NEWS
"But You Don't Look Sick" - A Photo Journal
By Vasiliki-Rafaela Vakouftsi from Greece.
“But you don’t look sick”. How many times I have heard this? Maybe I don’t look sick to you but I am sick and my daily life is far from what you may think.
I tried to captures in pictures my daily routine as a chronic patient and I’m going to share them with you.
First of all, let me tell you some things about me. My name is Vasiliki-Rafaela, I’m a musician and I have Crohn’s Disease, Adrenal Insufficiency, Psoriasis and Psoriatic Arthritis. I have written a book about my journey with Crohn’s and a book about my life with Adrenal Insufficiency. Also, I really like traveling and I really miss it with the pandemic.
Now let’s start with the hospital visits…
...the hospital stays and therapies…
...the hospital stays and therapies…
...take the pills, medicines and supplements…
...and maybe today is the day of the week for the injection for Crohn’s…
...or maybe I need the emergency shot for Adrenal Insufficiency…
And now it’s time for a walk.. Don’t forget to carry the pills with me...
...and of course my medical ID…
Back at home again.. Really exhausted...Let’s check the e-mails and read a book before going to sleep
That’s a little idea of how my daily life is. But, you’re right. So before saying “You don’t look sick” think of what is behind the image and what you cannot see…
The Difficulty of Finding a Treatment
For the ordinary individual, health is accepted as a given. It’s a part of life that mostly runs in the background like a minimized window on a computer. It’s always running, keeping us alive, and impacting our physical and mental states. Yet again, for most people, it’s rare to directly confront it on a minute to minute, or even second to second basis. Instead, it emerges at the forefront of life either by active and deliberate personal choice, or when something goes wrong. When a previously silent computer program running in the background becomes unresponsive, what was once insignificant becomes a major issue. To a greater extent, when that disruptive program causes our computer to crash and lose all of our work, it’s catastrophic. In a similar way, the typical individual goes to the doctor only on the occasions when their health is compromised by infection, injury, or other issues. Plus, when our health is stable and we are well, the changes we make, like starting a fitness regime, new diet, or implementing mindfulness strategies to our lifestyle, are done by choice.
However, when you live with a chronic illness, health management becomes significantly more complex. For one, chronically-ill patients often do not have the benefit of having a lifestyle defined by stable health. Chronic illness is by its very nature unpredictable. Diseases like Crohn's disease and ulcerative colitis revolve around periods of peaks and valleys - remission and flares. Once again, living with a chronic condition transforms the nature of managing health. The process of searching for, utilizing, and adjusting to a treatment for inflammatory bowel disease, or other chronic conditions, is one of trial and error. Unlike treating the common cold or a broken bone, the path to recovery is much less clear cut. Personally, I have tried various medications across a variety of different medication classes only to discover that they were not effective for treating my particular case of ulcerative colitis. It takes constant monitoring of your symptoms, and a commitment to embracing change to successfully navigate the healthcare system as a chronically ill patient.
It’s a difficult reality that many patients struggle through countless medications, clinics, and treatments before finding relief. Simply put, when you live with a chronic illness, your health is never certain. It’s unlike managing short-lived, common conditions, because there’s no clear timeline. Patients are forced to adjust to a new normal. This new reality is a reality where an individual must persist despite burnout, despite anxiety, and despite certainty. It involves significant sacrifices in one’s lifestyle, and even identity. Confronting health is no longer a special event or a choice, instead it’s a part of the daily routine. I believe this is part of why accepting illness is full of so many emotions, and why fatigue can easily take over. Everyday, patients are fighting a difficult, and often invisible, battle while living normal lives full of other responsibilities. The process, and the challenges, involved with finding and managing treatment do not make this balancing act any easier. Thus, it’s important to recognize the difficult, frustrating, and exhausting experience of patients worldwide. After all, despite illness, set-backs, and struggles, we persist to live lives as friends, artists, and advocates.
Planning with Crohn's
Stay with me for this one – I promise it won’t be as boring as it sounds! If you immediately switch off when you hear the world ‘plan’, or indeed ‘regime’ or ‘strategy’, you’re not the only one! There are, however, benefits to planning when you live with a chronic condition like Crohn’s Disease – and more importantly, if your plans become routines, then they’re more likely to become second nature, and you’ll find yourself doing those tasks subconsciously. Here, I will share some of my planning tips, which you may just find helpful. It’s all about finding what works for you so that you can manage to fit in all of the things you want to do, despite your health condition(s).
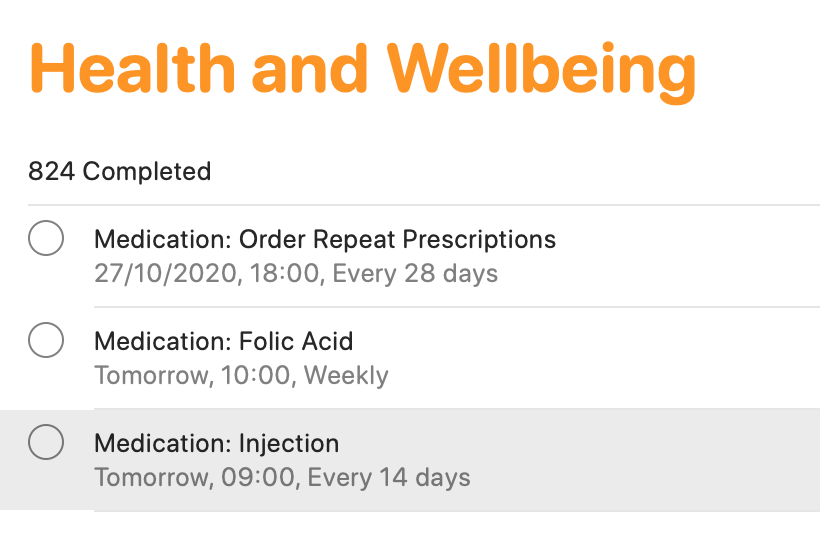
Smartphone apps
There are tons of smartphone apps available to help you keep lists, plan activities and so on! I keep it fairly simple, making use of macOS/iOS Calendar, Reminders and Notes (or the same apps on other operating devices). The calendar function is ideal for noting down all of your appointments. This helps for looking to the future, but also looking back at when and where different events occurred. The reminders app is an absolute lifeline for me. I have separate folders for different activities (e.g. university, health, work, voluntary commitments and so on). I add in activities, and a date/time (or location) reminder. This definitely helps me to keep track of everything that I need to do. If I didn’t, I would definitely forget! From a health tracking perspective, this is ideal as a reminder for booking in my next vitamin B12 injection which takes place every three months, as well as for when I need to ring up my doctor to arrange routine blood tests, when I need to self-inject my treatment, and when I need to order my repeat prescription. You may think that you’ll remember everything, but when you are busy with ‘life’, on top of ‘brain fog’ which many of us can relate to, it’s easy to forget. I know I have done that in the past, particularly when it came to self-injecting my treatment. I would remember that I need it on Tuesday for example, which would be the two-week dose period. However, I would have a busy day at college, would forget when I came home, and then in bed at night, I would suddenly remember, and think ‘I’ll have it tomorrow’. But then tomorrow became the weekend, and before I knew it, it may be a whole week later and I still hadn’t given myself my injection. I knew that was no good, but I just needed to do something about it – which I did!
Finally, Notes are brilliant! Again, I have different folders for a whole variety of different items. ‘Health’ is one of those. I use notes for keeping track of how I have been feeling, as well as for noting down points to discuss with my healthcare teams. I also use notes to keep track of discussions held with healthcare professionals, either face-to-face or over the phone. It’s just another good way to have information at your fingertips to help with your care, while the discussions are still ‘fresh’ in your head.
Scheduling in rest days
We all know what it’s like to live with a condition like Crohn’s – we have so much robbed away from us. As a result, when you are feeling on the better side, you will naturally try to fit in everything that you can. I know that I have been there! Though sometimes, it really doesn’t pay off. That’s why I try to give myself time and space to just ‘do nothing’ – because I know that’s what my body needs. In pre-pandemic times, I would avoid booking in too many back-to-back travels, so that I always had some time to recover. In the current climate, I do my best to block off certain days where I’ll have meetings, keeping overs ‘free’ to do work at my own pace, and also take it easy. It’s all about being in control, as much as possible, so that you give your body (and importantly, your mind) the time and space to breathe.
Leaving the house with everything that you need
Phone. Wallet/purse. Keys. Mask! The list goes on – but it’s really important to have everything that you need to hand. As well as the usual items that most of us require these days, I also have supplies in my backpack and car for every eventuality. This includes painkilling tablets and gel, anti-spasmodic tablets to help with cramps, laxative tablets if I notice a blockage, anti-diarrhoeal tablets if the opposite happens, lactase enzyme to help me digest products containing lactose and the RADAR key to access locked accessible toilets. This list can go on and will depend on personal circumstances. I always find it best to have everything stored in one bag, so you can ‘grab and go’. It may feel excessive, but you will thank yourself later on when you’re not caught short.
Knowing your triggers and avoiding them
Although everyone is different, we all have some kind of trigger which can worsen how we feel. For me, I know that stress is a key trigger for worsening symptoms. That’s why I try to minimise stress as much as is practically possible – although that is much easier said than done! That’s why you’ll generally see me planning to do work well in advance of deadlines, for example, and seemingly ‘being on top’ of everything. In reality, it’s much harder to do, and I do find myself rushing for deadlines still – but at least I have minimised that as much as is practically possible. I am also my own worst enemy. As a perfectionist, I place huge amounts of pressure on myself to succeed and to do everything to the very best of my abilities. While it’s a good quality to have, it isn’t when it impacts on your health. So, it’s really important to be kind to yourself, and to re-evaluate your workload if you find yourself totally swamped and feeling ill. Nothing is worth more than your health.
Do you have any other planning tips which help you to live with your condition whilst getting through life? Let us know in the comments and on social media!
Explaining Chronic Pain
This article is sponsored by Gali Health.
One of the most troubling and tricky feelings of the human condition is pain. It’s the body’s warning signal that something is wrong. It always seems to show up unexpectedly. It’s the world’s worst party guest. Seriously, it could at least bring a party gift, or an extra bag of chips and salsa to share. Instead, it interrupts the flow of midnight ragers and days of routine alike. Pain is the ultimate consumer. It takes, absorbs, and swells, without giving any of itself up. To make it even more complicated, pain comes in more hues, flavors, and shapes than can be counted. Pain is a universal experience, but the experience of pain is unique to each individual.
There is round, smooth, aching pain that rolls around the body all day. There’s sharp, jagged pain that cuts, stabs, and leaves a metallic taste on the tongue. There’s pain that shapeshifts. It howls like a werewolf, then sizzles like the sting from an insect. I could go on, but the list of the types of pain is again endless. That said, living with a chronic illness like IBD means tasting an entire buffet’s worth of pain types. Despite the fact that pain is so specific, and individual, people often try to measure and compare pain. As a chronically ill individual, it can be frustrating to have your pain compared, and rationalized by others. For instance, people will often compare the abdominal pain from ulcerative colitis, or Crohn’s disease to a stomach ache. In reality, chronic pain is much different from everyday pain.
When the pain from chronic illnesses is compared to pain from other illnesses, a large part of the context is ignored. Patients with chronic illnesses and pain have to confront pain oftentimes on a daily basis, and manage pain oftentimes without a totally effective treatment. The pain from a stomach ache, or a stubbed toe will eventually fade, and if it doesn’t, there is generally an effective treatment available. With a chronic illness, no such treatment necessarily exists. There is no timeline for recovery from the pain. Instead, it can be endless and unclear with multiple trials of various treatments required in order to find relief. In essence, chronic pain has no end deadline.
Despite this, the chronically ill often live normal lives everyday. Patients and pain sufferers go to college, go to work, and even to social events despite their pain. It’s especially important to remember this, because for all of its flavors, pain can be quite invisible. Dealing with pain is a challenge, and a burden, but millions of people around the world surmount the obstacle of pain everyday. Accommodations for patients make living with this weight easier, and enable us to be more active members in our communities. Still more work needs to be done to improve the quality of life for those dealing with pain. The compassionate way to treat the chronically ill, is the most inclusive way and the way that eliminates the disadvantages of the disabled. In the future, I hope all pain is treated with the utmost consideration and care for the individual. After all, if that was the case, there would be a lot less physical, and mental pain in this world.
This article is sponsored by Gali Health
Gali Health is an AI-based personal health assistant app helping people with inflammatory bowel diseases (IBD) proactively manage their condition. Gali gathers knowledge from daily interactions and health monitors to tailor support and information to your specific IBD experience.
Emotions and IBD
There are a lot of emotions that come with the diagnosis of any chronic illness, or even any major life change. But laying on the operating table, under the haze and fading twilight of the anesthesia medication exiting my veins, I felt nothing. The echoing silence of the room was heavy all around me. I expected to feel an overflowing stream of emotions flow over me, but instead the most striking sensation of my diagnosis was emptiness. It could have been the drugs dulling my system and my perception of the world. Yet, over time, I’ve started to think that the cause of the void-like feeling around my diagnosis was something incredibly real, and not artificial. The feeling of change is oftentimes so big that it feels like nothing.
In that hospital room, so much had changed with a simple test. The scale of the moment was beyond comprehension. My parents and I communicated without words, because anything that could have been said would have failed. All the periods, letters, and adjectives in the world would never be enough to frame that point in time. So, somehow and instead, I just knew that I had ulcerative colitis without being told. Shock, and the whole experience, was such a surreal feeling. To know that something has snapped, or broken, or ended, but to be unable to directly confront that realization is off-putting. It was easier to not speak the change aloud, because to speak it into the world would make it extra real.
In the weeks after my diagnosis, it was as if a light switch had been switched back on. All of the fear, grief, and anger I had missed earlier suddenly now surrounded me. The trauma of illness is such a widespread and varied experience, but it can be difficult to describe and discuss. It’s isolating to feel different, and to feel like you’ve lost a piece of yourself. Health is something that most people take for granted or don’t think about. So when it’s taken away from you, its absence becomes the dominant part of your everyday life. The shift in my lifestyle to one focused on health had a significant impact on my mental health. I was in an environment, my freshman year of college, where everyone seems to be testing the limits of their independence. Thus, to feel completely dependent on my unstable day-to-day health felt unfair and tragic.
It’s a challenge to have the energy to battle painful, and draining symptoms on a daily basis. I learned that adjusting to my illness, and all of the treatment that comes with it, was a major part of my healing journey. On top of that, I realized that acknowledging the emotions I was experiencing was an important part of accepting my illness. It’s normal and natural to be angry, to grieve, and even to be nostalgic for your life prior to diagnosis. In fact, for me, it was the first step towards opening up and connecting with others in the chronic illness community. My experiences, feelings, and my relationship towards my health has been full of highs and lows. Most of all, I’ve learned that the negative and positive emotions I’ve encountered from dealing with illness are all valid. They’ve helped me grow, learn, and evolve as an individual. Every journey is different, and that is perfectly okay.
My IBD Life: The Road Not Taken
Hello everyone. I hope you had a wonderful World IBD Day!
The month of May is special to me because May 17 happens to be my stomaversary! Three years ago, on May 17, I received my ileostomy. It was a decision that I made after Infliximab a.k.a Remicade gave up on me. My doctors wanted me to try some more meds, but I insisted on the surgery. I wanted a permanent ileostomy, which was quite a surprise for the surgeons. I remember them coming up to my hospital bed and asking me questions about my education and background. I smiled and assured them that I did want my ostomy to be permanent. In a country like India, where stigma and taboo exist even with the state of being ill, it is rare for a 24-year-old person to ask for something like an ileostomy, additionally, a permanent one.
I actually wanted an ileostomy back in 2015. I would have had a temporary ileostomy then. I had already failed most meds and immunosuppressants with the exception of MTX (methotrexate) and biologics. I could not afford biologics and the doctor I consulted then had already told me that only biologics or surgery could help me get better. Soon thereafter, I started visiting the outpatient department of the All India Institute of Medical Sciences (AIIMS) in New Delhi, which is considered to be the best hospital in the country and it is a government-run hospital, so consultations are free. However, owing to the massive burden of patients that it bears, not every patient gets the same level of care. The doctors try their best, but they are humans after all.
When I went there, I begged the doctors to give me an ostomy. I had already watched countless videos on YouTube about young people living their lives with a stoma, and I figured a surgery would buy me some time and my intestine would heal, and I could get it reversed later. I was 22 then, and the doctors told me that a stoma at 22 would make my life very hard in India. I was thus advised to try the same medicines once again that I had already failed along with some new antibiotics and brands of aminosalicylates. I did not do any better on them. My condition was deteriorating and my scans were not good, but it was still not bad enough to get me into a bed at AIIMS. Meanwhile, in addition to my symptoms of constant bloody diarrhea and weight loss, I was beginning to experience some pain in my pelvic regions whose intensity and duration were growing day by day.
In December 2015, I went to the GI OPD at AIIMS and cried straight for 4 hours in pain. It was then that a senior doctor saw me and I got to consult with him. I begged him to operate on me. He consoled me and assured me that I would be treated better and I was then admitted to the GI ward. I stayed there for a month amid more courses of steroids, antibiotics and scans. On January 2nd, 2016, my 23rd birthday, I was given my first dose of Exemptia (a biosimilar of Adalimumab a.ka.a Humira) which was cheaper than Remicade, and patients at AIIMS were provided with some assistance by the firm that manufactured the drug to lower the financial burden. I went home with some hope which lasted for only 2 weeks. After 2 weeks, I lay 24/7 in pain in my bed, 10 steps away from the toilet. I managed to pass some firm stools, but that made the pain even worse which was now affecting both my hips and lower back and my thighs. It felt like a thousand hot steel knives carving into the flesh inside my intestines and my pelvis. I frequently visited the ER in the middle of the night, screaming in pain to get a dose of IV Tramadol.
As I write this, it almost makes me want to stop writing further. I remember taking sleeping pills, antidepressants, and tramadol pills to sleep and kill the pain. I remember trying to end my life for 2 nights. I remember trying to hang myself. I remember giving up. My younger brother had received an offer of admission from Imperial College London, but he was working instead, to run the house and afford my treatment. My parents had separated. I figured it would be better for everyone if I killed myself. I really didn’t want to die though. I just wanted the pain to end. I eventually ended up admitting myself again in the hospital in February. An MRI of my spine did not find anything. Psychiatrists thought I was exaggerating my pain because of past emotional trauma. The SR (Senior Resident) who oversaw me in the ward did not believe me when I told him that Adalimumab was not working anymore and my symptoms were worsening. After a month, I ended up faking wellness (I told my doctor I wasn’t feeling any pain on Clonazepam, when in fact, I stayed up all night in pain and additionally did not ask for a pain shot) to get out of the hospital.
Back home, I started taking more pain pills and anti-anxiety drugs. The biologic was not doing its job anymore and after another month at home, I was back in a bed at the hospital. This was my worst. I was totally incontinent, bedridden, and weighed 80 lbs. I passed blood and mucus incessantly even when I was ordered not to eat/drink anything. Doctors had given up on me, and Infliximab was just too costly. There was no way I could afford it. One night, the SR came in and told my mother to take me back home. That night, once again, I found myself thinking about death. I was not afraid of it, but I regretted that I could not do anything significant. My ambitions and dreams were dying with me. The next day, I and my friends started a crowdfunding campaign to gather money for Remicade, which was very successful owing to the kind generosity of my college batchmates, and I gained some more time on Remicade. But the pain never went away. It was constant and Remicade had minimal effect on it. I was still incontinent. All that any drug could do for me was to decrease the number of my visits to the toilet. Incontinence and pain were chronic. I depended on diapers, a cocktail of many pain meds, and many unhealthy, unsafe, and drastic measures to get through the day and night. I was getting Remicade infusions every month instead of the usual 8-week frequency because there were signs that Remicade too was not working. I found myself in the hospital every other month.
When Remicade finally gave up on me, and I had lost 2½ years, I decided it was time to get rid of my colon once and for all. My GI tried to persuade me to try some more treatments like FMT, but I aggressively denied. While I was being taken into the operating room, my surgeons once again asked me to permit them to retain my colon. I told them that if they found anything worth retaining, they could. When they opened me up, they found - “Hepatic flexure, transverse colon and up to upper rectum thickened. Descending colon and sigmoid colon densely stuck to parietal wall, mesentery shortened and thickened”. These are the intraoperative findings as written on the operation note from the day of surgery. The surgeons could not save any part of my colon except for the lower rectum and anus. When they told me after the surgery that they could not save anything, I was not sad. I was relieved. My pain was gone. I had a chance to re-build my life now. I would not have to stare at the outside world from the window grills of the hospital hallway anymore. I don’t know if that operation note explains my pain, but I firmly believe that I was never insane or exaggerating my pain because I never needed IV Tramadol after the surgery. Earlier, I had been labeled an addict and treated like a liar. All my self-doubt disappeared after my surgery.
Getting back on my feet with my ostomy was not easy. I suffered from ileus immediately after the surgery and I could not keep anything down. I was sent home prematurely because that is how things work in a hospital with too many critical patients and too little beds. I was dejected and did not want to go to the hospital. I was scared because this surgery was supposed to work. I was vomiting furiously. Reluctantly, I admitted myself back after 3 days of discharge and finally after 15 days, my stoma ejected out gallons of intestinal juice like a fountain, and when it stopped, I could eat again. I went back home. After 6 weeks, I was back to work and I never went back to the hospital again, not even for a follow-up or to get my discharge papers. I had lost a lot. Now I had to get everything back. Finally after 2 years, in August 2019, I found myself in the best graduate school in India - the Indian Institute of Science.
I never want to tell my story to people, because I’m not sure what kind of message it sends out. When I go to the annual meeting of ostomates at AIIMS, I find nobody in my age group. I feel alone and wonder if I made the right decision. I wonder if I would encourage another 24-year-old in India to get the surgery. I often did many things that bordered on insanity to get through the intense pain I felt for over 2 years. I often ask myself if I could have done anything else. What do you think? What would you have done if it were you instead of me? What would you choose? When I told other patients that I was getting an ostomy, I received many messages urging me not to go for it. They told me it would destroy my life. Here I am though, living with minimal pain and no meds, in the best graduate school in my country studying Aerospace Engineering, which was my childhood dream. However, I have a very limited social life. I might never be able to work for an industrial organization. I don’t even know if I can make a career in academia. My future is still uncertain. With every passing year, statistically, my chances of falling into a relapse increase. My rectal stump still passes out mucus and blood frequently, and my stoma health is not so good. In a hurry to make up for lost time, I also haven’t given myself time to process everything that has happened to me.
I guess in the end, it’s a journey of self-discovery where you find out who you really are, what matters to you the most and what you are capable of. I am content with the choices I made, good or bad. Things could have gone more wrong because of my choices and I might not have survived. I was prepared to take that risk though. I had dreamed a dream, and when that dream was lost from me, I wanted it back so desperately, that I was ready to sacrifice anything to get a chance to work on those dreams again. That’s who I am. I never knew if it would work out, but I sure did believe. And I hope you believe it too. No matter how bad it gets, I want you to believe that things can work out well in the end. And I want you to hold on to that belief firmly.
I share my story in the hope that you don’t give up like the many times I did in despair. I hope that whatever road you choose for yourself ends in a brighter place than where you began. I hope that your story becomes a greater force of hope than mine. I hope.