NEWS
Mental Health & IBD Series
by the 2025 CCYAN Fellows
This month, some of our fellows worked together to share perspectives on mental health and IBD. Check out their articles and videos on this topic below!
Insights from Beamlak (Ethiopia), Aiswarya (India), and Lexi (U.S.A.)
Living with inflammatory bowel disease (IBD) is never just about physical symptoms. It impacts mental health, education, relationships, and self-worth. For many patients, the emotional toll can be as heavy as the physical pain. We came together to explore the connection between IBD and mental health, and each of us shares a different perspective, facts, lived experiences, and personal reflections. Together, they form one message: mental health in IBD care is not optional, it is essential. We wanted to show that IBD is both a physical and mental health journey. Data highlights the need for better systems of care, and personal stories remind us of the resilience and strength it takes to keep moving forward. Together, we call for greater awareness, compassion, and support for every person living with IBD.
Read their perspectives:
Facts we Can’t Ignore - Lexi
Diagnosis is a Light, not a Lampshade - Aiswarya
“Let it” - My Rule for Living with IBD - Beamlak
Insights from Akhil (India) & Alexis (U.S.A.)
Akhil & Alexis (alongside 2022 CCYAN Fellow Maalvika & CCYAN’s Program Manager Rosa) presented about the intersections of Chronic Illness, Mental Health, and Cultural Considerations at the 2025 Bridging Voices, Building Futures: Youth Innovation in Mental Health Conference (hosted by Generation Mental Health). View the presentation below:
Check out more of our 2025 fellow’s articles and videos on other mental health topics:
What it’s Like Working Through Phobias - Kaitlyn Niznik
Through (on Stigma, Shame, and Talking about IBD) - Michelle Garber
God of Small Things: A Crohn’s View (on Stigma and Connection) - Rifa Tusnia Mona
IBD & Grief by Akhil Shridhar
Internalized Stigma in IBD, Mental Health, and Quality of Life by Aiswarya Asokan
Mental Health & IBD (An Infographic) by Lexi Hanson
The Facts We Can’t Ignore (Mental Health & IBD Series)
by Lexi Hanson (Missouri, U.S.A.)
According to the American Gastroenterological Association (AGA), 35–36% of IBD patients report anxiety or depression—far above national averages. Yet, too often, providers prioritize physical health while overlooking mental health needs. Supporting mental health is not a luxury for IBD patients—it is a necessity.
What are some supports that can make a difference for Young Adult IBD patients?
Embedding mental health professionals (psychologists, social workers) in IBD care teams.
Routine mental health screening for young adults.
Coping toolkits to build self-advocacy, communication skills, and emotional resilience.
Extending transition support to age 25, not just 18–20.
Availability of peer and lived-experience communities for validation and advice.
Access to reliable information tools about nutrition, travel, accommodations, relationships, fatigue, and brain fog.
IBD-aware university services: bathroom access, class accommodations, and counseling.
Policy reforms to ease insurance challenges and improve navigation.
Education on ADA rights and workplace accommodations.
Self-compassion training to protect mental health.
Check out Lexi’s July post for more facts about Mental Health & IBD!
Photo from Unsplash.
“Let It” — My Rule for Living with IBD (Mental Health & IBD Series)
by Beamlak Alebel (Addis Ababa, Ethiopia)
Living with Inflammatory Bowel Disease (IBD) is a journey no one truly understands unless they’ve walked it themselves. It changes your body, your mindset, your lifestyle — and even your identity. Over the years, I’ve discovered a rule that helps me rise above the noise, pressure, and pain:
“Let It…”
It reminds me to stop fighting what I can’t change and instead make peace with it — to keep breathing, keep moving, and most of all, keep living.
Let It Be What It Is
IBD is unpredictable. One day you feel okay; the next, you’re back in the hospital.
I remember one exam day when the classroom was overcrowded. I had followed every rule—no phone, fully prepared—but when I arrived, every desk was already taken. There was no seat left for me.
It wasn’t a flare. I had come ready to write the exam, but the conditions made it impossible. I felt angry and frustrated—I had put in the effort, yet I was turned away by circumstances beyond my control. Missing that exam hurt deeply, not only academically but also emotionally. Still, I whispered to myself: “Let it. Everything has a reason.”
Let People Say What They Want
“You don’t look sick.” “Are you sure it’s that serious?” People don’t see what happens behind closed doors — the fatigue, the pain, the hospital visits. Their words used to cut me, but I’ve learned: “I don’t need to prove my pain.”
Let Yourself Say No
There are foods I can’t eat, events I can’t attend, and expectations I can’t meet. I used to feel guilty for saying no, as if I was letting people down. Now I know: “Let yourself say no. It’s not weakness — it’s wisdom.”
Let Hope In
On the hard days, hope is my medicine. Sometimes all I can say to myself is: “Tomorrow is another day.” And that’s enough. Even a tiny spark of hope can carry me through the darkest moments.
Let Go of Pressure
IBD puts pressure on every part of life — physically, emotionally, and socially. I’ve let go of the need to be perfect. If my body tells me to rest, I listen. If I miss something important because of my health, I remind myself: “My health comes first.”
Let Life Be Easier
I no longer compare my life to those who seem to “have it all together.” My peace, joy, and success may look different, and that’s okay: “Let life be gentle, even if it’s not always easy.”
Photo from Unsplash.
Diagnosis is a Light, not a Lamp Shade (Mental Health & IBD Series)
by Aiswarya Asokan (South India)
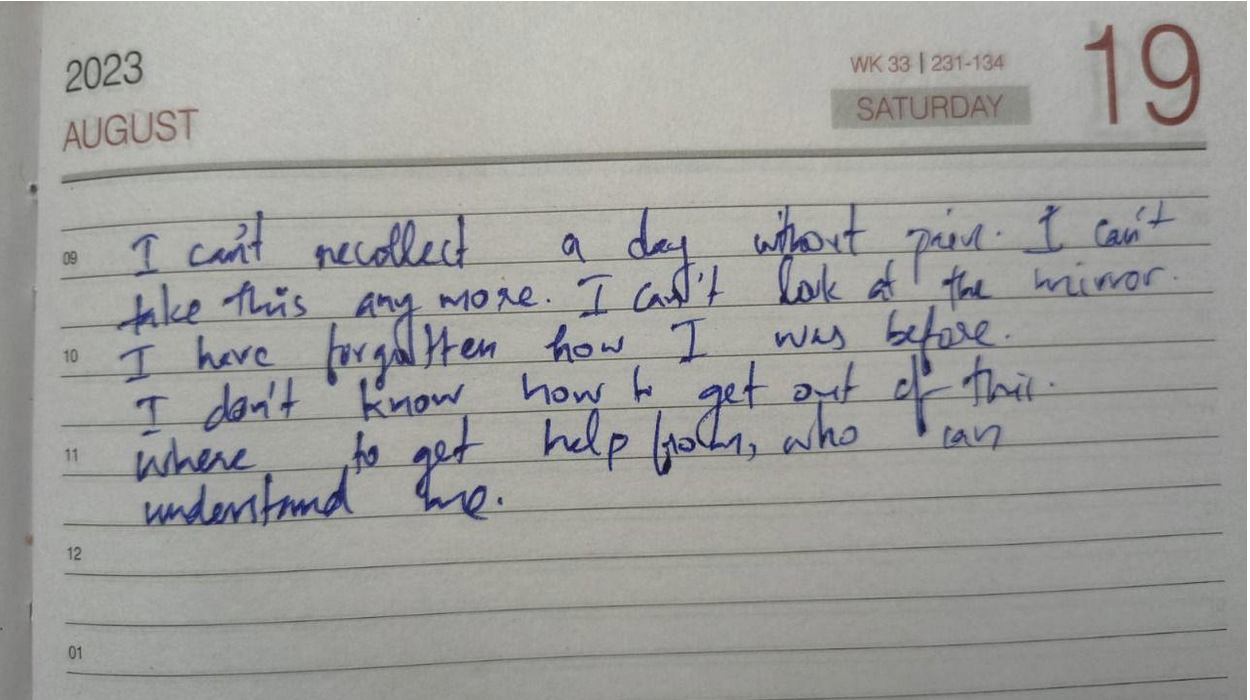
It was on May 2nd 2016, a day before my 19th birthday, for the first time in my life, I heard the word Crohn’s, from my doctor back then. It came as a scientifically valid explanation to all the so-called “sick drama” I was exhibiting through the years. But the excitement of this achievement soon faded away when I came to know that there is no cure for this. Then came the joint family decision, we will keep this diagnosis a secret to ourselves. Anyways, who is going to accept me if they know I have got a disease that makes me run to the toilet and that I have to be on regular medication to stop this from happening. For the next 4 years, I lived like a criminal, fearing for every breath this crime will be caught. In between, I was ill informed about the dietary restrictions I was supposed to follow, and kept eating triggers from time to time, meanwhile wondering why this is happening – but was still focused on keeping the secret safe.
Still, life was a smooth sail with a few days of bad weather here and there, till 2020, when I had my worst nightmare: a serious flare that left me hospitalized for more than 2 months and unable to take my final year university exams. And my secret was out. Not being able to appear for exams was too much for an academically excellent student like me. I was experiencing such intense pain that I couldn’t even turn sides in bed. All this made me question my identity and shattered my fundamental belief system. None of the medicines were working on me. A group of surgeons visited me, and told me that if surgery was attempted, my life might be over on the table. When I realized I might die soon, I decided to live a little. Even though I was not able to eat anything, I ordered a red velvet cake and ate it. The 2020 Tokyo Olympics were going on – it was my all-time wish to watch the Olympics live, but my academic schedule did not allow me to do so. So from the hospital bed, I watched Neeraj Chopra win a gold medal for India, while all my classmates were taking final year exams.
After a while, steroids started working and I started getting better. At the age of 23, I was 33 kilograms, severely malnourished and on a high dose of medication. I was not afraid to die but coming back to normal life was a challenge. I couldn’t face people nor attend phone calls. Even notifications from messages were alarming for me. I zoned out from everyone around me. I felt myself as a complete failure.
One person kept on calling me, despite me ignoring all their calls, until one day I finally picked up. He was my childhood bestie, who stood with me till I was able to manage things on my own. He made a timetable for me, which included slots for physical activity, exam preparations, and fun activities, and made sure I followed them on a daily basis. Then the exam date came up. There were times when I took supplementary exams alone, in a hall that usually accommodates 60 students. Everyday after the exam, he would ask me how it went, and suggest a movie to watch as a reward for the hard work. After a while, exam results came, and I had the highest score than previous years. Life was again on.
Whenever a flare up hits me, the first thing I notice is a keen desire for physical touch, especially a warm hug, though it sounds strange. I also clench my jaw while asleep, to an extent that my whole face and ears start to hurt the next morning, which further makes it hard to have food. Within the next 3 years, time was up again for a rollercoaster. I had a stricture, unbearable pain, my oral intake was nil, and I had to go for a hemicolectomy. The anticipated complications for the surgery were extremely frightening. This time my boyfriend came up and assured me that “no matter what, I will be there for you.” The surgery went smoothly and I was discharged. I was physically fit but started experiencing PTSD-like symptoms. I started feeling I was just a financial burden to my family.
I slept all day and night as I was not ready to face the thoughts in my head. My boyfriend used to call me every day – just for those few moments I was living, but the rest of the time I used to sleep. This time no friends nor family could help me. Then I started searching for IBD support groups, came to know about IBD India, took the free mental health counselling, and joined the peer group. For the first time, I felt less isolated and felt a sense of belonging. And slowly I replaced my coping mechanism of sleeping with painting. Gradually I was healing, and started feeling more freedom like never before.
Life goes on. Ups and downs are part of it. But when one door closes the other opens. When you feel stuck, ask for help and keep asking until you get one strong enough to pull you out — that is the bravest thing you can do for yourself.
Image from Unsplash.
Mental Health and IBD: An Infographic
by Lexi Hanson (Missouri, U.S.A.)
Some connections between Mental Health and IBD (sources included below):
Some evidence supports a reciprocal relationship between mental health and disease activity. Depression is more consistently linked to outcomes than anxiety.
Mental health issues are strongly linked to relapse and recurrence. Stress-related cytokine production likely contributes to inflammation. Anxiety and depression affect treatment adherence, leading to worse outcomes.
Psychiatric comorbidities remain a major driver of poor outcomes and healthcare costs despite advances in treatment.
Some Daily Habits to Help your Mental Health:
☐ Take medications as prescribed
☐ Eat balanced meals that support your gut health (avoid known triggers)
☐ Drink enough water throughout the day
☐ Practice 5–10 minutes of relaxation (deep breathing, meditation, or gentle stretching)
☐ Check in with yourself emotionally (How am I feeling today?)
☐ Engage in light physical activity if able (walk, yoga, stretching)
☐ Prioritize 7–9 hours of quality sleep
☐ Write down one thing you’re grateful for today
Sources:
Mental Illnesses in Inflammatory Bowel Diseases: mens sana in corpore sano. Bartocci et al. 2023. https://pmc.ncbi.nlm.nih.gov/articles/PMC10145199/
Consensus Statement on Managing Anxiety and Depression in Individuals with Inflammatory Bowel Disease. Hinnant et al. 2025. https://academic.oup.com/ibdjournal/article/31/5/1248/7739104
https://www.crohnscolitisfoundation.org/patientsandcaregivers/mental-health
Learning to Complain: A Survival Skill for Chronic Illness
by Akhil Shridhar (India)
For many of us living with IBD, saying “I’m fine” has become a habit, something we were taught to say to avoid worrying others or causing trouble. But managing a chronic condition means we can’t afford silence. Doctors need us to describe what hurts, what’s changed, and what’s not working. At first, that shift feels unnatural. How do you speak up about pain when you’ve spent years trying to hide it? Learning to explain what’s wrong isn’t just about getting better care, it’s about breaking the silence, challenging stigma, and making sure our needs are heard. Speaking up is advocacy, and it starts with learning to complain. Many of us were taught to downplay pain, brushing off discomfort to seem strong.
This kind of silence runs deep, shaped by family, culture, and a society that equates quiet with resilience. But for people living with IBD, staying silent can be dangerous. It leads to delayed care, isolation, and missed warning signs. Although, learning to speak up about symptoms is just a part of it. Especially in developing countries like India, where systems often lack the integration, communication is not just helpful but essential. For most, the responsibility of managing appointments, tracking medical records, logging test results and prescriptions, consulting different specialists, and coordinating insurance doesn’t fall on an organised platform, it falls on the patient.
Living with IBD means your body goes through changes that aren’t always easy to explain. Symptoms come and go, and sometimes they’re hard to put into words, especially if you’ve spent years being told not to make a fuss. When you share what you’re feeling clearly and honestly, you’re helping your doctor understand how to support you better. It’s not complaining, it’s communication. And with a little guidance and the right tools, you can learn to speak the language of your symptoms in a way that leads to real care and understanding.
Doctors rely on clear, consistent information to track how IBD is affecting your body, and that’s where accurate symptom-sharing becomes key. The table below outlines the kinds of details that help build a more accurate picture of your condition.
Living with IBD often means navigating a maze of symptoms, appointments and uncertainty. But the ability to speak clearly and communicate will go a long way in getting the care that we deserve. That’s why this table isn’t just a tool, it can help you bridge the gap between what you feel and what the doctor needs to know. Remember, this guide is meant to serve you, so feel free to adapt it, add to it, and make it your own. Bring it to your appointments, refer to it and use it to shape your care in ways that truly reflect your needs.
This log table is for you to document your symptoms and experiences in a structured manner. Save a copy and take notes or just use it as a reference for your next appointment!
Some Do’s and Don’ts of Travelling Internationally with IBD
by Rifa Tusnia Mona (Dhaka, Bangladesh)
Last month, I took my very first cross-border trip—from Dhaka, Bangladesh, to Delhi, India. It wasn’t just my first international journey; it was also my first time traveling by air. That alone is exciting enough, but there was something more that made it meaningful: it was my first adventure after being diagnosed with Inflammatory Bowel Disease (IBD).
Traveling is always a mix of excitement and unpredictability. Add a chronic illness to the equation, and every small detail becomes a bit more complicated—navigating airports, managing fatigue, handling meals, and dealing with unexpected flares. But from this experience, I learned some lessons I believe could help others who are walking the same path. So, here are a few do’s and don’ts for fellow warriors out there traveling with IBD:
✔️ Do: Plan Your Journey Thoroughly
When you live with IBD, planning isn’t optional—it’s survival. While no amount of planning can prevent every hiccup (hello, Murphy’s Law), it certainly softens the ride. For instance, simple things like knowing where to buy a local SIM card, or how to book an airport cab ahead of time can make a huge difference in having a smooth start!
✔️ Do: Ask for Help When Needed
This is something I struggle with, especially as an introvert. At the airport on my return flight, I was utterly exhausted and going through a flare-up. A kind airport staff member offered to assist me, but I declined—probably out of habit or hesitation. I regretted that later. When you’re in an unfamiliar place, everyone is technically a stranger anyway. So if help is offered, take it. Even small support—like directions to the washroom or help carrying your bag—can be a huge relief when your energy is limited.
❌ Don’t: Follow Others’ Travel Routines Blindly
Everyone’s body is different. What works for your friend might not work for you—and that’s okay. Several people recommended I take the Delhi Metro to get around. It sounded smart, economical, and even a little adventurous. But for someone already fatigued, changing between the Yellow and Pink lines during rush hour turned into a nightmare. That day ended in a flare-up. Lesson learned: listen to your body first. Your energy is precious—don’t waste it trying to keep up with someone else’s idea of efficiency.
These are just a few of the moments from my first international trip with IBD. Traveling with a chronic illness can be isolating. Often, it’s hard to explain your condition or expect some stranger to truly understand it. But the truth is: you understand it. And that’s enough.
Acceptance and self-awareness are your greatest tools. Don’t let IBD define your boundaries. Opportunities are still out there, and you deserve to chase them. If you make room for compassion—for yourself first—you’ll find that you’ve already conquered half the challenges.
Don't forget to enjoy my short video of the journey (linked below!). Again, I thank you for reading this far. See you next month!
A Heart That Heals
by Beamlak Alebel (Addis Ababa, Ethiopia)
Through sleepless nights and heavy days,
You lit my path in countless ways.
With faith and strength, you pulled me through,
Restored my soul, made all things new.
To doctors wise, with healing hands,
Who serve with love in every land—
With knowledge deep and hearts so kind,
You brought me peace and strength of mind.
To the surgeon, calm and true,
Whose steady hands saw me through—
With courage firm and vision bright,
You turned my pain to healing light.
To nurses kind with gentle care,
with whispered prayer—
With watchful eyes and steady grace,
You made the hardest moments safe.
To family strong, who stayed so near,
Who held me close through every tear—
Your endless love, so fierce and true,
Was my sky bright when storms blew through.
To friends who stood through every test,
With laughter shared and hearts at rest—
Your joy and comfort every day
Helped chase the fear and dark away.
To support groups, warm and wise,
Who lift each other’s truths and cries—
You showed me I am not alone,
In every scar, our strength has grown.
Through trials, triumph, joy, and pain,
My gratitude will still remain—
To every soul who walked with me,
I thank you all—eternally.
Image from StockSnap.
Advocating for IBD
by Lexi Hanson (Missouri, U.S.A.)
Why is IBD Important to Advocate for?
IBD (including Crohn’s disease and ulcerative colitis) affects millions worldwide and can severely impair quality of life.
Often diagnosed in teens and young adults, IBD can affect people during the most critical stages of personal and professional development.
Because IBD involves bowel symptoms, people often avoid talking about it, leading to shame and isolation.
Lasting impacts from IBD
High rates of anxiety and depression are associated with IBD due to its unpredictable nature and social limitations.
IBD leads to significant healthcare costs, lost productivity, and financial strain for individuals.
Access to proper diagnosis, treatment, and ongoing care is not equal across regions and populations.
How can we Advocate?
Share personal stories and facts through social media, blogs, podcasts, and public events (especially during awareness months).
Advocate for policies that ensure better healthcare access, insurance coverage, and medical leave protections for those with chronic illnesses.
Form or join local or online support groups to connect patients, caregivers, and allies.
Listening to Your Body with IBD: The Stoplight System
by Michelle Garber (California, U.S.A.)
When you're living with Inflammatory Bowel Disease (IBD), your body becomes its own navigation system. Your body is constantly sending you signals, just like traffic lights do. But unlike the red, yellow, and green lights on the road that we instantly respond to, many of us with IBD have learned to ignore or minimize the "rules" or "drills" that we should follow when our body sends us our own, personal warning signs.
So why is it that we respect a blinking car dashboard, a low battery warning on our electronic devices, and traffic signals/signs more than the signals coming from our own bodies? We wouldn’t ignore our car’s check engine light for weeks (and if we did, we’d expect it to eventually break down). So why do we ignore our body’s warnings? Why don't we listen? As with most things, the answer is complicated.
Here are a few reasons why as people living with IBD, we might forget to listen to these warnings, or try to “push past” them:
Living with IBD means that a few warning lights are always on. That is, we might always have some level of fatigue, bloating, or discomfort. This "always-on" background noise becomes our new normal, and we stop noticing when new signals show up. This is risky because it can lead to ignoring major warning signs or missing slow-building flare-ups.
Our symptoms can become our new normal or "background noise," so we're used to pushing through pain. This means that even when our bodies give us that "red" or "yellow" light signal to slow down or stop due to a symptom/pain that is out of the ordinary, we are still conditioned to push through it. For a lot of us, that is a survival mechanism of having chronic pain (pain that never fully becomes "background noise") in a medical system and society that often tells us to "push through." The world is constructed for those who are able-bodied, and having chronic pain/IBD can force us to sink or swim.
We are often taught to minimize our symptoms, for ourselves and others. Sometimes, doctors dismiss our warning signs, maybe because medical literature doesn't acknowledge all the intricate traffic signals for IBD. Maybe, they're just burned out. Or, maybe doctors—and people in general—can't fully understand the severity of IBD symptoms if they haven't gone through it themselves. Whatever the reason, though, we are conditioned to minimize our symptoms. We are taught that our illness "could be worse." In fact, when explaining IBD to others who don't quite listen closely enough, the false notion that IBD is simply "stomach problems" circulates. So much so that we, ourselves, sometimes say this to others or even believe it ourselves. We don't want to be sick. We wish it was just stomach problems. Being told that our personal traffic lights/signals are simply a result of "anxiety" or "are in our heads" make it easy to eventually believe it ourselves because, why would we want to be sick?
We don’t want to "miss out." Sometimes, we’d rather have a moment of fun—followed by a flare/low-spoons day—than not experience the fun at all. Ignoring the signals can sometimes feel "worth it" since it can give us a small glimpse of what "normal" might be like. We are forever torn between the notions of "respect your body's limits" and "you only live once."
Finding a way to make a choice, despite the consequences, can feel liberating in the short-term. This can look like eating a food that you know isn't "safe" just because you want to make a CHOICE and have autonomy over your own body. As IBD patients, choice is often not in our vocabulary – so pushing through the pain of IBD is often the only way we can feel slightly in control of our own bodies. This is a sense of freedom that we greatly lack as IBD patients.
We don't want to be a “burden.” IBD, in itself, is a burden that we already have to carry. Living with it every day is extremely difficult, and that is an understatement. Even so, we still notice how it affects those around us— our caregivers, partners, family members, friends, co-workers, employers, and even doctors. Carrying the burden alone is never the solution, but it sometimes seems like the right one since it feels wrong to allow someone else to feel even remotely similar to us. It doesn't feel right to allow anyone to be down in the trenches with us—at infusion appointments, at ER visits, at ICU admissions, or at "bathroom sleepovers." It doesn't feel right to allow anyone to feel so wrong, even if they want to. Therefore, we ignore the signs, because if we took action that would mean that we'd need help, whether we like it or not. We'd have to reach out to someone, even if that's just a doctor. Simply alerting your doctor that you've failed another biologic can make you feel like a burden since you might feel as though you're giving them more work. Reaching out to loved ones can be even harder as they will often want to be there for you, and you simply don't want to burden anyone anymore.
We’re afraid of what we’ll find if we stop and really listen. As previously mentioned, we don't want to be sick again. We don't want to discover a new co-morbidity again. We don't want to switch medications again. We don't want to be flaring again. We don't want to go to the hospital again. We don't want to experience medical trauma again. We don't want to put life on pause again. We don't want to miss out again. We don't want to be a burden again. We don't want to lose control again. Listening to your body, and truly paying attention to what it's telling you poses the risk of you having to accept the fact that you might have to go through all of these things again. And at the end of the day, we just want to live—freely. It feels like a constant tug-of-war between surviving and actually living.
The truth is: Your body will always tell you what it needs. It’s just your job to check in—gently and consistently.
Since there is no cure for IBD yet, much of this disease has to do with symptom monitoring and, thus, taking as many preventative measures as possible. I, for one, know that I would like to stay in remission and avoid a flare-up for as long as possible. Even so, I know that's only possible if I listen to my body—genuinely listen. Whether that's taking note of unusual fatigue or nausea, a new sensitivity to food, etc., these are acts of listening to your body and its signals. While we are taught from a young age what traffic lights mean and why it's important to follow them, we aren't taught how to notice and follow the signals that our bodies give us.
A few simple things that you can do to start the practice of ‘checking in’ with yourself and your body:
Create your own ‘traffic light:’ write down some of the signs you notice, when you’re feeling ‘green, yellow, or red!’
Set aside a few minutes each day to ask yourself: What "color" am I today? What makes me that color? What am I feeling, and where am I feeling it? If I’m yellow or red, what needs to change? If I’m green, what can I do to stay there?
Not sure where to start? Here’s an example of my “traffic lights,” and some of the signals I use to check in with myself and my body!
A few things to remember/keep in mind:
Checking in doesn’t mean obsessing. It simply means being mindful enough to care. Just like we do for our phones, our cars, and our jobs—we deserve to offer ourselves the same level of awareness, support, and maintenance.
Living with IBD doesn’t mean you’ll always be stuck in red or yellow. Some days are green—some weeks or months, even. You deserve to honor those days as much as you manage the hard ones.
This stoplight system isn’t about fear. It’s about empowerment. You are not weak for needing rest, medical support, caregiving, or time. You are wise for knowing when to go, when to slow down, and when to stop.
Your body isn’t the enemy—it’s the messenger. Listen to it. Trust it. Respond with love. Your body is doing the best it can to keep you alive. Let’s return the favor.
Image from @tsvetoslav on Unsplash.