NEWS
How to Start a Food Diary
Dear Diary,
Sometimes when I eat it feels like a herd of angry buffalo have taken up residence in my gut. The rumbling, the pain, and the regret are all too familiar at this point. Maybe I just shouldn’t eat at all. Maybe that would be best. I wish it could just stop…
Okay, I might not be talking about that type of diary, but I’ve had many days in my Crohn’s journey where that could have described me. Like many people with Inflammatory Bowel Disease (IBD), I have a frustrating mix of good days and bad days. It always baffled me how I could feel good one day, but terrible the next. I wanted to know why. This started my journey of paying closer attention to what I eat, and in turn, keeping a food diary.
Why a food diary?
Our environment is everything we come in contact with on a daily basis that isn’t us. The air we breath, the things we touch, and the food we eat all make up our outside environment. If nothing in our environment impacts a disease, it should feel the same every single day. For me, and many others with IBD, this just isn’t true. In this case, we must start looking at our environment as a source of triggers for our disease.
One of the largest parts about how we interact with our outside environment is what we eat. Every day we eat a variety of different foods, from a variety of different places, that have a variety of different health effects. For me, food was an easy place to start to try to figure out some of my disease triggers. I know what I am eating every day, so why not try to see if there is any connection between what I eat, and how I feel. This led me to food journaling, and it has been an invaluable resource in helping me navigate and manage my own disease. It has given me power.
Research also backs up this idea. In one study done in 2016, one group of Crohn's patients was told to exclude either the four food types they had the highest antibodies to, while the other excluded the four food types they had the lowest antibody to. The group that excluded the foods types to which they had the highest antibodies had significantly lower disease activity and significantly higher quality of life.1 We might not have access to antibody testing, but we can certainly try to figure out what foods are worsening our disease and quality of life.
How to write a food journal
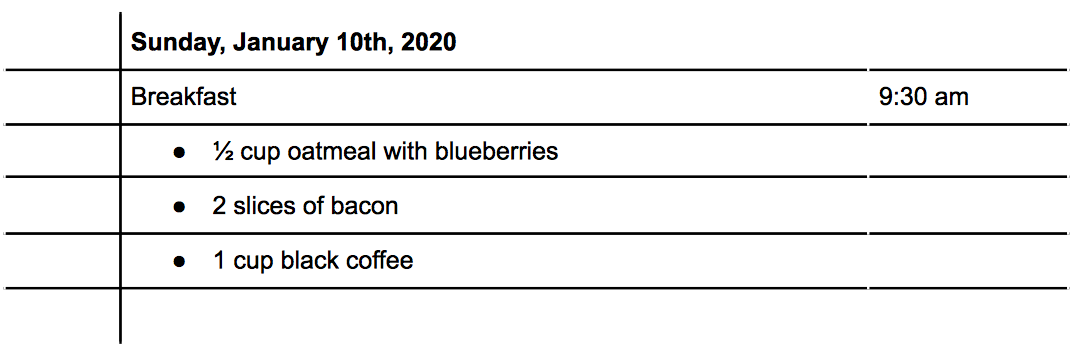
There are three main things to consider when writing a food journal: what you eat, the time you eat, and how much you eat. With these three written down, you will be able to better make connections between foods and symptoms. Let's do an example: For breakfast this morning, you ate a bowl of oatmeal with blueberries, some bacon, and a cup of coffee (I know, I know, coffee isn’t exactly known for its stellar track record in collaborating well with IBD, but it's a made up example!) How would that look?
Tracking Symptoms
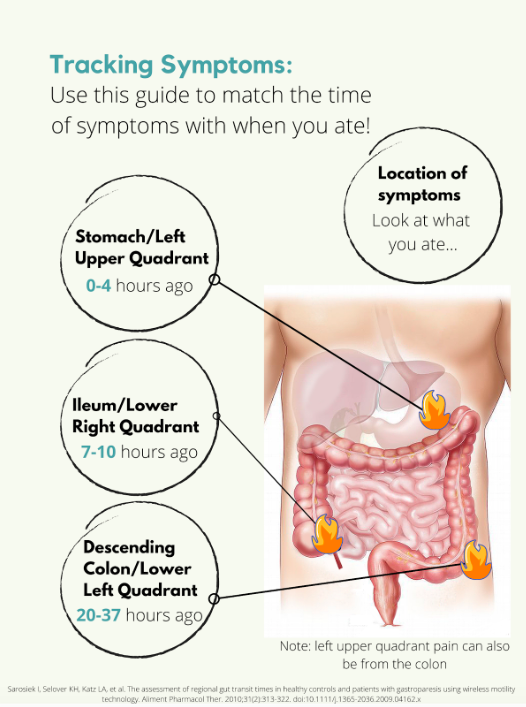
Symptoms are a little trickier. Say you have some pain in your lower right abdomen, how do you know what meal might have triggered you? Was it the meal you ate 5 minutes ago? 4 hours ago? The day before? For this we need to know a little bit about how long food takes to get to each different part of the intestines, also called the intestinal transit time. In a normal, healthy adult the following is accurate:
But what if you’re flaring? Diarrhea, inflammation, stricturing, and other aspects of a flare can all impact the amount of time it takes for food to get to the finish line. Some studies have been done on intestinal transit time in IBD patients, with most finding that the intestinal transit time is longer in IBD than in normal healthy subjects.2,3,4 In one patient with Crohn's disease, it took 156.2 hours for one meal to pass through. Talk about taking the scenic route! Like many other things with IBD, you are going to have to take an individual approach and problem solve to figure out how to best match symptoms and meals.
Resources
Tracking food can be done in something as simple as a spiral notebook, but there are also other options available. Here is a list of some apps you could use instead of a physical journal:
mySymptoms Food Diary & Symptom Tracker (Lite) by SkyGazer Labs LTD
Food Diary by WeCode Team
Cara Care by HiDoc Technologies
References
Gunasekeera V, Mendall MA, Chan D, Kumar D. Treatment of Crohn’s Disease with an IgG4-Guided Exclusion Diet: A Randomized Controlled Trial. Digestive Diseases and Sciences. 2016/04/01 2016;61(4):1148-1157.
Andersen K, Haase A, Agnholt J, et al. P-113 Gastrointestinal Transit Times and Abdominal Pain in Crohn's Disease. Inflammatory Bowel Diseases. 2017;23(suppl_1):S40-S41.
Fischer M, Siva S, Wo JM, Fadda HM. Assessment of Small Intestinal Transit Times in Ulcerative Colitis and Crohn's Disease Patients with Different Disease Activity Using Video Capsule Endoscopy. AAPS PharmSciTech. 2017;18(2):404-409. doi:10.1208/s12249-016-0521-3
Haase AM, Gregersen T, Christensen LA, et al. Regional gastrointestinal transit times in severe ulcerative colitis. Neurogastroenterology & Motility. 2016;28(2):217-224.
Starting a Healthy Relationship with Food
By Erin Ard
What should I eat during a flare-up? What should I eat to stay trim? What should I eat to be healthy? What even CAN I eat? Every day I'm plagued with these questions. Even more aggravating, none of which have an easy, clear-cut answer. But having had experience fumbling over meal-planning and studying nutrition, I've learned how to better navigate my eating habits.
Planning and preparing healthy meals for yourself can be an exhausting, time-consuming, and sometimes expensive, process - especially for college students. Now if you throw in food allergies, intolerance, or chronic illness this process can get MORE complicated! Having inflammatory bowel disease (IBD), myself, I know how challenging it is to eat healthy within your own food restrictions; especially if you don't have a good understanding of nutrition, gastrointestinal disease, or what your restrictions are! My disease has been in remission for several years now, so my food limitations aren't as strict as someone having a flare-up, and I still have trouble. For those who are new to the game, IBD is a class of autoimmune diseases that causes inflammation along the GI tract when the disease is active, and can hinder nutrient absorption. With Crohn's disease, a common form of IBD, there is no specific diet to follow to control symptoms. This is probably the most annoying thing you've read today, but I better let you know now.. According to the Academy of Nutrition and Dietetics, we only know of foods to avoid - foods like dairy, high fiber grains, alcohol and certain spices, since these tend to aggravate an inflamed bowel.
Being the nutrition major I am, I get to learn about the Dietary Guidelines for Americans (DGAs). These are a great resource for curious readers wanting to eat healthy and live an active lifestyle. They lay out simple and easy recommendations to help prevent chronic illness, e.g. diabetes or obesity. These illnesses have become more and more prominent in the U.S. and have direct ties with diet. But what about the many other nutrition-related diseases with not-so straightforward ties? Unfortunately, the DGAs aren't designed for all bodies. The research used to develop the recommendations use “healthy” test subjects, of course, not those with chronic illness already. If you have a chronic illness, you’ll need to take extra care to find your ideal, health promoting diet. Better start doing some research yourself or see a registered dietitian! Or try out this idea you've probably never heard before, a food diary! …
Taking extra care in regards to your diet is especially important with IBD. In Crohn's disease specifically, inflammation along the digestive tract can cause nutrient deficiency. Inflammation hinders absorption of important nutrients, vitamins, and minerals; putting you at a higher risk of malnutrition than your healthy roommate. Eating the right nutrient-rich foods and eating enough of these foods can make-or-break living healthy with IBD. All of this in mind, the DGAs are still an easy “go-to” to help you learn about what makes up a balanced meal and why. In the rest of this article, I want to help you navigate the DGAs and share my own troubles with forming healthy eating habits.
Navigating the Dietary Guidelines for Americans with IBD
When comparing the DGAs and what is good or bad for a person with the common IBD form of Crohn’s disease, there are a few noteworthy similarities. For instance, limiting saturated or trans fats, simple or added sugars, sodium and alcohol are wise choices for everyone. They also seem to focus on getting a variety of vegetable and protein choices, emphasize fiber, and recommend lower fat options for dairy. Here you need to be careful. As noted before, certain sources of fiber can hurt a person with active disease. In other cases, fiber can be very beneficial for a person with Crohn’s to add fecal bulk, when the disease is in remission (i.e. under control or without symptoms). It's important for you to understand what foods are necessary for a well-balanced diet and what foods impact your disease management. The DGAs give a great outline, but your personal nutrition plan should have the final say in deciding what to make for dinner.
Dietary Guidelines for Americans 2015-2020
1. Follow a healthy eating pattern across the lifespan.
2. Focus on variety, nutrient density, and amount.
3. Limit calories from added sugars and saturated fats and reduce sodium intake.
4. Shift to healthier food and beverage choices.
5. Support healthy eating patterns for all.
My Relationship with Food
All of this information I have outlined is great and all, but I haven't touched on the emotional aspects of eating yet. Eating is heavily tied to the emotions I experience in a day. My mind bounces back and forth so much in a day when I think about food, eating, how I feel, how my gut feels, how much time I have before my next class, and whether I even have the energy to fix a meal up.
I eat when I’m sad and eat when I'm happy. I'll make a great meal to celebrate an accomplishment or make comfort food if my gut hurts. If I have an important event to attend, I will forego eating entirely to prevent symptoms. If I’m sad or stressed enough, I will also not eat, and wallow in my own pity. It’s confusing and raw, and I don’t understand my eating habits most of the time. Like I said, eating is a heavily influenced by my emotions, so how I feel about my Crohn's or about myself will impact what and if I eat anything. Unfortunately, I've discovered that a majority of emotions I experience will have me make bad decisions about food. But pausing to understand why I make these decisions and what fuels these emotions, has helped me to better understand myself. All of this aside, I love making food.
Striving for Progress
I used to have so many misconceptions about food. The biggest misconception I had to overcome was what I needed to eat to be healthy and what I should eat to look good. As a teen and throughout college, I was more absorbed in looking good, being thin, and keeping belly small. Not maximizing my nutrient intake by eating whole foods and managing my disease resurgence.
I used to be influenced by fads and testimonials - "stay away from dairy for clear skin", "stay away from breads and pasta and sugars to shrink your belly", etc. Everything affected me. Every headline I saw or piece of information I was told. Any advice I was given. Everything I interacted with tried to influence my thoughts, opinions, actions, and lifestyle. Here I thought I was being educated. I never realized I was depriving myself more than helping.
What I’ve been learning is that nutrition is not black and white. The world will try to convince you that there are foods you should not eat for X and foods you absolutely need for Y health benefits. Sadly, this isn’t true. There isn’t one perfect diet plan out there for everyone or for XYZ benefits. Nutrition is much more complicated than that.
With all of this in mind, I would say that right now, I have the healthiest relationship with food I've had in a long time. Studying nutrition was a major player, but I also must give credit to being mindful every day. Being mindful of my cravings and urges has helped me stay away from flare-triggering foods. And I make progress each day deconstructing any false beliefs on what I see as a "healthy" food for me.
My message to you is to educate yourself, learn about food, learn what foods you tolerate, and strive for a healthy relationship with food.