NEWS
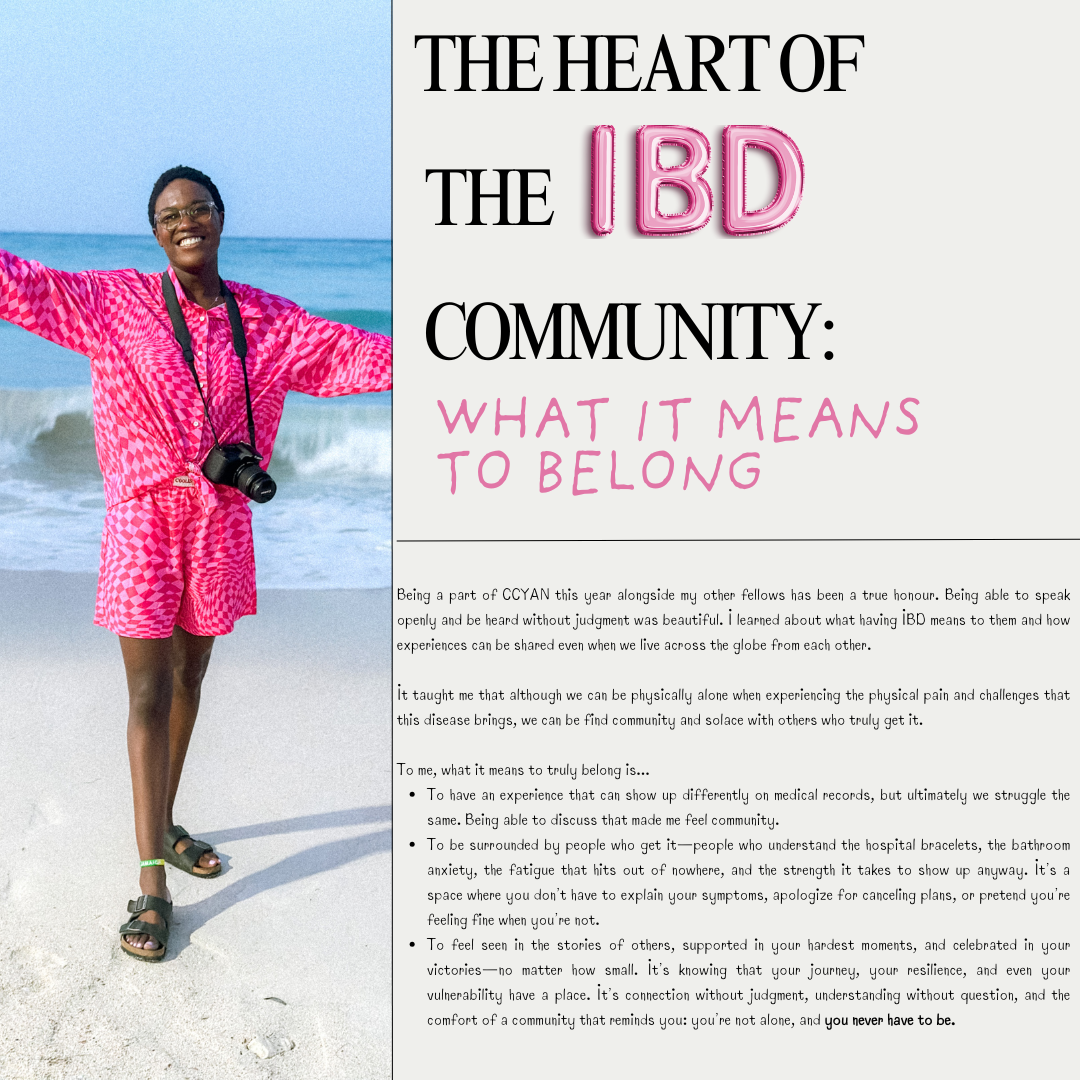
The Heart of the IBD Community: What it Means to Belong
by Lexi Hanson (Missouri, U.S.A.)
Being a part of CCYAN this year alongside my other fellows has been a true honour. Being able to speak openly and be heard without judgment was beautiful. I learned about what having IBD means to them and how experiences can be shared even when we live across the globe from each other.
It taught me that although we can be physically alone when experiencing the physical pain and challenges that this disease brings, we can be find community and solace with others who truly get it.
To me, what it means to truly belong is...
To have an experience that can show up differently on medical records, but ultimately we struggle the same. Being able to discuss that made me feel community.
To be surrounded by people who get it—people who understand the hospital bracelets, the bathroom anxiety, the fatigue that hits out of nowhere, and the strength it takes to show up anyway. It’s a space where you don’t have to explain your symptoms, apologize for canceling plans, or pretend you’re feeling fine when you’re not.
To feel seen in the stories of others, supported in your hardest moments, and celebrated in your victories—no matter how small. It’s knowing that your journey, your resilience, and even your vulnerability have a place. It’s connection without judgment, understanding without question, and the comfort of a community that reminds you: you’re not alone, and you never have to be.
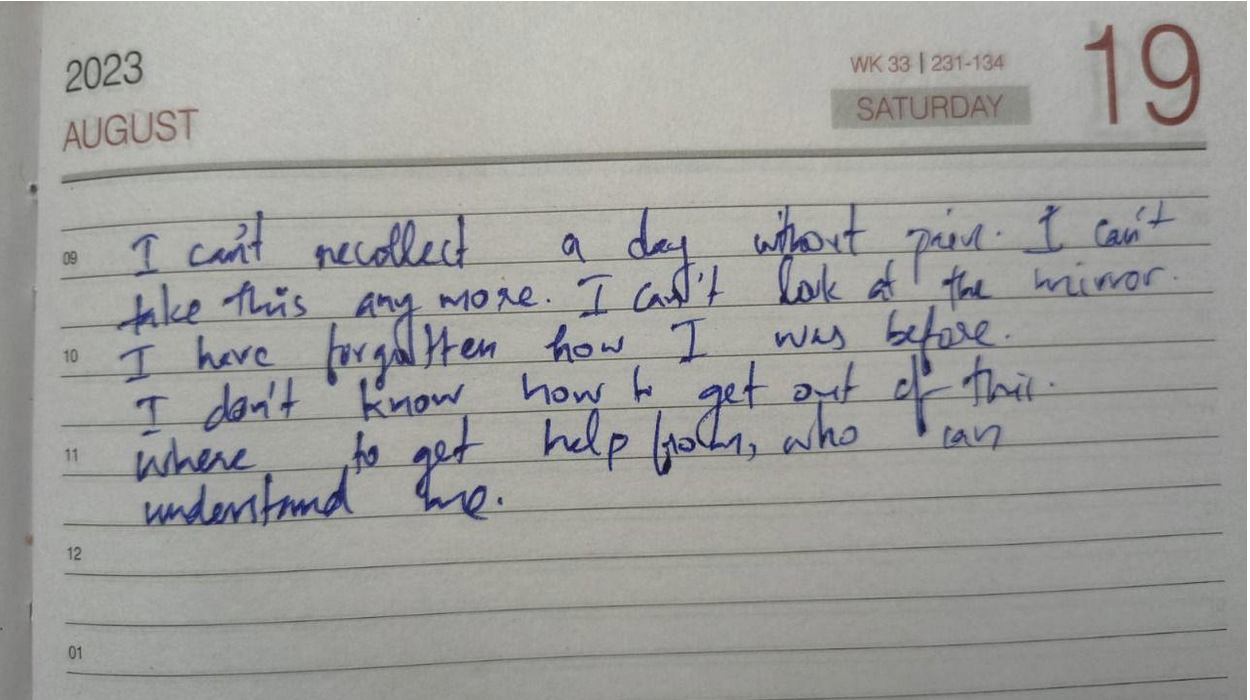
Diagnosis is a Light, not a Lamp Shade (Mental Health & IBD Series)
by Aiswarya Asokan (South India)
It was on May 2nd 2016, a day before my 19th birthday, for the first time in my life, I heard the word Crohn’s, from my doctor back then. It came as a scientifically valid explanation to all the so-called “sick drama” I was exhibiting through the years. But the excitement of this achievement soon faded away when I came to know that there is no cure for this. Then came the joint family decision, we will keep this diagnosis a secret to ourselves. Anyways, who is going to accept me if they know I have got a disease that makes me run to the toilet and that I have to be on regular medication to stop this from happening. For the next 4 years, I lived like a criminal, fearing for every breath this crime will be caught. In between, I was ill informed about the dietary restrictions I was supposed to follow, and kept eating triggers from time to time, meanwhile wondering why this is happening – but was still focused on keeping the secret safe.
Still, life was a smooth sail with a few days of bad weather here and there, till 2020, when I had my worst nightmare: a serious flare that left me hospitalized for more than 2 months and unable to take my final year university exams. And my secret was out. Not being able to appear for exams was too much for an academically excellent student like me. I was experiencing such intense pain that I couldn’t even turn sides in bed. All this made me question my identity and shattered my fundamental belief system. None of the medicines were working on me. A group of surgeons visited me, and told me that if surgery was attempted, my life might be over on the table. When I realized I might die soon, I decided to live a little. Even though I was not able to eat anything, I ordered a red velvet cake and ate it. The 2020 Tokyo Olympics were going on – it was my all-time wish to watch the Olympics live, but my academic schedule did not allow me to do so. So from the hospital bed, I watched Neeraj Chopra win a gold medal for India, while all my classmates were taking final year exams.
After a while, steroids started working and I started getting better. At the age of 23, I was 33 kilograms, severely malnourished and on a high dose of medication. I was not afraid to die but coming back to normal life was a challenge. I couldn’t face people nor attend phone calls. Even notifications from messages were alarming for me. I zoned out from everyone around me. I felt myself as a complete failure.
One person kept on calling me, despite me ignoring all their calls, until one day I finally picked up. He was my childhood bestie, who stood with me till I was able to manage things on my own. He made a timetable for me, which included slots for physical activity, exam preparations, and fun activities, and made sure I followed them on a daily basis. Then the exam date came up. There were times when I took supplementary exams alone, in a hall that usually accommodates 60 students. Everyday after the exam, he would ask me how it went, and suggest a movie to watch as a reward for the hard work. After a while, exam results came, and I had the highest score than previous years. Life was again on.
Whenever a flare up hits me, the first thing I notice is a keen desire for physical touch, especially a warm hug, though it sounds strange. I also clench my jaw while asleep, to an extent that my whole face and ears start to hurt the next morning, which further makes it hard to have food. Within the next 3 years, time was up again for a rollercoaster. I had a stricture, unbearable pain, my oral intake was nil, and I had to go for a hemicolectomy. The anticipated complications for the surgery were extremely frightening. This time my boyfriend came up and assured me that “no matter what, I will be there for you.” The surgery went smoothly and I was discharged. I was physically fit but started experiencing PTSD-like symptoms. I started feeling I was just a financial burden to my family.
I slept all day and night as I was not ready to face the thoughts in my head. My boyfriend used to call me every day – just for those few moments I was living, but the rest of the time I used to sleep. This time no friends nor family could help me. Then I started searching for IBD support groups, came to know about IBD India, took the free mental health counselling, and joined the peer group. For the first time, I felt less isolated and felt a sense of belonging. And slowly I replaced my coping mechanism of sleeping with painting. Gradually I was healing, and started feeling more freedom like never before.
Life goes on. Ups and downs are part of it. But when one door closes the other opens. When you feel stuck, ask for help and keep asking until you get one strong enough to pull you out — that is the bravest thing you can do for yourself.
Image from Unsplash.
Learning to Complain: A Survival Skill for Chronic Illness
by Akhil Shridhar (India)
For many of us living with IBD, saying “I’m fine” has become a habit, something we were taught to say to avoid worrying others or causing trouble. But managing a chronic condition means we can’t afford silence. Doctors need us to describe what hurts, what’s changed, and what’s not working. At first, that shift feels unnatural. How do you speak up about pain when you’ve spent years trying to hide it? Learning to explain what’s wrong isn’t just about getting better care, it’s about breaking the silence, challenging stigma, and making sure our needs are heard. Speaking up is advocacy, and it starts with learning to complain. Many of us were taught to downplay pain, brushing off discomfort to seem strong.
This kind of silence runs deep, shaped by family, culture, and a society that equates quiet with resilience. But for people living with IBD, staying silent can be dangerous. It leads to delayed care, isolation, and missed warning signs. Although, learning to speak up about symptoms is just a part of it. Especially in developing countries like India, where systems often lack the integration, communication is not just helpful but essential. For most, the responsibility of managing appointments, tracking medical records, logging test results and prescriptions, consulting different specialists, and coordinating insurance doesn’t fall on an organised platform, it falls on the patient.
Living with IBD means your body goes through changes that aren’t always easy to explain. Symptoms come and go, and sometimes they’re hard to put into words, especially if you’ve spent years being told not to make a fuss. When you share what you’re feeling clearly and honestly, you’re helping your doctor understand how to support you better. It’s not complaining, it’s communication. And with a little guidance and the right tools, you can learn to speak the language of your symptoms in a way that leads to real care and understanding.
Doctors rely on clear, consistent information to track how IBD is affecting your body, and that’s where accurate symptom-sharing becomes key. The table below outlines the kinds of details that help build a more accurate picture of your condition.
Living with IBD often means navigating a maze of symptoms, appointments and uncertainty. But the ability to speak clearly and communicate will go a long way in getting the care that we deserve. That’s why this table isn’t just a tool, it can help you bridge the gap between what you feel and what the doctor needs to know. Remember, this guide is meant to serve you, so feel free to adapt it, add to it, and make it your own. Bring it to your appointments, refer to it and use it to shape your care in ways that truly reflect your needs.
This log table is for you to document your symptoms and experiences in a structured manner. Save a copy and take notes or just use it as a reference for your next appointment!
Listening to Your Body with IBD: The Stoplight System
by Michelle Garber (California, U.S.A.)
When you're living with Inflammatory Bowel Disease (IBD), your body becomes its own navigation system. Your body is constantly sending you signals, just like traffic lights do. But unlike the red, yellow, and green lights on the road that we instantly respond to, many of us with IBD have learned to ignore or minimize the "rules" or "drills" that we should follow when our body sends us our own, personal warning signs.
So why is it that we respect a blinking car dashboard, a low battery warning on our electronic devices, and traffic signals/signs more than the signals coming from our own bodies? We wouldn’t ignore our car’s check engine light for weeks (and if we did, we’d expect it to eventually break down). So why do we ignore our body’s warnings? Why don't we listen? As with most things, the answer is complicated.
Here are a few reasons why as people living with IBD, we might forget to listen to these warnings, or try to “push past” them:
Living with IBD means that a few warning lights are always on. That is, we might always have some level of fatigue, bloating, or discomfort. This "always-on" background noise becomes our new normal, and we stop noticing when new signals show up. This is risky because it can lead to ignoring major warning signs or missing slow-building flare-ups.
Our symptoms can become our new normal or "background noise," so we're used to pushing through pain. This means that even when our bodies give us that "red" or "yellow" light signal to slow down or stop due to a symptom/pain that is out of the ordinary, we are still conditioned to push through it. For a lot of us, that is a survival mechanism of having chronic pain (pain that never fully becomes "background noise") in a medical system and society that often tells us to "push through." The world is constructed for those who are able-bodied, and having chronic pain/IBD can force us to sink or swim.
We are often taught to minimize our symptoms, for ourselves and others. Sometimes, doctors dismiss our warning signs, maybe because medical literature doesn't acknowledge all the intricate traffic signals for IBD. Maybe, they're just burned out. Or, maybe doctors—and people in general—can't fully understand the severity of IBD symptoms if they haven't gone through it themselves. Whatever the reason, though, we are conditioned to minimize our symptoms. We are taught that our illness "could be worse." In fact, when explaining IBD to others who don't quite listen closely enough, the false notion that IBD is simply "stomach problems" circulates. So much so that we, ourselves, sometimes say this to others or even believe it ourselves. We don't want to be sick. We wish it was just stomach problems. Being told that our personal traffic lights/signals are simply a result of "anxiety" or "are in our heads" make it easy to eventually believe it ourselves because, why would we want to be sick?
We don’t want to "miss out." Sometimes, we’d rather have a moment of fun—followed by a flare/low-spoons day—than not experience the fun at all. Ignoring the signals can sometimes feel "worth it" since it can give us a small glimpse of what "normal" might be like. We are forever torn between the notions of "respect your body's limits" and "you only live once."
Finding a way to make a choice, despite the consequences, can feel liberating in the short-term. This can look like eating a food that you know isn't "safe" just because you want to make a CHOICE and have autonomy over your own body. As IBD patients, choice is often not in our vocabulary – so pushing through the pain of IBD is often the only way we can feel slightly in control of our own bodies. This is a sense of freedom that we greatly lack as IBD patients.
We don't want to be a “burden.” IBD, in itself, is a burden that we already have to carry. Living with it every day is extremely difficult, and that is an understatement. Even so, we still notice how it affects those around us— our caregivers, partners, family members, friends, co-workers, employers, and even doctors. Carrying the burden alone is never the solution, but it sometimes seems like the right one since it feels wrong to allow someone else to feel even remotely similar to us. It doesn't feel right to allow anyone to be down in the trenches with us—at infusion appointments, at ER visits, at ICU admissions, or at "bathroom sleepovers." It doesn't feel right to allow anyone to feel so wrong, even if they want to. Therefore, we ignore the signs, because if we took action that would mean that we'd need help, whether we like it or not. We'd have to reach out to someone, even if that's just a doctor. Simply alerting your doctor that you've failed another biologic can make you feel like a burden since you might feel as though you're giving them more work. Reaching out to loved ones can be even harder as they will often want to be there for you, and you simply don't want to burden anyone anymore.
We’re afraid of what we’ll find if we stop and really listen. As previously mentioned, we don't want to be sick again. We don't want to discover a new co-morbidity again. We don't want to switch medications again. We don't want to be flaring again. We don't want to go to the hospital again. We don't want to experience medical trauma again. We don't want to put life on pause again. We don't want to miss out again. We don't want to be a burden again. We don't want to lose control again. Listening to your body, and truly paying attention to what it's telling you poses the risk of you having to accept the fact that you might have to go through all of these things again. And at the end of the day, we just want to live—freely. It feels like a constant tug-of-war between surviving and actually living.
The truth is: Your body will always tell you what it needs. It’s just your job to check in—gently and consistently.
Since there is no cure for IBD yet, much of this disease has to do with symptom monitoring and, thus, taking as many preventative measures as possible. I, for one, know that I would like to stay in remission and avoid a flare-up for as long as possible. Even so, I know that's only possible if I listen to my body—genuinely listen. Whether that's taking note of unusual fatigue or nausea, a new sensitivity to food, etc., these are acts of listening to your body and its signals. While we are taught from a young age what traffic lights mean and why it's important to follow them, we aren't taught how to notice and follow the signals that our bodies give us.
A few simple things that you can do to start the practice of ‘checking in’ with yourself and your body:
Create your own ‘traffic light:’ write down some of the signs you notice, when you’re feeling ‘green, yellow, or red!’
Set aside a few minutes each day to ask yourself: What "color" am I today? What makes me that color? What am I feeling, and where am I feeling it? If I’m yellow or red, what needs to change? If I’m green, what can I do to stay there?
Not sure where to start? Here’s an example of my “traffic lights,” and some of the signals I use to check in with myself and my body!
A few things to remember/keep in mind:
Checking in doesn’t mean obsessing. It simply means being mindful enough to care. Just like we do for our phones, our cars, and our jobs—we deserve to offer ourselves the same level of awareness, support, and maintenance.
Living with IBD doesn’t mean you’ll always be stuck in red or yellow. Some days are green—some weeks or months, even. You deserve to honor those days as much as you manage the hard ones.
This stoplight system isn’t about fear. It’s about empowerment. You are not weak for needing rest, medical support, caregiving, or time. You are wise for knowing when to go, when to slow down, and when to stop.
Your body isn’t the enemy—it’s the messenger. Listen to it. Trust it. Respond with love. Your body is doing the best it can to keep you alive. Let’s return the favor.
Image from @tsvetoslav on Unsplash.
What It’s Like Working Through Phobias: Creating A Comfort Toolkit
by Kaitlyn Niznik (New York, U.S.A.)
I can't remember a time when I didn't have a blood/needle/medical phobia. I would regularly faint at the doctor's office and even talking about blood was enough to make me pass out in high school. It wasn't a problem until I developed chronic stomach issues and was diagnosed with microscopic colitis. All of the sudden, I was pushed headfirst into a world of doctors' appointments and countless medical tests. It's hard enough to find answers from doctors, but fear can make you ignore your problems, making things worse. I still struggle with this phobia today, but with the help of a therapist, I’m working through my issues. Please seek the help of a trained professional to face your phobias in the safest way possible. Here are several strategies I'm using to make progress facing my fears.
Desensitization Training/ Exposure Therapy
Desensitization and exposure therapy can start with looking at images of videos of your phobia, eventually progressing to more realistic scenarios. For instance, someone with a blood phobia might progress from viewing images to medical shows and eventually going to blood drives. The overall goal might be to get bloodwork done, but you have to build up exposure over time to get more comfortable with your fears.
I've been unknowingly trying to do this my whole life. As a kid, I would reread veterinary books to expose myself to a little literary medical gore. I would deem it a success if I didn't get woozy. Today, medical imagery has become an inherent part of my artistic practice. I find exposure more palatable if I attempt to explore images and procedures from a place of curiosity rather than fear. If I'm looking at veins, I try to ask myself what colors I see under the skin. I've progressed to the point where I can look at surgical photos of arteries and attempt to draw them without getting queasy. It's easier for me to separate myself from a picture than a procedure happening to me, so that's where my exposure therapy has started.
Working with a therapist, I did a deep dive on my phobias and my hierarchy of fears. Instead of just seeing all situations surrounding blood or needles as being equally terrifying, I was able to sort them into a list of situations with varying intensity. While younger me thought a finger prick was the worst situation possible, I now list it much lower on my list, opting to put IVs in a higher position. It's all a matter of perspective. By making a fear hierarchy, I was able to tackle lower intensity situations and gain confidence and resilience before braving my top fears.
Keeping A Sense Of Control
When I was little, my family had to trick me to get me in the doctor's office. In adulthood, I tried to mimic this strategy by being spontaneous. Instead of scheduling a flu shot and worrying about it for weeks in advance, I'd wake up and decide to go that morning. This strategy somewhat lessened my stress, but it also felt too hurried. I never had a sense of control, just urgency to get it done and over with. It didn't leave me in a good headspace and I still found myself fretting over the possibility of getting a shot for weeks ahead of time.
Now, I'm better prepared. With the help of my therapist and journaling, I've made lists of what is within my control during doctors’ appointments. I keep a “comfort bag" ready and always bring it with me to appointments. If I need blood work, I pack my own snacks for afterwards and plan to reward myself with a sweet treat from a nearby cafe. I also pick out my "victim” arm ahead of time based on which arm feels stronger than day.
When it's my turn for bloodwork, I tell my nurse right away that I'm terrified and I'm a faint-risk. I also ask for the reclining chair when possible. It's not so upright that I'll get dizzy and slump over, but through experience, I've also found that fully lying down feels more vulnerable and heightens my fear. A reclining chair puts me in a better headspace, so it is important that I advocate for my preferences. Doing small things consistently and giving yourself small choices in your healthcare can help you feel more in control and you'll know exactly what to expect.
Pack A Comfort Bag, Activate Your Senses
In an effort to ground myself, I try to pack things in my bag that activate my 5 senses of sight, sound, smell, taste, and touch. I always have these items in a bag and ready to go. Consistency is key, so I bring them with me to all of my medical appointments. When I’m in the waiting room, I grab my headphones and put on some music. I also pack sensory items that are calming like fidget toys to distract myself with. If I’m getting blood drawn, I have a tennis ball handy that I can grip, tissues for when I cry, and a snack for when it’s all over. This kit can be any size and it should be personal to you. Here’s a list of what I keep in my bag:
Snacks
Water
Tissues
Tennis ball (to grip)
Lavender essential oil
Hand warmer
Electrolytes packet
Fidget toy or comfort object (worry stone)
Headphones for calming music or ASMR
Don't Just Wing It, Strategize
Plan out your day ahead of time. Plan to have downtime afterwards to chill, recover, and reward yourself. I like to have a friend or family member drive me to and from appointments just in case I feel dizzy afterwards.
Pressure therapies or tense & release exercises have also been proven to help calm the body. Box breathing is another exercise to keep in your toolkit. It can stop you from hyperventilating and keep you calm. Make sure to try these techniques out BEFORE an appointment or exposure to your phobia. Practice makes perfect and not every therapy works for every person. Find what fits you and make a plan to tackle your phobias.
Potential IBD Accommodations for Teachers and Students (from a NYS Teacher)
by Kaitlyn Niznik (New York, U.S.A.)
This infographic was created from discussions with other teachers in the United States living with IBD. Through those conversations, I realized that the workforce can be a scary and precarious place for people living with chronic illness. As a unionized, tenured teacher in a public school, I acknowledge I am in a privileged position to disclose my IBD. However, a teacher or student can choose not to divulge their chronic condition for a number of reasons including job instability or the fear of being singled out. I made half of my graphic focus on discreet ways to manage your IBD within the education system without revealing personal health information. This half includes having an emergency supply pack, trusted contacts that you can call for assistance, and knowing the location of private bathrooms instead of public stalls.
The other half of my picture illustrates ways a student with an IBD can pursue written accommodations to protect them at school. These include obtaining an Individualized Education Program (IEP) or 504 Plan after their doctor writes a note confirming their diagnosis and its impact on the student's daily life. In the student's records, they would be classified under the "Other Health Impairment" category and this form would be reviewed and adapted annually. Parents, teachers, and district personnel would work together to create an IEP or 504 plan that supports the student's needs, helps them manage their illness, and works to reduce the student’s stress in an educational environment. Teachers with an IBD can also present a doctor’s note to their district to receive reasonable workplace accommodations.
Why Finding Your People Matters
By Maria Rouse, N.C., USA
It took me nearly 15 years to begin finding community as someone with inflammatory bowel disease. It was a very lonely 15 years.
I try not to be so hard on myself, since I was first diagnosed with IBD when I was 10. There is not much in the way of accessible peer support for youth with IBD, especially at that young of an age. It was not an option I ever realized could be possible through my health system, and social media as a platform for peer support was just beginning at that time.
My inability to find community led to a false perception of singular failure. I was the only person my age that I knew with IBD, and consequently internalized ableism spread malignantly within my mind and began marring my conception of myself.
With the stigma associated with IBD, it is also not something you typically share about yourself with other kids on the playground, or even when you’re getting to know people during orientation at college. I have met several friends that I only much later learned had IBD.
Ableism is a key motivating force in keeping us silent from sharing our stories and lived experience with others. Ableism is part and parcel of patriarchy, colonialism, racism, sexism, or most of the negative isms that still permeate society. It encourages us to remain alone in our journeys as chronically ill people.
In a system that often tries to force us to act individualistically and hide our unique qualities for the sake of its imposed and exalted definition of success, building disability community is a light in the darkness. It is in itself an act of resistance and radical vulnerability in a society aims to police abnormality and difference. This can make us believe that our challenges and needs are uniquely too much, when nothing could be further from the truth. Community reminds us of our humanity as chronically ill people.
In any setting, making new connections and friends can be terrifying, particularly if you have felt so alone and different all your life as a person with a chronic illness. It can feel especially vulnerable to join a support group discussing such sensitive topics as disordered eating and body image with a whole new groups of people. But forming community through a group such as CCYAN is so worth any initial awkwardness or difficult topics.
The reality is that peer support is not just about you, although it often is cathartic and restorative to know we are not alone and to learn how others managed the difficulties that IBD created in their lives. Peer support is also an act of advocacy, allowing disabled and/or chronically people to take up space when so often our voices are not heard. Building community is an act of advocacy for yourself and also others who may still face barriers in sharing their experiences.
In short, don’t wait years to engage with peers who have IBD. Make time for that peer support group meeting, attend that advocacy event, or connect with peers over Instagram. There are typically more obstacles for chronically ill people to engage with peers, whether that is being immunocompromised or having limited spoons or energy. However, engaging with other IBDers in whatever format is accessible to you is well worth the effort. Life is truly all about connections, and the ones you make with those who have very similar experiences as you can be some of the strongest bonds you will experience. You never know what can come out of it, and how the world could be changed for the better.
Featured photo by Darrel Und from Pexels.
When the cared for becomes the carer.
By Selan Lee from the United Kingdom
I’m not the biggest believer in Astrology. I might complete an occasional zodiac quiz or look up my horoscope when life seems complicated - but I’m not one to base my whole personality around my status as an Aries. However, in light of recent events - I’ve become a bit more of a believer.
At the start of 2024, I made my annual Google search on the predictions for the Lunar New Year. What started as a little harmless fun quickly turned depressing. My fortunes for 2024 looked bleak as a dragon zodiac, and now I can see the start of my 2024 misfortune. Coincidentally, my mum began experiencing balance and coordination issues at the same time as my feeble attempt to predict the future. Following visits to the GP and A&E, a transfer to a ward and surgery - Mum has been relieved of the meningioma that started it all. I realised our roles had been reversed for the first time on Mother’s Day. I, who had been cared for as a daughter and a daughter with Crohn’s disease, had become the carer and guardian of a mother who’d been caring from the moment she found out about me.
Only now that she is home, with the benefit of retrospect, I realise I had a small glimpse into a carer’s experience. Many of us with chronic illness gripe that often, and quite rightly, our experience is never fully understood or communicable. But the trauma and sacrifice of carers is something even less understood. My mum would never call herself a hero or a loyal supporter, as many news headlines and commenters like to attribute to partners, loved ones and friends of chronically ill people. It is a title that never sits well with her and similarly with me following the last few months.
I sat next to her at every medical appointment. I anxiously walked the hospital corridors during her surgery. I memorised every detail of the conversations with the nurses. I visited her every day and filled in every piece of paperwork. Just like she did these last 6 years.
The roles had thoroughly been reversed, and not once did I feel heroic - I felt helpless, even more than I did when I was freshly diagnosed.
With the advantage of improved research and awareness, more and more people are aware of the intersectional and complex identities of people with chronic illness, as exemplified by the IBD Disk (Ghosh et al., 2017). However, this level of understanding and empathy has yet to be mirrored in the perception of carers. They are still a monolith of loyal, self-sacrificing heroes - not deeply traumatised, frequently tired and overwhelmed soldiers.
I am fortunate to have someone and a support network to rely on to come with me to hospital appointments or to talk to when being sick becomes a little too tough. I am acutely aware they are one of the reasons I’ve been resilient with my IBD (Keefer, 2018). Their endless care, kindness, and generosity are never lost on us, but as Atticus Finch said, “You never really understand a person until you consider things from his point of view...until you climb into his skin and walk around in it.” The experience of chronic illness can never be fully understood, but so is that of the carer. Some will be lucky to encounter this responsibility later in life. Still, one thing is for sure - it is one that no one is ever truly prepared for, and though it shouldn't be lauded to a pedestal which diminishes the status of the chronically ill person - it definitely is one that I believe deserves the same comprehensive appreciation.
Featured photo by Matthias Zomer from Pexels.
References
1. Ghosh, S., Louis, E., Beaugerie, L., Bossuyt, P., Bouguen, G., Bourreille, A., Ferrante, M., Franchimont, D., Frost, K., Hebuterne, X., Marshall, J. K., OʼShea, C., Rosenfeld, G., Williams, C., & Peyrin-Biroulet, L. (2017). Development of the IBD Disk: A Visual Self-administered Tool for Assessing Disability in Inflammatory Bowel Diseases. Inflammatory bowel diseases, 23(3), 333–340. https://doi.org/10.1097/MIB.0000000000001033
2. Keefer, L. (2018). Behavioural medicine and gastrointestinal disorders: the promise of positive psychology. Nature Reviews Gastroenterology & Hepatology, 15(6), 378–386. https://doi.org/10.1038/s41575-018-0001-1
I’m sorry to all the people I hurt while I was hurt
By Yeabsira Taye from Addis Ababa, Ethiopia
Being diagnosed with Inflammatory Bowel Disease (IBD) is an experience that is difficult to put into words. It is a moment that carries a mix of emotions, thoughts, and uncertainty. For me, it was a whirlwind of confusion, fear, relief, and hope all at once. It offered a sense of closure to that chapter of uncertainty.
During the difficult times of my flare-ups, I found myself longing for the support and understanding of my beloved ones. Perhaps what hurt the most was the way “some of them” invalidated my experiences. Whenever I tried to share my pain or express how I truly felt, they dismissed my feelings as mere exaggerations or attention-seeking behavior. It was devastating to have my emotions disregarded and to not have my pain acknowledged by those I held so dearly.
BUT of course I am very grateful for the love and support of the people who take care of me. They understand the challenges I face and go above and beyond to ensure that I am comfortable and well-cared for. Now, after I have faced three flare-ups within two years I understood that, it is important to acknowledge that everyone has their limits; chronic illnesses bring with us a multitude of physical, mental, and emotional challenges. It is not uncommon for loved ones to experience emotional detachment as they witness their beloved family member, husband/wife, fiancée or friend endure the hardships of a chronic illness. They may distance themselves emotionally to shield them from the pain of witnessing our struggle.
There are moments when the perception of distance from those we hold dear can lead us to inadvertently detach ourselves from them in an attempt to protect ourselves. It wasn't easy dealing with the physical and emotional pain that accompanied our condition, we may blame them for making our flare-ups even harder to handle.
As time went on, I realized that the mistreatment I endured from others was not a reflection of my worth or value. It was a poignant reminder that everyone faces battles of their own, and sometimes, their harsh words or actions are merely the projections of their own pain and insecurities. While navigating through my flare-up, I understood that forgiveness was essential. Forgiveness became a powerful tool in reclaiming my strength and power, transforming the negative energy into something positive.
Today, I am grateful for the difficult journey I endured during that time of flare-up. It allowed me to tap into my resilience, strength, and inner resources that I might have otherwise overlooked. It taught me the importance of self-reflection, self-compassion, personal growth, and forgiveness.
Featured Photo by Vie Studio from Pexels
Should You Be Open About Your IBD With Others?
By Isabela Hernandez (Florida, USA)
I’ve often wondered the effects of how open I’ve been about my disease, through these articles, on the mental coping of my disease. It has gotten me to look back on my journey and the strides I’ve taken when sharing the mental and physical fatigue I deal with. I used to be very closed off when it came to all things IBD. I would tell the people around me that I have “stomach issues,” and that’s it. As I entered into my advocacy journey, I started letting the people around me in; giving them the information I withheld for so long about a part of myself I repressed from the outside world. I truly believe that through this, I have been able to mentally process my disease better. So, this is where I wonder: does being more open with your disease mean better outcomes? Or alternatively, does being private about your disease mean you are able to maintain sanctity within the crazy experience that is having a chronic disease?
It can become exhausting trying to share an experience with someone that will never truly understand what it is like to be in your shoes.
As I spoke with another 2022 fellow, Carina Diaz, about this, and she expressed, “It’s exhausting to continuously have to educate people closer to me on IBD, especially family. I’ll either point them to resources so they can do their own research [like content made by fellows] or tell them that I’m not talking about my health at the moment,” which is something I feel and relate to daily. Even though I am open to those around me about my IBD, they still sometimes look at me with eyes of confusion, never fully grasping what I tell them. It can become exhausting trying to share an experience with someone that will never truly understand what it is like to be in your shoes. So, this somehow supports the argument that being private about certain parts of your IBD can actually save you from the exhaustion that comes from having to share very personal parts about yourself.
I encourage every IBD patient to find a community of patients your age to talk to.
However, Carina also mentioned, “It’s comforting to know I’m not the only young person who sees their doctors more than their friends.” I have come to the conclusion that there are two ways that I find best when being open about your disease. I believe being completely transparent, and not holding back, with other individuals who suffer with IBD through peer support absolutely shifts the way you will view your disease, while being open but maintaining healthy boundaries with friends and family will help them grow in their understanding of your disease while allowing you to maintain autonomy within your space as a patient. Having peer support through the IBD community is one of the best things that has ever happened to me and something I am eternally grateful that I found. I encourage every IBD patient to find a community of patients your age to talk to, hang out with, or even just meet virtually and challenge yourself to share parts of your journey you have been too embarrassed or scared to share. I used to think that certain parts of my life were too much or too humiliating to share to others and that they were these huge parts of my life that could never be lived down. However, I’ve found that once you share them, you realize they’re actually not that big, and they become just small, formative parts of the journey as a person. It is even more comforting to share them with people who you know, in some way, will understand.
This article is sponsored by Trellus
Trellus envisions a world where every person with a chronic condition has hope and thrives. Their mission is to elevate the quality and delivery of expert-driven personalized care for people with chronic conditions by fostering resilience, cultivating learning, and connecting all partners in care.