NEWS
HealtheVoices 2025: Feeling Beautifully at Home with my IBD
by Michelle Garber (California, U.S.A.)
Disclaimer from Michelle: Johnson & Johnson paid for my travel expenses to attend HealtheVoices, but all thoughts and opinions expressed here are my own. This conference was not attended as a part of the CCYAN fellowship.
From November 6th through November 9th, 2025, I stepped into a space that I had never experienced before. HealtheVoices 2025 was more than a conference for advocates like me. HealtheVoices became a place where my body, story, and heart finally felt understood. I walked in as an Inflammatory Bowel Disease (IBD) and mental health advocate, but I walked out feeling like I had reclaimed parts of myself that IBD had slowly worn down.
IBD affects so much more than the digestive system. My life is shaped by symptoms that are unpredictable and exhausting, with my mental health experiences running parallel to this journey and adding additional weight. IBD ultimately shapes the way that I move through the world, my energy, my confidence, and even the level of honesty that I bring to conversations. Daily life can feel even more heavy and lonely because it is rare for me to be in a room filled with people who truly understand what chronic illness feels like, and vulnerability about illness does not always land well with people who cannot relate. At HealtheVoices, that weight softened the very moment that I arrived. The environment made me feel safe before I even realized that I had been holding my breath for so long.
I met people living with many types of chronic conditions, from visible disabilities to more silent illnesses like mine. I met caregivers who understood illness from the position of love and exhaustion. I met people who shared my diagnosis of IBD and people who shared my mental health struggles as well. In turn, I finally did not feel like the odd one out or like the only person in the room fighting a battle that no one else could see. For one weekend, I felt truly seen, understood, and supported. It felt like everyone there spoke a language that I always knew but rarely had spoken back to me. It was a rare and profound reminder that community, safety, and understanding can change the way a chronically ill body feels because, to put it simply, I finally felt normal.
While I cannot speak for all of the attendees, I know that I felt this way for a variety of reasons, and I am going to try my best to put it into words.
For starters, I could tell that the conference itself was intentionally designed with us in mind, and that intention showed in every detail. Organizers checked-in on us often, encouraged rest, and made it clear that nothing was mandatory. They understood that rest is both a need and a responsibility. They understood that pushing too hard could cause flare ups, particularly for those of us with IBD or conditions that involve fatigue, pain, and unpredictable symptoms. Even travel was supported as I received reminders and check-ins to make sure that I made it to my flight safely. This took the emotional labor out of the small things that usually drain me, and their help and accommodations were never made to feel like favors. Plus, everything was optional, yet everything was thoughtfully provided. It was all offered with genuine care, and that is something that I rarely feel in spaces outside the chronic illness community. I truly felt taken care of at every moment. I never felt pressured to show up to an event, and I never felt like a burden or a "waste of an attendee" if I did not. I felt valued simply because of who I am, IBD and all. Typically, I am made to feel as though my IBD devalues me throughout many domains of life, but I felt the opposite way while at HealtheVoices. I also felt considered and looked out for without being pitied or restricted. In other words, I felt empowered to take care of myself and to be the advocate I want to be, while also realizing that there is power in accepting help and care—there is the "power of us."
Regarding this "power of us," I was able to witness and experience how chronic illness can foster unity, even when diagnoses and symptoms may differ. This was exhibited right off-the-bat at the very first dinner of the conference when attendees were grouped based on their health condition, and I accidentally sat with the mental health and pulmonary hypertension group instead of the immunology group. What started as an awkward mistake due to my brain fog after a long day of traveling ended up turning into a gift. At this dinner, I connected with people who understood my mental health story in ways that felt grounding and familiar. Some even worked in the mental health field like I do, which felt incredibly validating. Therefore, even though not a single individual there had IBD, our emotional landscapes were still strikingly similar. We each shared our stories of career challenges, burnout, medical dismissal, discrimination, chronic pain, hospital admissions, fatigue, chosen family, the exhaustion of being misunderstood, and the emotional toll of navigating life and relationships with an unpredictable body and/or mind. We also connected over experiences specific to gender, such as being dismissed in medical settings until a male caregiver shows up.
These discussions reminded me that chronic illness is not defined only by biology. It is shaped by stigma, gender, identity, socioeconomic realities, and the emotional toll of constantly having to justify our experiences. Even people whose conditions had nothing in common with mine understood the same nuances of fatigue, pain, fear, and perseverance. Our hearts carried extremely similar stories, and the overlap was both comforting and heart-wrenching at the same time.
After that realization, I made a conscious effort for the rest of the weekend to approach people without looking at their badges. I did not want to lead with diagnoses anymore since I understood that a diagnosis was not the only thing that could foster deep connections. I wanted to understand people for who they were rather than for what condition they advocated for, even though I understood that advocacy often played a large role in the attendees' identities.
Despite it being an advocacy conference, my goal was not to advocate or educate that weekend. I simply wanted honest connection. I wanted to feel safe being myself. I wanted to meet people who would understand both the heaviness and the humor that come with living in a body that needs extra care and requires constant negotiation, without limiting myself by my diagnosis. My IBD has limited me enough already, and I was not going to let it stop me from making the meaningful connections that I have been seeking just because of a label. As it is, living with IBD and mental health challenges is incredibly isolating, especially when daily experiences and honesty are treated as oversharing. Everyone, including myself, preaches vulnerability, but it is difficult to be vulnerable when people do not know how to respond or cannot relate to your daily reality. That is why having the space to openly share about your day-to-day life—without the sugarcoating—is essential, and I found that space with each and every attendee carrying all of the diagnoses under the sun. It did not matter if they had IBD, a different chronic illness, or if they were a caregiver since we could all relate to one another in some way.
This was an incredible phenomenon that attendees and I noticed since at HealtheVoices, we did not have to explain the basics. Each conversation started with an innate understanding of one another. This understanding was not just based in compassion and shared experiences as it was oftentimes also based in shared medical knowledge/terminology, tips and tricks for navigating the healthcare system, etc. This is because everyone there lived some version of the same complexity. For example, many of the attendees understood Prednisone's mental and emotional side effects, sometimes even making light of it nonchalantly during conversations. Outside of the chronic illness space, these jokes and statements would have to be explained or given some background information, which can become exhausting over time, especially as you meet more people throughout your life. Having people who just "get" certain things—without needing to pause the conversation to explain and without having to worry about how it might be taken—is a breath of fresh air.
I did not have to soften the truth or worry about being labeled as "dramatic" or "negative." I did not have to explain why I left an event early or arrived late, nor did I have to explain why I did not finish the food on my plate. People just got it. This conference felt like a safe haven where I did not have to justify my needs or my existence as someone living with IBD. Even when we were not familiar with aspects of each other's health condition(s), we approached one another with curiosity rather than making assumptions, offering unsolicited medical advice or "natural remedies" that we have likely already tried/been advised to try countless times, or making remarks along the lines of, "everything happens for a reason" and "at least it's not cancer."
Conversations were honest but never forced, and I found that our weekend did not revolve entirely around illness. Sure, we cried a lot, but we also laughed a lot. We talked about hobbies, goals, spirituality, tarot, and things that were not centered in our diagnoses. It felt balanced in a way that my everyday life rarely does since either my whole world feels tied to my IBD, or I attempt to live in denial of its existence. At HealtheVoices, I did not have to shrink or edit my truth.
Yet, there was a moment very early into the weekend when I felt myself growing emotionally tired. While there were those intriguing conversations outside of chronic illness, most conversations were still deep and personal in nature. As a result, I felt an unexpected countertransference building inside of me, as if I had automatically tried to become the "listener" and "helper." Hearing such heavy stories that mirrored my own felt draining at first because I empathized deeply, and I wanted to hold people's burdens for them for as long as I could. That is what I am used to doing for others, and that is what I honestly enjoy doing. I see it as a privilege to be trusted with such personal information and stories of deep pain. Thus, I wanted to show my gratitude for this privilege, which expressed itself as me unconsciously attempting to relieve some of their burdens. It was as if I had naturally tried to step into the role of "therapist" instead of simply being myself. It is a habit that comes naturally to me, especially since I am entering the mental health field as a therapist and hope to work with people who have chronic illnesses.
I also initially experienced some imposter syndrome early into the conference. I was surrounded by these incredible advocates, many of whom have been advocating for decades. Some were even making a career out of their advocacy journeys. Even though it feels like IBD has been a part of my identity for my whole life, I was only diagnosed 4.5 years ago. Similarly, even though I feel as though I have been advocating for years, I really have only been actively advocating and becoming involved in the IBD community this past year. This made me begin to question why I was selected to attend the conference. What the heck do I have to offer? The more this question weighed on me, the more I felt the need to make up for my perceived lack of experience. This translated into my attempt to take on that therapeutic role that is all too comfortable because at least I would be offering something.
After a good night's rest that day, I realized something important: I was not there to fix anything, lighten anyone's burden, or carry emotional weight/pain for others. I was there as Michelle, not as a therapist. In fact, nobody there asked or wanted me to show up as a therapist. The fact that I was selected to attend the conference is proof in itself that there is something that I could offer within the advocacy space, even if I am a "newbie." There is something that I could offer by simply being myself, and I was allowed to be myself (whoever that is). Listening deeply is part of who I am, but absorbing others' pain does not have to be. Once I gave myself permission to let go of the helper role and the imposter syndrome while understanding that I could be present without absorbing everything, something inside of me shifted: I started to share and listen without performing emotional labor.
As a result, my body felt lighter. My energy felt different. As someone who lives with IBD and chronic fatigue as a constant companion, I hardly ever feel energized. Yet in that space, surrounded by community and safety, I felt more awake and alive than I have in years. I slept through the night without restlessness or insomnia, and I rested without guilt. That establishment of safety ultimately allowed my body to shift out of survival mode, which is the foundation of many evidence-based theories. I felt at home in a way I did not expect. I finally saw that I was allowed to accept help and let people in, even if they were going through their own struggles. I saw how support can be mutual and balanced. I also saw how I could be the "supported" instead of the "supporter," especially by how the HealtheVoices organizers took care of me without requiring anything in return. Letting myself step into that truth felt like exhaling after years of holding my breath. It felt like the relief that comes from finally unclenching my fists and jaw. It reminded me how much chronic illness is affected by environment and emotional safety because healing is not only medical, but it is also emotional and communal.
Overall, this experience made me realize how rare it is to just feel safe in everyday life. At HealtheVoices, everyone had something, whether it was a chronic illness, a disability, or the role of being a caregiver. Illness was not the exception. Rather, illness was the normal. By that, I mean that caregivers and those with health challenges were not the minority, and we did not feel out of place. That shift in perspective changed how I saw myself as it made me feel entirely human. Despite my symptoms persisting due to their chronic nature, I did not necessarily feel "disabled." I did not feel "different" or "abnormal." I did not feel like my everyday reality was "too heavy" or "too personal" to be shared. It was simply life, and almost everyone there understood.
The environment created at HealtheVoices highlighted a crucial truth: the world can accommodate people living with chronic illness, but spaces simply choose not to. The conference gathered people with vastly different conditions and needs, and yet everyone I met felt included and supported. This was not magic. This was intention. This was care. This was a commitment to treating people with chronic illness as fully human. I felt that my needs mattered and that I mattered. The organizers did not treat accommodations as burdens but rather as standard practice. This was eye opening because many institutions act as if inclusion is too much work, but this conference proved that it is entirely possible. In fact, it showed me that inclusion is completely achievable when people genuinely want to create it. To put it simply, inclusion is a choice. Dismissing people is also a choice. Institutions, workplaces, and communities can make room for us, but they simply choose not to invest in the effort.
I left the conference with a heart full of gratitude for the connections I made, the stories I heard, the jokes I shared, the insights I gained, and the revitalized sense of identity that I fostered. I left with a deeper understanding of caregiver burden and the emotional landscapes of people living with all types of conditions. I left with the lived experience of how community is essential for healing. I left with a reminder to show up authentically, even in spaces that do not always understand. I left with a deeper commitment to advocate for people with IBD and for people living with chronic illness(es) more broadly. I laughed more than I expected to, and I actually felt real joy. I left with the realization that I often carry emotional burdens for others and take on roles that are not mine to hold, and that realization is going to guide how I move forward in my personal and professional life.
Most of all, I left with a renewed determination to push for environments that truly include people with IBD and other chronic conditions. We deserve to feel normal, included, and valued. We are not abnormal. We are simply made to feel that way by systems that refuse to accommodate us. Anyone can become disabled at any time through illness, accident, age, etc. Anyone can become sick. Anyone can get hurt. Everyone ages (or at least that is the end goal). It is easy to not be concerned about something that does not affect you, but take it from me, it is 100% possible to wake up sick one morning and never be able-bodied again. That is the story of many people with IBD and many people with chronic illnesses. Inclusion matters because disability affects all of us eventually. Anyone can shift into the world that I navigate every day. In turn, inclusion genuinely benefits everyone.
All in all, HealtheVoices reminded me that despite my IBD, I am not alone—I never was. It reminded me that there are some spaces where people like me can feel completely safe, completely understood, and completely ourselves. There are places in the world where people with IBD can feel completely and beautifully at home. Being in such a space where chronic illness and disability is the norm shifted my understanding of what it means to feel "normal." It showed me what true accommodation, accessibility, community, and compassion look like. It showed me what is possible when people choose care over convenience. It proved to me that inclusion is not only possible, but it is deeply worthwhile. I will carry that truth with me and continue advocating for a world that chooses to see us, support us, and welcome us as we are. And for that, I will be forever grateful.
The Hidden Struggle: Medication Access and Equality for IBD Patients
by Beamlak Alebel (Addis Ababa, Ethiopia)
Treatment is more than a diagnosis or a prescription — it’s about whether the medicine you need is available, affordable, and within reach. For many IBD patients, that uncertainty becomes a heavy burden. It’s hard to stay strong when your survival depends on something you might not find or afford tomorrow.
For me, the struggle is deeply personal. Every month, when it’s time to get my medication, I feel both guilt and sadness. I can’t ignore the heavy burden it places on my family. Watching my parents worry about how to afford my treatment hurts more than the illness itself, especially since the medicine is rarely available in public hospitals. Even though they never complain and always care for my feelings, I can see the stress in their eyes — the quiet fear of what might happen if one day the medicine becomes too expensive or unavailable. It’s painful to live knowing that your survival is also your family’s financial struggle. I wish the medicine could at least be less expensive and easily accessible everywhere, so no one would have to choose between health and hardship.
The world has powerful medicines with great potency — but what is the use of their strength if only a few can afford them? True progress in healthcare means making effective treatments available and affordable for everyone, not just for those who can pay the high price.
Access to medication is not a privilege; it is a lifeline. Yet in many places, that lifeline is fragile. I have seen patients lose hope — not because their illness defeated them, but because the system failed them. Seeing people treated as if their lives are less valuable simply because they are sick is one of the deepest pains a person can feel. It makes you question your worth. It makes you feel invisible.
But we are not invisible. We are fighters, dreamers, and survivors. Our illnesses may have changed our bodies, but they have not taken away our strength or our right to be seen, respected, and included.
Equality should not only exist in words or promises. It must exist in action — in how policies are written, in how medications are distributed, and in how people with chronic illnesses and disabilities are treated. I know how it feels to be looked at differently, to be judged for something beyond your control. What we have is an illness, not a choice.
Even in schools and health-related fields, there are times when lecturers or professionals do not fully understand what it means to live with a chronic condition. They see our physical state but not the strength it takes to show up, to keep learning, and to keep fighting. Being judged for taking sick leave or missing class because of health reasons can make a person lose hope. For now, we keep silent — but one day, we may speak as a volcano when the time comes. Because silence does not mean weakness; it means patience, and patience has power.
I dream of a world where no one loses hope because of a lack of medicine or misunderstanding — where being different is not a reason for exclusion, and where compassion leads policy and practice. Modern research is advancing, but true progress will come when every patient, everywhere, is valued equally — when access to care and empathy become rights, not struggles.
Advocacy is how we get there. By speaking up, sharing our stories, and reminding the world that every life matters, we turn our pain into purpose. Because in the end, access to medication and equality are not just medical or social issues — they are matters of dignity, compassion, and humanity.
Everything will change one day — the policies, the systems, and the hearts of people. Until then, we keep raising our voices, believing that our struggles today can open doors for those who come after us.
Learning to Complain: A Survival Skill for Chronic Illness
by Akhil Shridhar (India)
For many of us living with IBD, saying “I’m fine” has become a habit, something we were taught to say to avoid worrying others or causing trouble. But managing a chronic condition means we can’t afford silence. Doctors need us to describe what hurts, what’s changed, and what’s not working. At first, that shift feels unnatural. How do you speak up about pain when you’ve spent years trying to hide it? Learning to explain what’s wrong isn’t just about getting better care, it’s about breaking the silence, challenging stigma, and making sure our needs are heard. Speaking up is advocacy, and it starts with learning to complain. Many of us were taught to downplay pain, brushing off discomfort to seem strong.
This kind of silence runs deep, shaped by family, culture, and a society that equates quiet with resilience. But for people living with IBD, staying silent can be dangerous. It leads to delayed care, isolation, and missed warning signs. Although, learning to speak up about symptoms is just a part of it. Especially in developing countries like India, where systems often lack the integration, communication is not just helpful but essential. For most, the responsibility of managing appointments, tracking medical records, logging test results and prescriptions, consulting different specialists, and coordinating insurance doesn’t fall on an organised platform, it falls on the patient.
Living with IBD means your body goes through changes that aren’t always easy to explain. Symptoms come and go, and sometimes they’re hard to put into words, especially if you’ve spent years being told not to make a fuss. When you share what you’re feeling clearly and honestly, you’re helping your doctor understand how to support you better. It’s not complaining, it’s communication. And with a little guidance and the right tools, you can learn to speak the language of your symptoms in a way that leads to real care and understanding.
Doctors rely on clear, consistent information to track how IBD is affecting your body, and that’s where accurate symptom-sharing becomes key. The table below outlines the kinds of details that help build a more accurate picture of your condition.
Living with IBD often means navigating a maze of symptoms, appointments and uncertainty. But the ability to speak clearly and communicate will go a long way in getting the care that we deserve. That’s why this table isn’t just a tool, it can help you bridge the gap between what you feel and what the doctor needs to know. Remember, this guide is meant to serve you, so feel free to adapt it, add to it, and make it your own. Bring it to your appointments, refer to it and use it to shape your care in ways that truly reflect your needs.
This log table is for you to document your symptoms and experiences in a structured manner. Save a copy and take notes or just use it as a reference for your next appointment!
Advocating for IBD
by Lexi Hanson (Missouri, U.S.A.)
Why is IBD Important to Advocate for?
IBD (including Crohn’s disease and ulcerative colitis) affects millions worldwide and can severely impair quality of life.
Often diagnosed in teens and young adults, IBD can affect people during the most critical stages of personal and professional development.
Because IBD involves bowel symptoms, people often avoid talking about it, leading to shame and isolation.
Lasting impacts from IBD
High rates of anxiety and depression are associated with IBD due to its unpredictable nature and social limitations.
IBD leads to significant healthcare costs, lost productivity, and financial strain for individuals.
Access to proper diagnosis, treatment, and ongoing care is not equal across regions and populations.
How can we Advocate?
Share personal stories and facts through social media, blogs, podcasts, and public events (especially during awareness months).
Advocate for policies that ensure better healthcare access, insurance coverage, and medical leave protections for those with chronic illnesses.
Form or join local or online support groups to connect patients, caregivers, and allies.
IBD: I Battle Daily
by Beamlak Alebel (Addis Ababa, Ethiopia)
Living with inflammatory bowel disease (IBD) has taught me an unforgettable truth, that is the battle I face every single day. It is not a one time event or temporary struggle, it is an ongoing challenge that affects every part of who I am. It is not just physical, it is emotional, mental and spiritual. Every decision I make has the power either to support my healing or challenge it.
From my personal journey, I have learned something I believe is absolutely essential for a person living with IBD: understanding our condition is crucial. The more we know about IBD – the symptoms, the triggers, the treatment options – the better prepared we are to manage it with strength and confidence.
But I have also come to realize another powerful truth: what works for me might not work for someone else. Each of our bodies is beautifully unique, and that is why it is so important to slow down, reflect, and truly listen to your body.
IBD is not just about following a set of rules someone else wrote, it is about discovering and honoring your own rhythm.
I once heard my lecturer say, “I ALWAYS STAY ON MY SAFE SIDE.” That one sentence echoes in my mind on tough days. For those of us with IBD, our safe side is not just a place, it is a mindset. It is the knowledge we have gathered, the awareness we have cultivated and developed about our own bodies. Staying on our safe side means respecting our limits and standing strong in what we know helps us.
Let this journey inspire others to do the same. Let it be a reminder that even in the face of invisible battles, we have the strength to rise. Let it encourage every IBD warrior out there to listen closely to their bodies and to honor their unique paths with pride and resilience.
We fight daily not just with medication, but with courage, care, and community.
Image from Unsplash.
One Condition, Two Worlds, Shared Strength: Cross-continent experiences of living with IBD
by Beamlak Alebel & Kaitlyn Niznik
Kaitlyn’s experiences in the United States:
Living with microscopic colitis in the U.S. comes with its own challenges:
Months-long waits between doctor’s appointments
Expensive medications and treatments, especially without strong insurance
Delayed diagnosis despite advanced healthcare systems
Difficulty finding foods that align with dietary needs and aren’t overly processed
Being dismissed by others who don't understand the condition
A painful impact on social life and emotional well-being
Beamlak’s experiences in Ethiopia:
In Ethiopia, living with IBD means facing different (but just as heavy) burdens:
Widespread misconceptions: many believe it’s just stomach pain from bad diet
Medications are not only costly—they’re rarely available
IBD is seen as a disability, making it hard to find work
Employers are hesitant to hire people with chronic illness
Speaking openly often leads to judgment or silent gossip
There’s little public awareness, and support is nearly nonexistent
Surgery and pain are not just physical but emotional struggles too
Isolation is deep, and the future feels uncertain
Chronic illness carries stigma, creating silence and shame
Despite our different realities, our pain, fears, and desire to be understood are the same.
IBD knows no borders.
And neither does our strength.
We’re raising our voices—because IBD is real, painful, and deserves global attention.
By sharing our stories, we break the silence.
By standing together, we make IBD visible.
By speaking out, we show that shame fades when we are heard.
Let’s keep going. For ourselves. For each other. For every IBD warrior around the world.
Battling an invisible illness while everyone else plays “doctor”
by Beamlak Alebel (Addis Ababa, Ethiopia)
Exams are already stressful, but for those of us dealing with invisible illnesses, they can feel like an impossible battle. The pressure to perform, sleepless nights, and depression don't just affect our mind - they also affect our whole body too: and while we struggle through the pain, others think they have all the "expert" answers:
My Brother wonders, "maybe it is some unknown disease science hasn't discovered yet."
My Parents think, "it must be setan (evil spirit), we should take her to holy water."
Society assumes, "it's probably caused by her poor lifestyle or malnutrition."
Meanwhile, I am just trying to survive this exam while everyone else plays doctor.
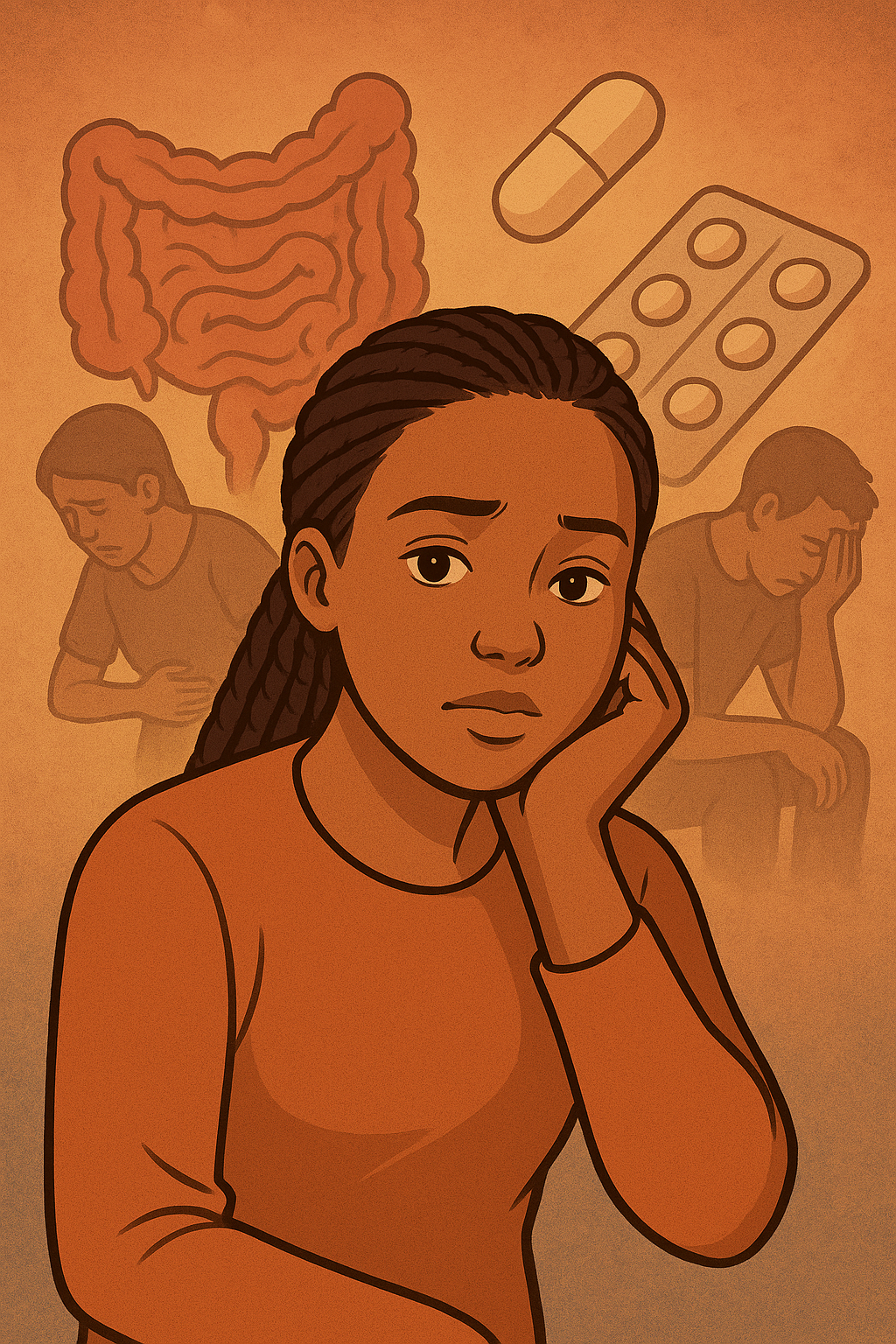
The silent struggle of invisible illness
Living with IBD means battling symptoms that others can't see. It is a constant storm - worsening digestive system, gut motility issues, poor sleep, and one of the biggest triggers, stress.
Exam deadlines and academic pressure can make symptoms flare up. But instead of understanding the real impact of stress on chronic illness, people jump to conclusions. They blame supernatural forces, poor diet, or anything except the real medical condition.
Why awareness really matters
The truth is, many people don't understand invisible illness until they (or someone close to them) are directly affected. This lack of awareness leads to stigma, misdiagnosis, and people suffering in silence. We need more conversations about IBD not just in medical communities, but also in everyday life.
Invisible illnesses like IBD can be incredibly tough. Friends and family should understand that IBD is a serious, life-threatening condition, and many factors outside our control can trigger painful flare-ups. Other people's misconceptions about IBD just add to our stress as patients...so if stress is a known trigger, we need to address these misunderstandings!
This is why it is important to raise awareness, have discussions, and help others recognize the impact that IBD has on us.
Because we know invisible illnesses exist, so why do we keep doubting those who live with them?
Instead of playing doctor, maybe it is time we start listening.
(Image from iStock, credit: nadia_bormotova)
My Journey of Advocacy as an IBD Patient in Africa: A Medical Student's Perspective
By Yeabsira Taye Gurmu, Addis Ababa, Ethiopia
As an IBD patient living in Africa and a medical student preparing to become a doctor, I have come to deeply appreciate the importance of advocacy. Living with a chronic illness can often feel isolating, especially in a context where awareness about conditions like IBD is still developing. Through my own journey, I’ve realized that advocacy is not just about raising awareness; it’s about creating a sense of community and support that can make a significant difference in the lives of those affected by IBD. However, I’ve also learned that it’s crucial to balance this advocacy with my need for personal peace and maintaining my boundaries.
In my efforts to advocate for IBD awareness, I’ve found that it’s essential to be selective about what I share. While my experiences can help others understand the challenges of living with IBD, I’ve recognized that I don’t have to disclose every detail of my journey. Setting clear personal boundaries allows me to engage in advocacy without compromising my emotional well-being. For example, I choose to focus on the broader message of understanding IBD rather than delving into the more painful aspects of my experience. This approach not only protects my mental health but also helps me stay purposeful and impactful in my advocacy work.
I’ve also learned the importance of self-care while engaging in advocacy. It’s vital for me to participate in discussions and support groups at a pace that feels comfortable. Sometimes, this means stepping back and taking time for myself to recharge. I’ve found that when I prioritize my well-being, I can engage more authentically and passionately in my efforts to raise awareness for IBD. Encouraging others to find their own balance has become a priority for me, as advocacy is most effective when it aligns with our personal values and comfort levels.
By sharing my experiences thoughtfully and prioritizing my well-being, I can contribute meaningfully to the conversation around IBD without losing sight of my own needs. As I continue my medical training, I aspire to inspire my peers to embrace the significance of patient-centered advocacy. Each voice is important, and together we can foster a supportive environment that not only raises awareness but also honors the individual experiences of those living with chronic illnesses like IBD.
Featured photo by Steve Johnson on Unsplash.
We are all pandoras, each with our own boxes - but we all have hope.
By Selan Lee from the United Kingdom
Suppose you live in the UK and have any interest in inflammatory bowel disease (IBD). In that case, you will likely have recently seen news articles in which researchers from University College London, Imperial College and the Francis Crick Institute announced they had found a section of DNA present in 95% of people with IBD, which causes an excessive immune response and consequently inflammation.[1] This news has been greatly welcomed by many in the IBD community here - myself included. However, the feelings the announcement generated are weirdly reminiscent of a conversation I recently shared with others with IBD.
Last month, I met with members of the Young Adult Advisory Panel - a fantastic group committed to helping Crohn’s and Colitis UK meet the needs of the IBD young adult population. As we walked to the social venue, the conversation led to how we each coped with the often tumultuous nature of IBD. It soon became clear that the common thread for all of our coping methods was hope. Some hope for research breakthroughs. Others hope for a reduction in flare symptoms, and a few hope for a good blood test result.
Living with a chronic illness can quickly diminish hope for many and unfortunately lead to poor mental health. Research suggests that around a third of individuals diagnosed with a life-changing chronic illness will experience symptoms of depression.[2] But, as so many of us with IBD will tell you - hope is never truly extinguished.
Over the years, hope has taken on several names—the indomitable human spirit, desperation, or perseverance—but it has never disappeared from the human consciousness. Unfortunately, IBD and chronic illnesses have also been present in humans’ lives for an equally long time. But instead of looking at this longstanding relationship as parasitical, I rather see it akin to the prevalence of the myth of Pandora’s box throughout history.
We all know of Pandora’s box, a myth that warns of unchecked curiosity and disobedience when Pandora unleashes evil into the world when she opens a box left in her care by the Gods. Despite all the horrors she releases, hope remains and enters the world, providing humans with the resilience necessary to live in a world filled with such evils. This story has been used for many reasons: to curb curiosity and provide hope. We’ve all faced bleak circumstances where we have relied on hope to see us through.
Life with IBD is no different. We have all faced negativity in some form with IBD - whether that be a medication failing to work, health professionals denying you agency or being limited in your capacity to spend time with friends and loved ones. But like Pandora, we know that there is hope, and with that hope, in the words of Martina Sazunic, we use that hope to “build a ladder” and make the best of our respective situations to reach what we are hoping for. Thus, we are all Pandora.
We all are Pandoras, each with our own boxes, living with the negativity wrought by these boxes—but we all also have hope. So, while that breakthrough in research might, in some eyes, look like a minor step forward in the ambiguity of IBD - it is also a reminder that hope is what empowers us to continue advocating for better lives with IBD. So, from one Pandora to another, hope is in your box - don’t forget that.
References
Gallagher, J. (2024, June 5). Major cause of inflammatory bowel disease found. BBC News. https://www.bbc.co.uk/news/articles/c1wwdd6v2wjo#:~:text=A%20major%20cause%20of%20inflammatory,excessive%20inflammation%20in%20the%20bowels.
Professional, C. C. M. (n.d.). Chronic illness and depression. Cleveland Clinic. https://my.clevelandclinic.org/health/articles/9288-chronic-illness-and-depression
Featured Photo by Pixabay from Pexels.
Confronting Crohn's Disease as a Young African Woman: Challenges and Opportunities
By Yeabsira Taye Gurmu, Addis Ababa, Ethiopia
My journey with inflammatory bowel disease (IBD) began in my late teens, when I started experiencing debilitating abdominal pain, diarrhea, and unexplained weight loss. At first, I tried to dismiss the symptoms, attributing them to a common stomach bug or something I had eaten. But as the weeks turned into months, I knew this was something much more serious.
Navigating the Health care system
Getting an accurate diagnosis was perhaps the biggest hurdle I faced. In Ethiopia, access to specialized gastroenterology care and diagnostic tests like colonoscopies is extremely limited, especially outside of the major cities. It was difficult and time consuming to obtain an accurate diagnosis of Crohn's disease, even then. Diagnostic tests like colonoscopies and endoscopies were difficult to come by; there was a long waiting list. During this time, my health only continued to decline, leaving me in constant pain and with debilitating fatigue. Watching my body deteriorate as doctors struggled to diagnose the problem, I recall feeling powerless, ”It was an extremely frustrating and isolating experience."
Grappling with Limited Treatment Options
Once I finally received the Crohn's disease diagnosis, I then had to confront the daunting challenge of finding effective treatments. The older medications, such as steroids were relatively accessible, but the newer biologic therapies recommended by my gastroenterologist were simply unavailable at the time and are presently financially out of reach.
Confronting Cultural Stigma
On top of the medical challenges, I also had to confront the cultural stigma surrounding my condition within my community. Some traditional medicinal practices view digestive disorders as a result of spiritual imbalances or curses, rather than a legitimate medical issue. There were times when I felt a great sense of shame and isolation. The fear of judgment and discrimination made me avoid social gatherings and hesitant to share my diagnosis. This only compounded the mental and emotional toll of living with a chronic, often-misunderstood condition.
Finding Strength in Community : A Hopeful Future
Despite the daunting obstacles, I refused to give up. I sought out support from local patient advocacy groups, Crohn’s and Colitis Ethiopia. Where I connected with others facing similar struggles. Together, we are working to raise awareness about IBD and lobby for improved access to essential medications and specialized care.
Today, while my Crohn's disease remains a constant challenge, I am better equipped to manage my condition and live a fuller life. I continue to share my story, in the hopes of breaking down the stigma surrounding IBD in African communities and inspiring others to persist in their own battles. My journey with Crohn's has been arduous, but it has also made me resilient, empathetic, and determined to create positive change, I reflect. "I may not be able to control this disease, but I can control how I respond to it - and that gives me strength to keep fighting."
Featured photo by Abuti Engidashet from Pexels