Like millions of people around the world, I am doing my bit to control the COVID-19 pandemic, as well as my own health, by staying at home. What seems like torture for many is actually a relief for me – even though I may be getting a bit fed up of being forced to stay in after a few months.
Having followed posts on social media over the last few weeks as more and more countries have imposed ‘lockdown’ measures, I’ve grown increasingly concerned for people’s physical and mental health – having quite literally seen people breakdown and unable to cope after a matter of days cooped up in their homes. For some, they’ve never had to experience being forced to do something they don’t instinctively want to do. For others, it reignites the memories of past traumas when they were forced to stay at home – perhaps during their diagnosis of IBD. But finally, for some, home isn’t the safe place that it is for many of us, and we need to recognise that and try to support those individuals as much as possible.
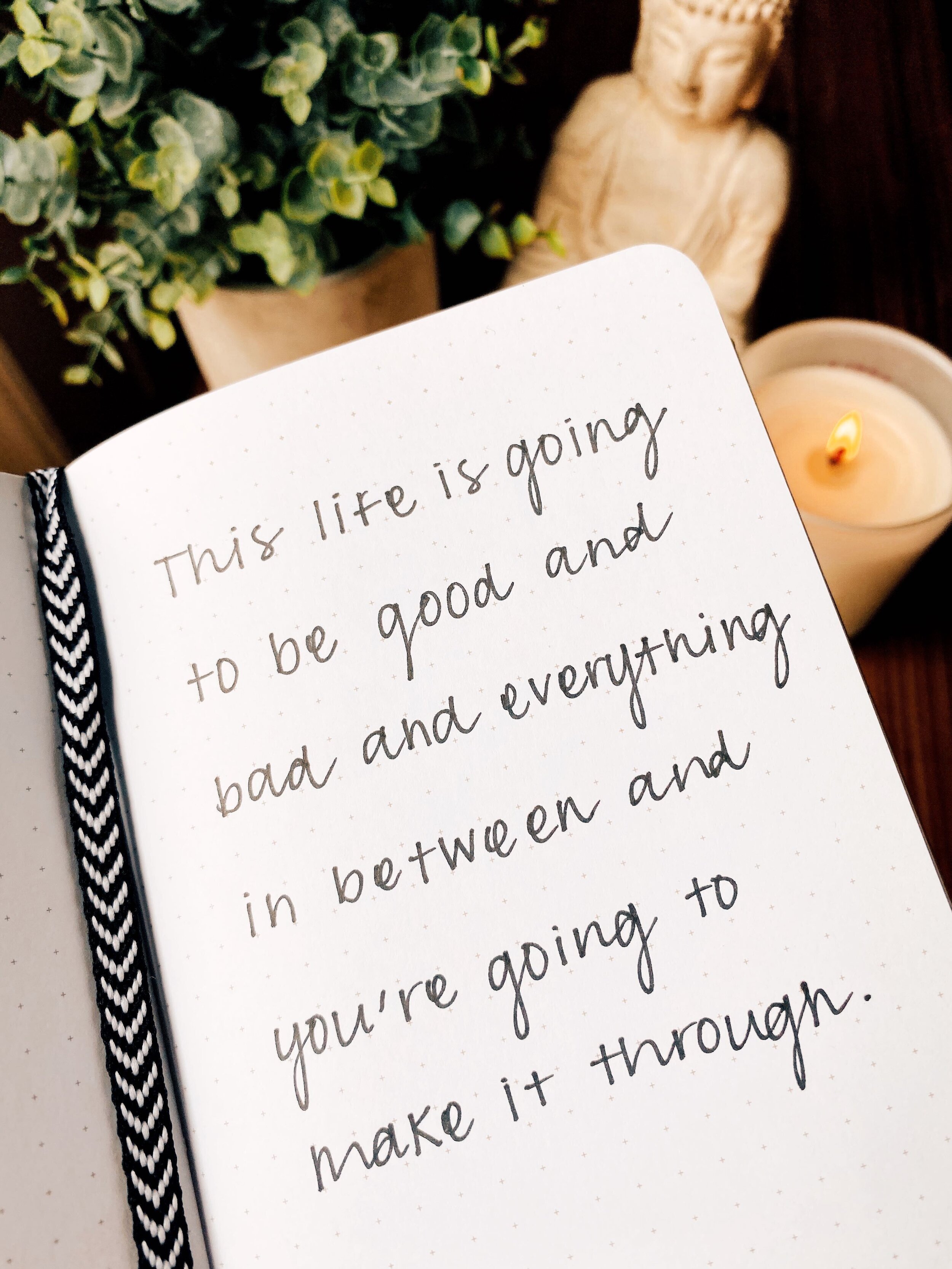
During these unprecedented times, we’ll experience a whole raft of emotions – fear, anxiety, anger and frustration being right up there at the top. However, being the optimist that I am, I think there’s going to be an awful lot of things which society will learn from this pandemic as a whole – and even more things which we’re going to learn as individuals, which will make us re-evaluate our lives and actions – hopefully for the better.
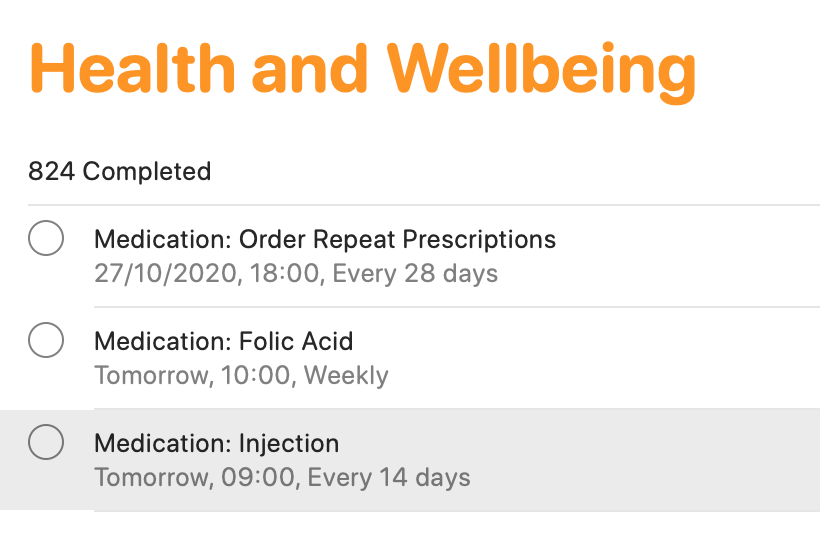
Nobody likes being told that they need to do something – it goes against our instinctive behaviour to be social and independent. However, it’s for our own good. As somebody taking biological immunosuppressive treatment to manage my Crohn’s disease and arthritis, I know that I am at an increased risk of complications if I was to contract the coronavirus. If I have no contact with people, then I’m dramatically decreasing my risk of contracting the virus – as well as limiting my need to rely on healthcare services which are going to be stretched beyond limit in the coming weeks and months. To be fair, being at home has not bothered me one bit – I’m quite enjoying it! I have had PLENTY of opportunities to be used to this though. Throughout my childhood, I was forced to spend more time at home because of ill health, and in recent years, I’ve had no choice but to stay at home more to look after my mum. These experiences have fortunately taught me a few lessons for life. Aside from feeling happy and safe at home, my experiences have taught me to be comfortable with my own company – something which many people struggle with. They’ve also taught me to appreciate what really matters in life – your health and your loved ones, which more and more people are slowly starting to appreciate.
While I’m coping really well, I appreciate and empathise with others who are struggling – which is nothing to be ashamed of. It’s at times like this when everyone is reminded that we’ve got to look out for each other. My door (metaphorical of course at the moment!) is always open, for people who want to chat, rant, scream, cry or sing – so please reach out to me if you just need to talk. I also thought this could be an opportunity for me to share some things which work for me while staying at home. They may not work for you, but it may be worth giving them a try!
Routine or no routine – that is the question
Some people love routine and structure to their days; others much prefer randomness! There is no right or wrong answer – you’ve just got to find what works for you. Despite being particular on a lot of things in life, I’m one of those who I guess ‘sits on the fence’ with this one. My working week tends to follow some kind of pattern, though I’ve learned to keep things fairly flexible, to fit around me. Some days, I really don’t feel like doing much, so I’ll take it easy. Other days, I’m on it from the get-go, and will fit in tons of things. The most important thing to remember is find what works for you!
Finding your activity regime
Keeping active has never been more important! Here in the UK, people are allowed to go outdoors for one form of physical activity per day. I’ve decided to not go beyond my house, for obvious reasons, and so I’ve dedicated time every single morning to finally get back into yoga – which I’m absolutely loving after nearly three weeks of practice now. It has taken the current situation to force me into practicing something until it becomes a habit – and I certainly feel better for it now. Yoga is one of those forms of activity which is great for those of us with joint problems, since you can do as much or as little as you want! I’ve been using the Down Dog app, which has a guided instructor taking you through things. Not only does my body feel better for doing it, but my mind is also feeling clearer. It has forced me to slow down, focus on myself, and ‘be’ in the present. Yoga may not be your thing, so find something that is – at least give something a try, and if it’s not for you, move on to the next!
A dedicated space to work
Having a dedicated space to work is really important. I have my computer set up on a desk in my bedroom, with the correct set up for my posture. There’s also plenty of space for the textbooks, papers and other materials to be alongside. It helps for you to have somewhere to go where you can focus solely on what you’re trying to do, which also works when you want to leave your work alone and think about something totally different!
That being said, variety is also important, especially when you’re sat in the same spot, looking at the same screen (and the same wall behind it for me) more or less every day. So, I’ve agreed with myself to use my desk as the place where I’ll write my PhD thesis. For everything else, such as dealing with other emails, charity work, and other computer tasks, I’ll use my laptop at different places in the house. Sometimes it’s on the bed, or at the dining table, or sat on the sofa, or even in the garden! These aren’t ideal places to be, especially for your posture, but it’s sometimes nice to have a change of scenery.
Keep yourself fed and hydrated
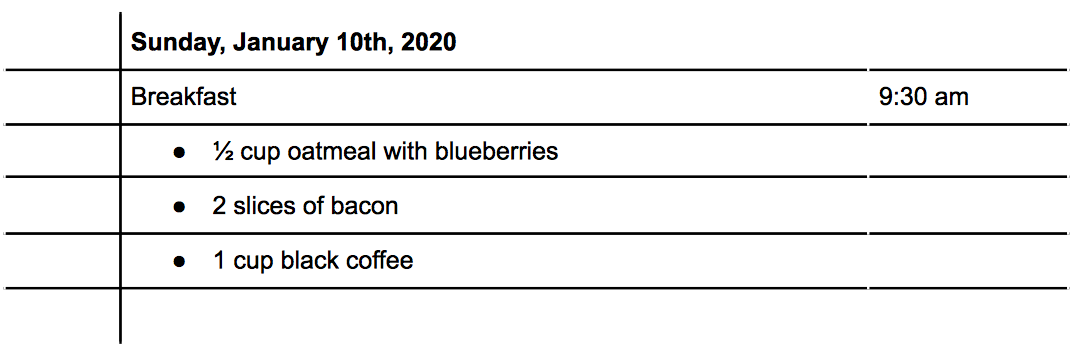
While some people may find that they eat and eat and eat while they’re at home all the time, I’m actually the exact opposite! Especially when I am working, I often slip into the habit of doing ‘just a bit more’… and before I know it, it’s 4pm and I’ve still not had any lunch – which is no good! So, I’m really disciplined with myself now and ensure that I always set time, away from the computer, to have breakfast, lunch and dinner. Making sure you keep yourself hydrated is also really important – which may mean cutting back on the coffees! I’ve switched everything to decaf now so I can enjoy a cuppa without making myself more dehydrated. I’ve also been tracking my fluid intake on my Fitbit app (as well as calorie intake) which does force you to keep up with what you should take each day.
Take breaks, and don’t feel guilty
This is a big one! You may feel under pressure to be working every hour while working at home – but that really doesn’t work. I tend to break my day up with breaks here and there – sometimes it may just be going to the kitchen to get something to eat or drink, but sometimes it could be 30 minutes or an hour spent watching some TV, or reading, or listening to some music. Whatever it is, make sure you do it! You’ll find you work so much better during short, focused periods of time, when your mind can be on the task you’re working on.
Stay connected with others, as much or as little as you want
It’s really important to stay connected with loved ones, acquaintances and colleagues, especially at times like this. I often speak with family members and mum’s friends several times a week over the phone, just like I chat to our neighbour over the fence when we’re both near the side door. Friends tend to message and video call, which is always nice. We have to look out for each other. It’s also fine to sometimes switch off from the outside – we need that too. I sometimes ignore phone calls during the day, especially when I’m busy working. Keeping connected is important, but I also have to work at the same time, so multiple interruptions each day for an hour phone call at a time isn’t always helpful! Don’t feel guilty – I usually drop them a message to say I’ll call them later, unless something is wrong!
Making the best of a bad situation
Nobody would wish for what’s happening to the world right now – but sadly, a lot of it is out of our control. The control we have is to follow guidance, stay at home, limit our contact with others, and ensure we act responsibly when it comes to shopping and using healthcare services. What we can control is our thoughts and actions. It’s not easy by any means, but it is possible. How can you make the best of a bad situation? What can you now do that you’ve been putting off for ages? How can you use this time wisely to focus on yourself and your loved ones? These are all things that are in our control. Whether you take some time to slow down, or pick up a new hobby, or even plan for the things you’re going to do when the world comes out of hibernation – they’re all things that can help to pass the time. Never let the things you can’t do stop you from doing the things you can do!