives of others. While I cannot eliminate all risk, I am trying to minimize my stress and focus on what I can control. I am taking precautions, such as wearing a mask, and going out for only essential needs. The entire experience of the past few months has brought health to the forefront of the public’s attention. I am hopeful that it will improve the public discourse on chronic illness, and lead to more resources in the health sphere. After all, public health is a collaborative effort, and not an individualistic one.”
Grady Stewart
As someone who is immunocomproised, I carry around the stress of potential sickness anxiety with me. Before the pandemic, I have always been transparent with people in my life about my need for them to stay clear of me if they are not feeling well . This advocacy that I was working on getting good at is now amplified x3. My remicade appointments have carried on, first I couldn’t bring anyone now I am allowed to and it’s back to normal. I feel isolated and lonely but thankful for my roommates who keep me company and my cousin who drives me to the grocery store. For me, it has been a major trigger to have the topic of conversation constantly be of health and healthcare. My hope is that this will bring a new normal. That together we can collectively make workplaces schools etc more accessible for all and that there is now a general awareness and understanding for the immunocompromised community.
Amy Weider
Reflections on Being Diagnosed with a Chronic Illness as a Child
By Leah Clark
When I was twelve years old, I was diagnosed with Crohn’s disease. From personal experience, I believe that being diagnosed at a young age can be seen as a blessing and a curse. Of course I am partially biased; I don’t want to go through my life wishing that I had been diagnosed at a later age. There is literally nothing that can be done to change that. With that, let’s start with the bad news about being young and diagnosed with a chronic illness. At the time, I didn’t fully understand what what was going on half the time. I remember feeling healthy, and then all of a sudden, I was feeling awful all the time. I would could home from school exhausted; I barely ate anything because everything made my stomach hurt. It wasn’t like a normal cold with the sniffles and running nose. That I could recognize, but these new painful experiences were different, and I didn’t know what was going on until I finally went to the doctor.
Reflecting now, I realize what else was going on, apart from getting Crohn’s disease. Part of my childhood was taken away from me, and that’s a pretty big statement. A part of my childhood was not lived because I was too sick to live it. While other kids my age were able to go to pizza parties and stay up late at sleepovers, I literally was too exhausted to keep up. Along with Crohn’s, I was also diagnosed with Celiac disease, so I can’t eat gluten anymore. Not only was I that sick pale girl with bathroom problems, I also couldn’t eat half of the diet a normal child eats. No chicken nuggets and pizza rolls. I had to bring my own snacks when it was someone’s birthday at school. This was also a time before the gluten free diet fads exploded the industry, so there were not many options for me that didn’t include basic foods. You never realize how integral food is in American culture until you can’t eat it anymore.
“A part of my childhood was not lived because I was too sick to live it.”
Aside from missing out on those experiences, I also missed out on social and developmental aspects. For example, in my middle school, there were a lot of tall, athletic girls and boys that participated in volleyball, basketball, tennis, track, cross country, so on and so on throughout the year. Sure, middle school sports aren’t really that much in terms of importance, but at that age, sports signified a time to spend two hours with your friends outside of the classroom. I wanted to be part of that. I didn’t want to miss out on what my friends talked about, who they were talking to, all the hot gossip. You know, typical middle school things. However, I was not good at sports, like, at all. While all my other friends were growing up, getting taller and having fun actually being good at sports, I was not. I was malnourished for so long that I skipped that part of purperty. In fact, I’m still the same height that I was in 8th grade, 5’2. Maybe this is why I don’t like participating in sports even to this day. I feel like I don’t “fit in” in the activity, and I sometimes still get angry that I can’t be better at them.
Anyways, the point I’m trying to make is not that I was bad at sports when I was younger, or that I couldn’t eat birthday cake with everyone. The point I’m trying to make is that I was deprived of childhood experiences that I would consider vital in growing up. Some days, I wish that I had a different childhood; I wish I wasn’t diagnosed when I was so young. It brought not only sadness into my life, but a lot of anger, for a long time. I was forced to grow up faster than my classmates. Heck, I understood how healthcare worked at the age of 14. But, it’s frustrating to be a child and not understand why bad things are happening to you for no reason. For awhile, I felt like I was being punished for something. Why do bad things happen to a good people? Am I a bad person? It took so long for me to realize that sometimes, life sucks, and sometimes good people get sick.
The picture on the left is my 6th grade school photo. My face was thin. I hated smiling. I felt like a ghost being trapped in a body I didn’t recognize. The picture on the right was taken this summer, almost ten years after the other. It’s safe to say I don’t feel that way anymore.
That being said, being diagnosed at a young age was also a blessing in disguise because I was an impressionable pre-teen and able to adapt to my new lifestyle of having a chronic illness in the same way I adapted to other major changes in my life (puperty, middle school, etc). I thought of it as, “Well, I guess this is a thing now,” and I just accepted it as my new life. It wasn’t until later when I would look back on my life that I realized I had experienced some pretty tough things. Of course, I didn’t love it at the time. Who would love having to explain to all your classmates why your face looks like an inflated balloon from prednisone? Or why you have to skip school to go to the doctor’s office for infusions every few weeks? I was lucky enough to go into remission fairly quickly after diagnosis, and (most) classmates did not even discuss my disease with me because it wasn’t affecting my day to day life. I have spent almost half of my entire life living with Crohn’s disease. I know tricks to help with flares. I’ve had years of experience in learning what foods affect my body. Yes, it has been a learning process, but as I grow older, I will be gaining more and more knowledge on how to handle my disease. I learn more about myself and what kind of person I want to be everyday. These experiences, though rough, have shaped me into the person I am today.
I was able to adapt to my new lifestyle of having a chronic illness in the same way I adapted to other changes in my life. I thought of it as, “Well, I guess this is a thing now,” and I accepted it as my new life.
The one thing about being diagnosed at a young age that outshines all the rest is the fact that I have met so many wonderful people with the same disease as me. I was diagnosed in the summer of 2009, and that same summer was the year my parents sent me to a summer camp for kids with inflammatory bowel diseases. I was a camper there every year from then on for six years and was fortunate enough to be a counselor for four years after. It was such a joy to meet kids my age that knew exactly what I was dealing with. We were able to share stories, give eachother advice on how to handle our illnesses, and just spend a week being a “normal” camper. I am happy to have been diagnosed at a young age, because I was able to meet other kids that were diagnosed at a young age, too. It’s a special bond. I have made lasting friendships with mnay people, and it has been an amazing journey. I understand not everyone diagnosed at a young age was able to meet people their age with their illness. IBD can be a very isolating disease, but the thing I find to be one of the best things about my illness is the community established from it. A good support system can honestly be the difference in someone’s life that changes how they look at their disease. I know for me, just the fact of knowing there were other kids like me, helped me so much with my when I was younger.
If I could give just one piece of advice to someone with IBD, it would be to establish a support system. If you haven’t met anyone that has IBD, I encourage you to seek them out. Whether that be a club on your college campus, a support group in your town, or even online, meeting other people will similiar experiences with you can be se rewarding. I was fortunate enough to establish these relationships at such a young age, and for that, I am grateful to have been diagnosed with my chronic illness as a child.
New Year's Resolutions from a Fellow Crohnie
By Erin Ard
Living a life with inflammatory bowel disease is in one word, unpredictable. For Crohn's disease, you pretty much do what you can to control the inflammation in your body by controlling your food intake and working with your gastroenterologist on what treatment methods to use. Not to mention, dealing with any other additional complications or side effects. I was diagnosed with Crohn's disease 10 years ago now and I've learned a lot about strength, resiliency, and the imperfection of the human body. Since my diagnosis, I've learned a lot about my body and my disease including how to accept all of its flaws. But because reality tells me I will deal with this disease for the rest of my life, my journey with Crohn’s is not over yet so there is still so much more to learn.
My journey with Crohn's started back in high school and honestly, I had no idea what would be in store for me. When I was finally sent to see a specialist, we would drive over an hour to my gastroenterology appointments. I started out taking mercaptopurine to suppress my immune system but quickly advanced to Remicade as a long-term treatment. On Remicade, I finally felt like myself again – at least a version of myself with additional manifestations of my Crohn's. The joint pain and short-lived fevers still persist, even today. It has been 8 years since I started on Remicade and a lot has happened over those years. I finished high school, moved away from home, and started college at the University of Wisconsin - Madison. Since starting college I've learned a lot more about myself as an individual and how Crohn's affects my life as a whole. In fact, it has changed since I was diagnosed and achieved remission the first time around.
I moved through the years mostly symptom-free. With only the rare stomach ache, but still able to maintain your daily routines. I knew precisely how my daily life would change if my disease was active. I valued the time I had thinking I could eat what I wanted without repercussion or go on a long run without my joint pain forcing me to limp the remaining distance. When your Crohn's is in remission, you have the freedom to eat delicious - maybe not so Crohn's-compliant - foods. You may even plan travel trips into your year with minimized anxiety of having an episode. I had the freedom to do all of these things! Since 2019 started, I tackled my vision board ideas by cooking more from scratch, trying out healthy recipes in my Insta Pot, and booking my first flight on a plane! Followed by several more flights to exciting new locations I hadn’t dreamed of experiencing because of the travel-anxiety instilled by my Crohn’s. For a woman in her early 20s with Crohn’s disease, I was crushing it! Then a few reality checks later, the unpredictability of IBD set in and I learned an important lesson. That no matter how far into remission you've gotten, odds are you might flare-up again in the future.
Photo by Evie Shaffer from Pexels
This sad truth is where I found myself recently. For the last few months, I've felt pretty off. I was getting more frequent belly pains, indigestion, irregular bowel movements, and my joints were starting to bother me more. I had originally attributed all of my symptoms to not eating well, which was a naïve thing to believe.. In retrospect, I had been struggling to stay in remission for the past couple of years. With the way that Remicade infusions worked over my 8 week time period, I would started getting symptoms again around week 7. That last week was a familiar struggle which included neglecting some of my responsibilities at school. I would end up skipping a class here or calling into work there - each pretty understandable given the circumstances but I still regretted having to do. About a year ago I went in for another colonoscopy (my third so far) because of these recurring symptoms and because my last one was towards the beginning of my diagnosis. The results didn't come back perfect, of course. They found some inflammation in my distal colon and the opening to my small intestine, which would explain my irregularity, stomach pain, and indigestion. I was told my gastroenterologist would be in touch to discuss what my next steps would be. After that visit, everything concerning my disease went on hold for awhile. In other words, life happened. My obligations for school and work started to take over my free time. Being the Crohnie I am, my limited will power from the fatigue would have me put the small tasks off until the following day. Meaning my health was put on a back-burner because they would always be put off until the “next day.” I was still receiving infusions every 8 weeks and conquering through my days, so I didn’t jeopardize my self-efficacy. I felt able to accomplish whatever I set my mind on. Eventually I started to wonder what my prognosis would turn into if I continued living this way. So I finally scheduled that appointment, this time with the gastroenterologist that performed my last colonoscopy.
Since I've started this fellowship with #CCYAN - the Crohn's and Colitis Young Adults Network, I've read so much about other people's experience and learned the expansive symptomology of inflammatory bowel disease in other bodies. Since the start of the year I realized how crucial it is to maintain your disease to prevent complications or necessary surgery in the future. Heading into the new year, my new outlook will be focused on achieving remission and maintaining a healthy body, any way I can. Let me share with you what my Crohn’s-related New Year’s resolutions are for 2020..
Learn to accept the unpredictable.
The first resolution I’d like to explore more is in how I think. Because Crohn’s can be so unpredictable, accepting this as a fact of the disease may help uncontrollable events feel less traumatizing. When you can learn to seek solutions or simply see the positive rather drowning in the self pity, loathing, disgust or whatever you might feel, you will feel a bit more at ease. It takes so much energy worrying about what "could" happen in the future. Like what "might" happen if you venture away from the privacy of your home and go to the movies today. Or "if" you might have the urge to go on an airplane while the bathroom is busy. Or "if" you don't make it to the toilet on time. Events like these are bound to happen and throw you for a loop if you aren't prepared. I should clarify that learning to how to accept and not worry about the future doesn't necessarily mean you shouldn't prepare for anything and everything. Because the first thing we all learn with IBD is that preparation is key to surviving any traumatic bathroom incident!
To take initiative when it comes to my well-being and body's health.
The second resolution involves how take action when Crohn’s is clearly affecting my body. My bad habits of binge-eating sugary treats or ordering high-fat take-out when I’m not feeling well starts to become routine when I don’t take responsibility for some of the fall out. I’d like to learn how to better take initiative to prevent consequences or make the most of my recovery. This means staying in close contact with my gastroenterologist about any trouble I’m having, not eating foods I know will quarantine me in the bathroom the next day, and keeping track of my symptoms, as tedious as that might be.
Recently I received not-so-great news from my gastroenterologist and it felt like my world was collapsing. After I took a calprotectin test which showed an adequate amount of inflammation, she told me that my Crohn's was flaring up again. It took me a bit to realize that what I was experiencing was actually long-lived. I had started getting symptoms months prior and it took me too long to get back on track. Something simple that could have helped me notice something sooner would have been a food log, which unfortunately, I don't have a lot of experience in carrying out. However, I do see their value and hope that this next year I can explore this path and hone in on what my exact food triggers are and how my body changes throughout the year. If you are now interested in doing the same, see this article on How to Use a Food Diary to Help Manage Crohn’s Symptoms and Flares from Everyday Health. I might not go as far as weighing my food, but at least I will get an idea of what food leads to which symptom.
My disease will change as much as I do.
This is one thing I needed to accept my disease started to flare up again. I was caught up in the idea that I had achieved remission and that everything would stay relatively constant. I just couldn’t see myself going through what I had in high school again, when my Crohn’s had surfaced. Since then it’s been a constant flow and I tried to push any thought that the disease would hold me back aside - which was an advantage for the time-being. However, this also kept me from growing because I just shut everything out. I wasn’t able to harness the power of vulnerability in having an illness to accept myself as I am and love my body.
After spending the last 8+ years in remission, with only some minor episodes, finding out my disease was flaring up again came as a shock to me. I've noticed that I'm the type of person who is apprehensive around big life changes. I like how things are going, I am comfortable with how everything is, and if I have to suffer through it a little, I am fine with that. However, this kind of mindset wouldn't suffice anymore and I've been realizing that more and more every day. My doctor and I have been working hard to put my disease back into remission. I'm trying some new medication out and taking everything new in day by day. IBD is so specific to every person, so how it presents itself or progresses is going to look different in all of us. And as all of us grow into young adults and beyond, our disease will change over time as well. For the better, or not so much.
My body will do some weird things, just learn to go with it.
You would think having to deal with gut pain would be enough, but there are so many other things that can factor in! The most common list of symptoms for Crohn's disease include abdominal pain, diarrhea, and fatigue. But the lesser known, indirectly related symptoms should also include weird noises, smells, urgency and accidents. Your gut will make loud gas-y noises while it’s quiet in the office. You will have to take frequent, unexpected breaks when the urgency gets the better of you. And the unfortunate reality is that sometimes, you won't make it to the bathroom in time.
The most healing part of my being more vulnerable this past year, was accepting these symptoms as they were instead of trying to control them. Because when I’d try to control them, I would get gut upset, constipation, or even more uncomfortable. I eventually started to tell people that yes, I have had accidents in the past and brushed this confession off like it was normal. Humor always goes a long way in these situations. Because of the healing I’ve already had, I want to pursue this resolution in 2020 as well to see my body’s flaws in a new light.
My hope is that you will find some inspiration to create your own list of resolutions for yourself. Whether they are similar to mine or completely different! Join me in making a resolution list for yourself this year and we can both actively improve our life with IBD together!
Doing the imPOSSIBLE while living with IBD
By Andi Nowakowski
Limitations and sacrifice are an unfortunate aspect of living with a chronic condition, which is why I was very excited when, this summer, I was able to take part in an activity I’ve been wanting to do for a long time; I donated blood.
It may not sound like much, but between the numerous immunosuppressants I take on a daily basis, my Crohn’s disease diagnosis and all the issues that are in tandem with IBD, I didn’t know if this was a donation I would ever be able to make. Even so, when the company I was interning with over the summer announced it was hosting a blood drive, I decided to do some research and was surprised to find that I would likely be able to contribute!
Whew! This experience was a rewarding mix of anxiety and exhilaration. The day of the blood drive arrived, and I was asked to fill out a survey that included questions about my age, weight, specific medication use, surgeries, etc. They checked my vitals and iron levels and deduced that I was a good candidate to donate. The only thing left to do was sit down and give over some of my life-saving bodily fluids-- an accomplishment I have been dreaming about for years.
The nurse warned me to look away as she was about to place the needle, advice that, as a professional patient, I flippantly dismissed. Being an IBD patient, I am used to being poked and prodded with needles. Let me tell ya, that needle was MUCH larger than I anticipated. A word to the wise, if you have a fear of needles, you may want to keep your eyes averted at all costs should you decide to donate. In the end, it took about 15 minutes. They took a pint of blood while I sat in a reclining chair and enjoyed a well-earned snack. I was shocked at the amount of blood they drained out of me. Turns out, the average person has about 10-12 pints of blood in circulation but only needs about 8 to function normally. Honestly, though, I was really proud of myself for taking on this challenge and pushing my own limits.
Donating blood is a thankless, but worthwhile task. The person who will ultimately end up receiving your blood will never know who you are, but it is a life-saving and meaningful endeavor. For many, donating blood is a routine measure and most people probably don’t think twice about it, but for me, it was a way of giving back a little bit of good to the world. It was my way of saying, “Screw you Crohn’s.” It was my silent triumph against IBD and the limitations that come with it. The goal of this article is not to persuade you to go out and donate blood. I will say that it was physically challenging for me to do so. That being said, I do hope to inspire you to push yourself and seek out the endless possibilities that this world has to offer. Be patient with yourself and your condition, but don’t let IBD stop you from pursuing your dreams. Allow your experiences to strengthen your resolve and keep challenging yourself to experience all that you can.
As one of our founders, the late Cory Lane, used to say, “live each day like an adventure.”
Andi