NEWS
10 Things to Know If You're Recently Diagnosed with IBD
Newly diagnosed with IBD? I wish you knew these first.
Growing up as a teenager, I was a perfectly healthy child. I ate regularly; I was active and a bright kid who never had any particular routine or lifestyle that I used to follow. But everything started turning upside down once I started seeing symptoms. An bigger tragedy was when I almost felt like the game had ended after being diagnosed. No! Not at all. The actual game starts only after the diagnosis. Our bodies are always changing with IBD. From one day to the next, we don’t know how we are going to feel or what is going to happen. So it is of the upmost importance to know yourself and your body first. Ignorance certainly isn’t bliss here. If you feel like IBD is ruling your life, it’s time to take back the control. Here are the 10 things which I would like to share with all those who are newly diagnosed with IBD:
Educate yourself: Knowledge is power. Understanding IBD leaves you better equipped and empowered to manage it. There are many patients out there without enough knowledge about their IBD. It’s our responsibility to know everything we can about our disease and also our bodies. Take the time to learn everything you can. Read and discuss as much as possible with your doctors.
Track your symptoms and triggers: Learn about your own symptoms and triggers. Many doctors suggest maintaining a food diary so that your doctor may be able to use the data you gathered to help guide your treatment plan. We can understand our daily life and limit what happens to us by doing this.
Never miss your regular follow ups: After reaching my first remission, I assumed I was completely cured and had stopped my regular check-ups and follow ups with my doctor. The penalty for being so ignorant came with a cost of having the next severe flare up within the next few months which completely drained me and pulled me back to square one. IBD is a disease which needs to be managed and if you feel symptom free, you are not cured, it’s just that your medicines are working and controlling your symptoms. So it is important to have regular consultations with your doctor and monitor the functioning of your systems.
Make every appointment count: Be well prepared as to what you need to discuss with your doctor before hand as most of the appointments will be limited to 10-15 minutes and you tend to lose out on discussing important stuff. You can even jot down pointers on paper before entering the doctor's cabin.
Don't be afraid to ask for more information: The time slot allotted for each appointment may be limited. That doesn't mean you need to limit your queries and clarifications. Make the best of that limited time. For instance, if you’re being treated with steroids, ask for detailed information about how this medication could influence how you feel, the side effects, mood swings, weight gain, and such.
Know your treatment: First, know what kind of treatment the doctor has put you on. Whether it is the traditional treatment or biologics or allopathy or any other alternative therapies. Understanding your treatment can help you know what is happening to your body and analyse your recovery rate to attain symptom free life by choosing the best that suits your body as what suits others may not you and vice versa.
Emotional health is equally important as your physical health: There could be days when your entire body hurts and there is nothing you can do. There could even be days when you don’t even want to move because you are so exhausted. During those days it’s not easy to control your emotions as you tend to feel more low and helpless. But you can still fight back by choosing to feel “it's OK”. Don’t let your IBD control you.
Coping with Stress: Stress doesn’t cause IBD, but it can sometimes make symptoms worse. Stress relief is crucial if stress provokes your flare-ups. Learning how to cope with stress and anxiety isn’t always easy. But it’s really important for us to keep stress under control. Yoga, meditation and music could be a few tools that may be helpful in this.
Reach out for help when needed: IBD can be an embarrassing disease. It’s normal to feel alone sometimes. At a young age, we are taught not to discuss what happens behind a bathroom door. This can leave those of us with IBD, feeling extremely isolated and even hopeless. This can impact our self-esteem and quality of life. It's utmost important to have some go to people who understand these challenges and support us in every step of our journey.
Nutrition matters: Understand how your system works and choose what goes into it rightly. When the intestine is under attack, it has a hard time absorbing nutrients. Therefore it's important for us to be aware of what we eat. Follow a low residue diet to relieve abdominal pain and diarrhea. If you have strictures, it is especially important to avoid nuts, seeds, beans and kernels.
These are few of the things which I feel we need to keep in mind and plan our lifestyle when newly diagnosed. Knowing these pointers at the initial stages makes our lives much easier.
Challenges as a Crohn's Warrior in Malaysia
In Malaysia, Crohn’s disease is also known as “Western Disease” or “Rich People Disease.” The reason behind this is mainly because Crohn’s is a rare disease in Asia, particularly in Malaysia, as compared to Western countries. Many in Malaysia have never heard of this disease. Therefore, they are not aware of the Crohn’s and colitis patients’ struggles with their pain, medical procedures and psychological issues.
At the beginning stage, I had no one to guide me. I had no idea on how to handle my newly diagnosed disease. With no medical background, no one in the family or friends with similar conditions, I struggled to cope with this disease and my normal life. Can you imagine the struggles I faced as a first year university student with my condition? I was alone and I didn’t even understand what was going on and my normal was no longer a normal. The internet was my only resource for information other than my doctor. By reading everything I could find in the internet, I slowly started to understand this disease. Back then, there wasn’t even a support group for Crohn’s in Malaysia as the disease is relatively unknown to Malaysians. In fact, I didn’t even known about any other Crohn’s patients until I met one almost a year later after my diagnosis. My gastro doctors encouraged me and other patients to start a group so we could create a support system to each other. Now, newly diagnosed Crohn’s patients or caregivers in Malaysia have access to few channels that they could use to discuss, ask, guide and support each other going through this painful disease.
Living with chronic disease, I had to adjust and adopt to new diet and lifestyle. Changes in diet were mostly trial and error in the beginning. I had to monitor my consumption and take note of any changes. Why did I have to monitor those changes? It is simply because I wanted to avoid flare ups that were caused by certain food that I consume. For me, I found that my Crohn’s is mostly under control when I avoid foods that contain eggs. So I have to ensure my daily food consumption is egg free. If I didn’t, I’d have to visit toilet frequently the whole day. Precaution is needed for Crohn’s patients because flare ups can happen in any situations, therefore any heads up is a good one to have.
Apart from my diet, I had made some massive changes to my daily activities too. Since I’m an Ostomate, I have to ensure that I don’t partake often in hardcore sports in order to avoid stoma prolapse.
The understanding and acceptance of IBD in society is still a challenge for me. Most of them, as I mentioned above, do not know about Crohn’s disease. I remember one of my friends asking me “Sara, is your disease infectious?”. At that time, I just laughed and say “No, it doesn’t”. The lack of awareness, although understandable, is a huge disappointment when someone I confided in is not taking any initiative to understand it.
Stress is another thing that I started to consciously manage. What is the connection between Crohn’s and stress? Well, stress generally affects a person emotionally and mentally as it damages a person’s emotional equilibrium. But it also affects the person’s health. Even a person without chronic disease can feel their health being affected by high stress levels. So, anyone with chronic health issues, such as IBD patients, have higher chances of having a relapse and flare when they are stressed. It is imperative that I recognize my stress inducers, my stress level, my tolerance level and ways to reduce stress so that I do not have chronic flare ups. Although it is impossible to live stress free all the time, I believe that I should try to manage stressful situations to the best of my abilities.
Navigating relationship with Crohn’s is complicated and challenging. Crohn’s has created ups and downs in my relationships with my family, friends and loved ones. In the beginning it was really hard to explain to them my condition. They did not understand the condition or why and how I got this disease in the first place at all. It took a while for my family to accept my condition and now they are slowly getting used to it. They are a great support for me at the moment, and my heartfelt thanks.
Dealing with Crohn’s is tough enough and unfortunately, Crohn’s is not something that we can ignore or that it will disappear one day. Every single day is a challenge for me because I go through physical and psychological pain. I have to survive, improve my quality of life and live my life as normal as possible; I hope more people will become aware of Crohn’s disease, of patients’ struggles, and accept their conditions. Be kind even if you don’t see someone’s struggle, their pain or their decreasing health.
The Difficulty of Finding a Treatment
For the ordinary individual, health is accepted as a given. It’s a part of life that mostly runs in the background like a minimized window on a computer. It’s always running, keeping us alive, and impacting our physical and mental states. Yet again, for most people, it’s rare to directly confront it on a minute to minute, or even second to second basis. Instead, it emerges at the forefront of life either by active and deliberate personal choice, or when something goes wrong. When a previously silent computer program running in the background becomes unresponsive, what was once insignificant becomes a major issue. To a greater extent, when that disruptive program causes our computer to crash and lose all of our work, it’s catastrophic. In a similar way, the typical individual goes to the doctor only on the occasions when their health is compromised by infection, injury, or other issues. Plus, when our health is stable and we are well, the changes we make, like starting a fitness regime, new diet, or implementing mindfulness strategies to our lifestyle, are done by choice.
However, when you live with a chronic illness, health management becomes significantly more complex. For one, chronically-ill patients often do not have the benefit of having a lifestyle defined by stable health. Chronic illness is by its very nature unpredictable. Diseases like Crohn's disease and ulcerative colitis revolve around periods of peaks and valleys - remission and flares. Once again, living with a chronic condition transforms the nature of managing health. The process of searching for, utilizing, and adjusting to a treatment for inflammatory bowel disease, or other chronic conditions, is one of trial and error. Unlike treating the common cold or a broken bone, the path to recovery is much less clear cut. Personally, I have tried various medications across a variety of different medication classes only to discover that they were not effective for treating my particular case of ulcerative colitis. It takes constant monitoring of your symptoms, and a commitment to embracing change to successfully navigate the healthcare system as a chronically ill patient.
It’s a difficult reality that many patients struggle through countless medications, clinics, and treatments before finding relief. Simply put, when you live with a chronic illness, your health is never certain. It’s unlike managing short-lived, common conditions, because there’s no clear timeline. Patients are forced to adjust to a new normal. This new reality is a reality where an individual must persist despite burnout, despite anxiety, and despite certainty. It involves significant sacrifices in one’s lifestyle, and even identity. Confronting health is no longer a special event or a choice, instead it’s a part of the daily routine. I believe this is part of why accepting illness is full of so many emotions, and why fatigue can easily take over. Everyday, patients are fighting a difficult, and often invisible, battle while living normal lives full of other responsibilities. The process, and the challenges, involved with finding and managing treatment do not make this balancing act any easier. Thus, it’s important to recognize the difficult, frustrating, and exhausting experience of patients worldwide. After all, despite illness, set-backs, and struggles, we persist to live lives as friends, artists, and advocates.
The Acceptance and Struggle of a Childhood IBD Diagnosis
Being a kid is supposed to be a whimsical experience that one treasures and wants to have back. We long for those easier, good old days. But, when you are diagnosed with Inflammatory Bowel Disease at the age of 8, those childhood hopes can get lost.
When I was diagnosed with Crohn’s disease, I did not know what it was. I remember telling my friends and them thinking I kept saying “Crow’s disease” (granted, I did have a speech impediment). Honestly, even I couldn't fully understand what was going on with my body. I felt alone, isolated, and trapped in my body. I felt frustrated because of the lack of support I felt from my peers and the lack of communication that I could provide to the people in my life. I felt confused as to whether I was being too dramatic or if I was really as sick as I thought I was. It becomes hard to trust your body and self when—for so long—your symptoms are not understood. Still today, these emotions can flood my body when I think about my diagnosis or even have to deal with unrelated health procedures. The body has a mysterious memory intact.
In response to these events, I have found that I tend to forget things related to it. To be honest, pretty much everything—specifically during my diagnosis phase of life—is most often a blur. Being diagnosed as a child really made me deeply struggle with the faults of reality and mortality and sickness early on. My body is easily triggered by hospitals or doctors. Whether my response bodily or emotional, I cannot immediately make sense of it all at the time.
I often struggle making sense of my diagnosis. Being diagnosed at such an early age, the disconnect between what was real and fake is hard. How could it have such a constant effect on my life when I forget most details surrounding it? It can be hard when you are surrounded by so many people who have such an understanding of their diagnosis and can write such beautiful lessons they have learned when most days I do not even remember what age I was diagnosed at. It is so easy to compare journeys, thinking your IBD is not as bad as the next, or that you feel alone with it. But what we can hold is that we don't have to be positive all the time. It can be painful and we can hold both the pain and the lessons we have learned. We do not have to make sense of our diagnoses. There does not always have to be a bright side to everything and that does not make you less of anything. Everyone has their bad days, whether you see them or not. Just remember that it is okay to struggle, it's okay if not everything makes sense, and we are so happy to have you here.
Planning with Crohn's
Stay with me for this one – I promise it won’t be as boring as it sounds! If you immediately switch off when you hear the world ‘plan’, or indeed ‘regime’ or ‘strategy’, you’re not the only one! There are, however, benefits to planning when you live with a chronic condition like Crohn’s Disease – and more importantly, if your plans become routines, then they’re more likely to become second nature, and you’ll find yourself doing those tasks subconsciously. Here, I will share some of my planning tips, which you may just find helpful. It’s all about finding what works for you so that you can manage to fit in all of the things you want to do, despite your health condition(s).
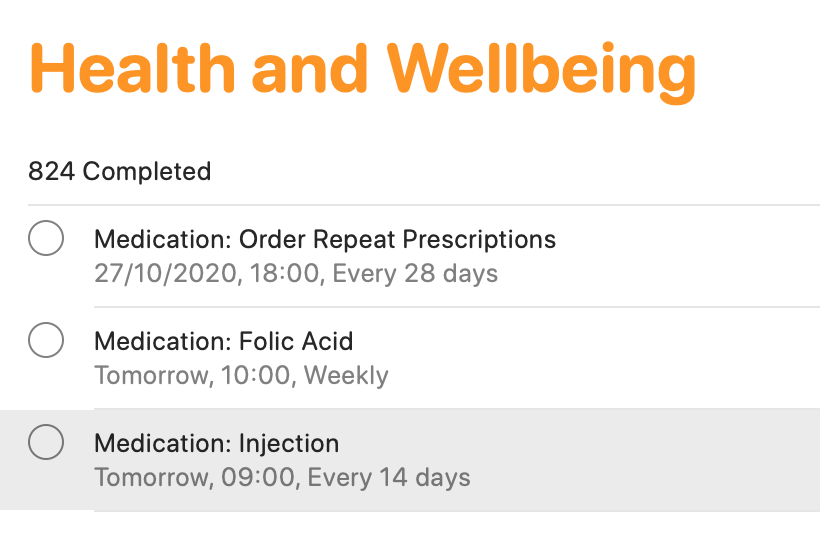
Smartphone apps
There are tons of smartphone apps available to help you keep lists, plan activities and so on! I keep it fairly simple, making use of macOS/iOS Calendar, Reminders and Notes (or the same apps on other operating devices). The calendar function is ideal for noting down all of your appointments. This helps for looking to the future, but also looking back at when and where different events occurred. The reminders app is an absolute lifeline for me. I have separate folders for different activities (e.g. university, health, work, voluntary commitments and so on). I add in activities, and a date/time (or location) reminder. This definitely helps me to keep track of everything that I need to do. If I didn’t, I would definitely forget! From a health tracking perspective, this is ideal as a reminder for booking in my next vitamin B12 injection which takes place every three months, as well as for when I need to ring up my doctor to arrange routine blood tests, when I need to self-inject my treatment, and when I need to order my repeat prescription. You may think that you’ll remember everything, but when you are busy with ‘life’, on top of ‘brain fog’ which many of us can relate to, it’s easy to forget. I know I have done that in the past, particularly when it came to self-injecting my treatment. I would remember that I need it on Tuesday for example, which would be the two-week dose period. However, I would have a busy day at college, would forget when I came home, and then in bed at night, I would suddenly remember, and think ‘I’ll have it tomorrow’. But then tomorrow became the weekend, and before I knew it, it may be a whole week later and I still hadn’t given myself my injection. I knew that was no good, but I just needed to do something about it – which I did!
Finally, Notes are brilliant! Again, I have different folders for a whole variety of different items. ‘Health’ is one of those. I use notes for keeping track of how I have been feeling, as well as for noting down points to discuss with my healthcare teams. I also use notes to keep track of discussions held with healthcare professionals, either face-to-face or over the phone. It’s just another good way to have information at your fingertips to help with your care, while the discussions are still ‘fresh’ in your head.
Scheduling in rest days
We all know what it’s like to live with a condition like Crohn’s – we have so much robbed away from us. As a result, when you are feeling on the better side, you will naturally try to fit in everything that you can. I know that I have been there! Though sometimes, it really doesn’t pay off. That’s why I try to give myself time and space to just ‘do nothing’ – because I know that’s what my body needs. In pre-pandemic times, I would avoid booking in too many back-to-back travels, so that I always had some time to recover. In the current climate, I do my best to block off certain days where I’ll have meetings, keeping overs ‘free’ to do work at my own pace, and also take it easy. It’s all about being in control, as much as possible, so that you give your body (and importantly, your mind) the time and space to breathe.
Leaving the house with everything that you need
Phone. Wallet/purse. Keys. Mask! The list goes on – but it’s really important to have everything that you need to hand. As well as the usual items that most of us require these days, I also have supplies in my backpack and car for every eventuality. This includes painkilling tablets and gel, anti-spasmodic tablets to help with cramps, laxative tablets if I notice a blockage, anti-diarrhoeal tablets if the opposite happens, lactase enzyme to help me digest products containing lactose and the RADAR key to access locked accessible toilets. This list can go on and will depend on personal circumstances. I always find it best to have everything stored in one bag, so you can ‘grab and go’. It may feel excessive, but you will thank yourself later on when you’re not caught short.
Knowing your triggers and avoiding them
Although everyone is different, we all have some kind of trigger which can worsen how we feel. For me, I know that stress is a key trigger for worsening symptoms. That’s why I try to minimise stress as much as is practically possible – although that is much easier said than done! That’s why you’ll generally see me planning to do work well in advance of deadlines, for example, and seemingly ‘being on top’ of everything. In reality, it’s much harder to do, and I do find myself rushing for deadlines still – but at least I have minimised that as much as is practically possible. I am also my own worst enemy. As a perfectionist, I place huge amounts of pressure on myself to succeed and to do everything to the very best of my abilities. While it’s a good quality to have, it isn’t when it impacts on your health. So, it’s really important to be kind to yourself, and to re-evaluate your workload if you find yourself totally swamped and feeling ill. Nothing is worth more than your health.
Do you have any other planning tips which help you to live with your condition whilst getting through life? Let us know in the comments and on social media!
Explaining Chronic Pain
This article is sponsored by Gali Health.
One of the most troubling and tricky feelings of the human condition is pain. It’s the body’s warning signal that something is wrong. It always seems to show up unexpectedly. It’s the world’s worst party guest. Seriously, it could at least bring a party gift, or an extra bag of chips and salsa to share. Instead, it interrupts the flow of midnight ragers and days of routine alike. Pain is the ultimate consumer. It takes, absorbs, and swells, without giving any of itself up. To make it even more complicated, pain comes in more hues, flavors, and shapes than can be counted. Pain is a universal experience, but the experience of pain is unique to each individual.
There is round, smooth, aching pain that rolls around the body all day. There’s sharp, jagged pain that cuts, stabs, and leaves a metallic taste on the tongue. There’s pain that shapeshifts. It howls like a werewolf, then sizzles like the sting from an insect. I could go on, but the list of the types of pain is again endless. That said, living with a chronic illness like IBD means tasting an entire buffet’s worth of pain types. Despite the fact that pain is so specific, and individual, people often try to measure and compare pain. As a chronically ill individual, it can be frustrating to have your pain compared, and rationalized by others. For instance, people will often compare the abdominal pain from ulcerative colitis, or Crohn’s disease to a stomach ache. In reality, chronic pain is much different from everyday pain.
When the pain from chronic illnesses is compared to pain from other illnesses, a large part of the context is ignored. Patients with chronic illnesses and pain have to confront pain oftentimes on a daily basis, and manage pain oftentimes without a totally effective treatment. The pain from a stomach ache, or a stubbed toe will eventually fade, and if it doesn’t, there is generally an effective treatment available. With a chronic illness, no such treatment necessarily exists. There is no timeline for recovery from the pain. Instead, it can be endless and unclear with multiple trials of various treatments required in order to find relief. In essence, chronic pain has no end deadline.
Despite this, the chronically ill often live normal lives everyday. Patients and pain sufferers go to college, go to work, and even to social events despite their pain. It’s especially important to remember this, because for all of its flavors, pain can be quite invisible. Dealing with pain is a challenge, and a burden, but millions of people around the world surmount the obstacle of pain everyday. Accommodations for patients make living with this weight easier, and enable us to be more active members in our communities. Still more work needs to be done to improve the quality of life for those dealing with pain. The compassionate way to treat the chronically ill, is the most inclusive way and the way that eliminates the disadvantages of the disabled. In the future, I hope all pain is treated with the utmost consideration and care for the individual. After all, if that was the case, there would be a lot less physical, and mental pain in this world.
This article is sponsored by Gali Health
Gali Health is an AI-based personal health assistant app helping people with inflammatory bowel diseases (IBD) proactively manage their condition. Gali gathers knowledge from daily interactions and health monitors to tailor support and information to your specific IBD experience.
What to Expect When a Loved One Gets Diagnosed with IBD
Navigating an IBD diagnosis is not easy. It can be messy and emotional and very tiring. The person diagnosed with IBD will be feeling many emotions, probably all at once. But it’s not just hard on the diagnosed individual; it can be very hard on their loved ones as well. It can be difficult to figure out what to expect and what to say and how to act when you find out someone was diagnosed with Crohn’s disease or ulcerative colitis. Hopefully this article will provide some insight into what to expect when that diagnosis happens.
The first few hours and days after your loved one gets diagnosed with IBD can be very confusing. You are processing their diagnosis, while trying to be there for them as well. While everyone processes it differently, there are likely some common reactions you can expect. Here are a few things to keep in mind:
Be prepared to simply be there for them. Whether they want to talk about it or not; whether they want you to accompany them to appointments or infusions; whether they want someone to sit with them while they are sick. And even if they don’t want any of that, make sure that they just know that you will be there if/when they do. Be there for them when they are ready to talk to you. Tell them you are there if they need anything and be ready to back it up with your actions. There is nothing worse than empty words.
Be prepared for them to become experts on their own bodies. They will become very familiar with their symptoms and will likely know when something is not right. Learn to trust that. If they tell you they think something is wrong, don’t try to argue with it.
Be willing to learn with them. For me, I read up a lot on my diagnosis. I read others’ stories, I read articles, I read medical journals. And I wanted my friends and family to understand some of what I was learning. So, be willing to read the articles they send you. Educate yourself on their disease. Don’t be afraid to be educated.
Be ready for the hard days. The days when their medication isn’t working. The days when their Prednisone is making them miserable. The days when they are in the hospital. Not every day will be hard, but some will be. So be prepared when they come. Remind your loved one that it won’t last forever.
Also be ready for the good days! The days when they find out they’re in remission. The day when they try a food they haven’t been able to eat in a while and it goes well. The days when they feel like themselves. Just as the bad days come and go, the good days will come, too.
Be ready for the doctors’ appointment. Especially when your loved one is first diagnosed and they are working to get control of the disease, there will be a lot of doctors’ visits. There will be ER visits and hospital stays. There might be infusions they have to go to on a regular basis. They may or may not want you to come. Be ready to support them either way. With COVID, they may have wanted you to come and you may not be able to. If that’s the case, try to get creative with ways to make them feel like you’re there. FaceTime them, call them, text them. Do something to make them not feel so alone.
Ultimately, be ready for a journey. It isn’t always easy and there will be really hard days. But your loved one is now part of a community that is welcoming and ready to help when they want. There will be people that they can relate to and that can understand them in ways that someone without IBD can’t understand. Encourage them to reach out to people they see on social media. Encourage them to ask questions and not be afraid to speak up. The IBD community is a great one and people are always willing to help!
Navigating a loved one’s IBD diagnosis can be a daunting thing. It is a lot to process and there is a lot of unknown. But by just being supportive and being attentive to your loved one, things will probably go a lot better than you expect them to.
My IBD Life - Ode to Despair
I sat down to write this article with the intent of describing some personal experiences with my family and friends during a period of progressing sickness that eventually led to surgery. It’s very hard for me to segregate various aspects of that time. I was struggling on many fronts. Everything seems so intertwined. I probably would have managed better, if the only thing I had to worry about had been my health. Sometimes, I wonder if I could live through that again. The worst parts of that period were the nights. Serially failing medications had brought me to a point where I was living with severe chronic pain and total incontinence. Every night I would go through a sequence of muffled crying, screaming, and dancing, to wither and end up on the floor like a lifeless body. I did that deliberately to tire myself out and fall asleep. Every night it was the same routine. Some nights, the urge to end it all was too strong to resist. I dreaded the nights and took up a night job to cope. I thought if I forced my mind to concentrate on a job, it would help with the pain. I’d suffocate at work, and even had “accidents” at work, despite wearing diapers. Everyone around me in my home or outside was oblivious to what I did to myself in my room in the dark. My coping mechanisms bordered on the psychotic. I would strangulate my body parts to make them numb. I would try to substitute the pain with another kind of pain by using an excessively hot pad. The pain was too much. The blood was too much. The nights were too long. The thing that hurt more than the pain was that every medication would make a mockery of my attempts to live. Early promising results followed by a rapid decline leading to increased symptoms were a pattern. At my core, I’m not a very hopeful person. My life circumstances have molded me into a deeply introverted and pessimist personality. My mind constantly tries to simulate everything that can go wrong and I try my best to put control measures in place. With this disease though, I was helpless. I read vehemently, but I was not a doctor. I forced myself to cultivate hope with every new medication. However, I always ended up dejected. Sometimes, I felt like a bloody soldier struggling to stand straight, kneeling on the ground against his sword, and waiting for all of it to get over.
As I started reminiscing those nights, my intents changed. I wanted to describe that cycle of hope and consequent despair to someone. It resulted in me writing a poem which I’m sharing here.
They tell me the war is over and we won.
They tell me that the night is at last, gone.
They tell me the sun’s rising on the horizon.
They tell me, they tell me it’s a new dawn.
They tell me the same things again and again.
And each time they say it, I believe them.
I hide from my fears, behind a translucent curtain.
Weak ropes of hope bear the weight of my pain.
Soon it all comes crashing down to the ground.
And I see them again. The blood-hungry hounds.
Dread sets into me as they approach and surround.
Every inch of me bleeds. My screams resound.
And when it’s all over, I look down from the edge.
Frail, pale, broken, and defeated, after the rampage.
No antidote to my ailment, my soul feels caged.
Desperate, I am prepared to embrace the only escape.
“Stop! Don’t!” I hear a voice break the silence.
I recognize the voice. It’s them. Once again.
They praise my resilience. Talk about Providence.
Promise me there’s a reason for my existence.
They look to infuse me with hope and faith.
They tell me tales of the fierce and brave.
Why then I don’t believe what they say?
Oh! It’s because, soon after ...
They tell me the war is over and we won.
They tell me that the night is at last, gone.
They tell me the sun’s rising on the horizon.
They tell me, they tell me it’s a new dawn.
There was a time when I tried to capture my pain in words. I was better at writing then. With time, the writing started to feel like a futile exercise. The nights never went away. Instead, I now try to repress those experiences in some corner of my brain as I have done with other traumatic incidents that I have lived through.
My doctor once told me that there were only 2 patients other than me under his care, with a severity of disease that was similar to mine. I felt sad, but then I realized it’s a good thing that more people do not go through such experiences. However, I’m sure there are enough like me in my country which has a population of 1.3 billion, but I’m not sure if everyone is as lucky as me. The mental health of patients with Inflammatory Bowel Disease has never been a priority in the Indian Healthcare system. It’s time that we begin to provide holistic support to young adults with inflammatory bowel diseases to enable them to manage this disease better and come out of the experience with as little residual trauma as possible.
Please stay safe and take care. See you next month. :)
IBD and Anxiety
When you are first diagnosed with Inflammatory Bowel Disease you learn quickly that the brain and gut function as one. They are deeply connected. Even if you don’t have IBD, you can look to feelings like butterflies in your stomach when you are nervous, excited, or in love. IBD has given me the superpower of identifying an instinctual trust of my gut. One thing you commonly hear when talking about how to manage your IBD is that you have to manage your stress levels. Since the brain and gut are so connected, the chances that a flare up will occur when you’re stressed are high. Truthfully, being able to manage your stress is a very privileged thing to be able to do and that’s a conversation that needs to be had. Outside forces and systems of oppression exist heavily in our world today. We are not functioning in a world that allows you to thrive and prioritize both your mental and physical health. For most people, there is always a tremendous amount of stressors that you cannot escape. Things like finances, unstable households, going to school, and working all cause a great deal of stress.
Today, I want to specifically talk about how managing stress levels and IBD feels increasingly impossible when you have clinical anxiety and/or PTSD, as these are so often linked with IBD.
I was diagnosed with IBD at a young age. My physical health was always prioritized over my mental health. This was more pronounced, I think, because mental health is not a thing that is necessarily often invested in for young children. As a child, it was very difficult for me to identify what I was feeling and what triggered these feelings. Specifically, with my anxiety, I did not know what a neutral state of mind meant. I didn’t know what my anxiety looked or felt like till around my sophomore year of college. After going on anxiety medication for a bit, I was able to understand what intrusive thoughts were and how they occupied my life.
The baseline for my anxiety is intrusive thoughts, but it can also manifest itself in different ways just based on the things I am doing in my life at the time. For example, my anxiety can manifest itself in ways such as crying in social settings, having an obsession with time (i.e. constantly looking at the clock or leaving hours early for events), and, when things are more extreme, staying in my room for days on end. For me, it is so important to specifically state how my anxiety manifests because for so long I did not know what it meant. I think it is important that we normalize talking about everything that anxiety can bring with it, not just generalizing or downplaying it. So often, I think anxiety is talked about in very loose terms and given very simple fixes for how to “handle it.” This, in return, can oftentimes belittle the situation.
When these more intense and intrusive moments occur, my IBD flares up. So, I often question how I am to manage my stress when I often cannot control my anxieties. In the past, I would become stressed when I experienced my anxieties because I did not know what was wrong. Now, they still stress me out, even though I know that it is anxiety.
For me, and I think many others, anxiety is something that I have to constantly cope with on the daily. If I am not ten steps ahead of it, it will simply swallow me whole.
IBD and anxiety can feel overwhelming and scary, but what has helped me is knowing that I am not alone. Having these two conditions together is not uncommon, and what feels very isolating and full of despair is not the case. Medication has helped me in the past and therapy is a forever process for me. I also keep a bullet journal of coping skills I have used in the past - identifying coping mechanisms that worked and ones that did not. This list gives me a place to turn to when I feel as though nothing could help and it's easily accessible. I have also found solace in being in a community of people who understand. Explaining anxiety or IBD to someone who has not gone through it can be very exhausting and this goes for many other varying identities as well! When I do find the energy, making art is another space for me to process my anxiety, whether that be through a conceptual piece or just painting a canvas with one color over and over again.
What are ways you cope with your anxiety?
Judging Symptoms with Crohn’s
Sometimes, it feels like all gastro symptoms are inflammaotry bowel disease (IBD)-related… especially being symptomatic with IBD for so long. However, it’s not always case – which can cause a great of confusion, as well as making life just that bit more complicated!
As well as Crohn’s disease, I also have gastroesophageal reflux disease (GERD), irritable bowel syndrome with constipation (IBS-C), an internal rectal prolapse and lactose intolerance. I was diagnosed with Crohn’s disease in 2008, after several years of experience gastro-related symptoms. So, at that point, I assumed that everything I had experienced was the result of Crohn’s. What I failed to realise, and what wasn’t explained very well at the time, was that I also had GERD. I was suddenly prescribed all of this medication, without being properly informed of the purpose of each different medication.
Over time, and with the right treatment, I became more informed, and I was able to get my Crohn’s disease under control, to the point where I was deemed to be in clinical remission. This was concluded by considering blood tests for inflammation (CRP and ESR), colonoscopy and gastroscopy results, small bowel MRI scan results and faecal calprotectin results, each of them done at different frequencies over different periods of time. This happened gradually over a few years, and in the process, I learned more and more about my body. However, I began to struggle with more gastro-related symptoms, which I initially thought were a Crohn’s flare, but soon realised were not exactly the same as before my Crohn’s diagnosis. I felt bloated and constipated, I had abdominal pain, and I was passing mucus. It became clear that I most likely had IBS-C. The problem I found with IBS was that there was no quick and easy fix for it – not that there has been a quick and easy fix for Crohn’s disease, but at least I was able to take some treatment which helped control the inflammation. With IBS, I felt very much in the dark. Recommendations were an anti-spasmodic to relieve cramping, laxatives to ease constipation, and avoiding foods which seemed to make me ‘worse’. I watched what I ate very closely, and soon identified certain green vegetables as a trigger, as well as milk products, which I tried to reduce.
Little did I know, but the milk products weren’t just a trigger for worsening my IBS symptoms, but I was also lactose intolerant. I was diagnosed in 2015 – some seven years after my Crohn’s diagnosis. This only happened after one doctor felt there was something else going on and decided to test for lactose intolerance and Helicobacter Pylori infection – and thank goodness they did! I’ve managed to cut most forms of lactose completely out of my diet since, and when I can’t, I have found a lactase enzyme supplement I can take immediately before eating or drinking something containing lactose, to help me avoid those unpleasant symptoms.
I thought that was going to be it when it came to gastro problems. Then, something else came along! Originally blamed on my IBS-C, I noticed I was struggling more with constipation, despite eating a balanced and healthy diet, and doing everything else ‘right’. A couple of healthcare professionals didn’t really acknowledge my perspective, and just said I need to take laxatives permanently – something which I do take, but often feels like a ‘quick fix’ or ‘cover the wound with a plaster’, without understanding the underlying reason for these changes. Many blame IBD, plus IBS for constipation, without necessarily looking further. It sometimes feels as though assumptions are an easier option in the medical world, but not for those of us living with these symptoms. Moreover, I had observed changes beyond those I had learned to notice by living with IBD and IBS-C.
Cutting a very long story short, I ended up going for a proctogram which revealed I had an internal rectal prolapse – which is basically when your rectum folds in on itself. It wasn’t the most dignifying procedure – much like most gastro-linked investigations. Dignity often goes straight out of the window! However, this finding did explain the sharp shooting pains I had been having in my rectum, as well as the mucus I had been passing, the ‘fresh’ blood I had noticed, and why it sometimes felt as though there was a physical obstruction – because there was. The verdict was ‘there’s not much we can do’ – something I think we’re all too used to hearing. There are surgical options, but they come with risks and they more or less said they would not be considering that option for somebody of my age. So, I was sent away with pelvic floor exercises, and the notion that ‘I just have to live with it’ – which I do. At least I received an answer for the symptoms I had been experiencing, even if I don’t have an answer as to ‘why’ I have a rectal prolapse. My current hypothesis is that it is something to do with hypermobility, which has consistently been overlooked – but that’s a whole different story!
All of these different symptoms, and the conditions subsequently diagnosed, have taught me so much. I have learned to really listen to what my body is telling me – which is not easy but does improve with time. I’m not always right, but my judgement certainly seems to be stronger now, after all of these years with IBD, IBS-C, GERD, a prolapse and lactose intolerance. I am much better at distinguishing as to ‘what’ is causing ‘what’ – although it’s impossible to always be ‘right’! You just tune into what you are feeling, almost like detective work. You place pieces of the puzzle together to help you build the picture of what you think is happening. Your previous experiences and your observations guide you, alongside being proactive in terms of knowing clinical indicators, recognising new triggers, stressors or symptoms, and then being proactive in seeking the right input from the right healthcare professionals. It comes more naturally after years of having to take things into your own hands to get answers. For example, I now know that the abdominal pain and cramping that I frequently experience is when I am perhaps a little constipated as a result of IBS-C and my internal rectal prolapse; so I adjust certain parts of my diet and take additional laxatives when I begin to notice patterns changing, early on. Likewise, the ‘whale’ noises and ‘washing machine sensation’ immediately indicate that I’ve consumed something containing lactose without realising – like the time I ate a gorgeous cheesy pizza, and then realised I hadn’t taken my lactase enzyme… I suffered for the next few hours!
These conditions, in one sense, sensitise us to be more receptive to how our bodies work. I don’t think I would have been as knowledgeable or as ‘switched on’ as I am if I hadn’t been diagnosed with them – and I wish more people recognised this, particularly certain healthcare professionals. I often have grievances with professionals who rely solely on certain clinical indicators for disease remission. For example, those who just use CRP as an indicator as to whether you are in remission or not. This has happened to me in the past when I was evidently in the middle of an IBD flare, but at that point in time, I was not confident at self-managing my health. As it turned out, my faecal calprotectin was off the scale, and so some additional treatment helped me out immensely. What did I learn? Nobody knows my body better than myself. Healthcare professionals can help me the most when they listen to what I am saying, acknowledge my expertise, and then work with me to identify what is really happening, and then plan with me as to what to do to help manage symptoms so that I can get on with my life, and most importantly, have a good quality of life. So, when anybody questions what you are thinking or feeling, remind them of this point, and hopefully, they will change their approach so that it is supportive, rather than a hindrance.