NEWS
The Vasovagal Response and IBD
by Kaitlyn Niznik (New York, U.S.A.)
As someone with several medical phobias, I have always been a fainter. Being in a heightened state of fear and stress is a recipe for disaster that usually leads to me being on the ground. It takes skill to faint and take out a row of chairs and your mother at the doctor’s office, but I like to think that I’m improving with time and therapy (see my phobias article for details). However, when I began having digestive issues in college, I started experiencing pre-syncope symptoms frequently during flareups that have lasted to this day. Doctors always told me it was a vasovagal response, so I have been asking nurses and reading up on research in the hopes of finding some answers. Though I have not figured out how to completely stop my symptoms, here is what I have found on the subject and some strategies that may help.
IBD can come with a multitude of strange and hard-to-explain symptoms with some occurring outside of the gastrointestinal system. These extraintestinal manifestations can include feeling faint during a period of intense stomach pain or dizzy during a bowel movement. The vagus nerve and parasympathetic nervous system connect the gut, heart and brain, causing a plethora of vasovagal symptoms when thrown out of balance.
For some background information, syncope is a medical term for fainting while presyncope describes the symptoms one experiences when they almost pass out - including dizziness, nausea, blurry vision, weakness, and chills or sweating. Both syncope and presyncope can be signs of different conditions, but are also strongly attributed to vasovagal syncope. Vasovagal syncope is experienced by around a third of the world and is a common symptom of dehydration, giving blood, standing up too quickly, etc. (Johns Hopkins Medicine, Syncope). According to Verywell Health, a vasovagal response can have physical triggers, such as straining during bowel movements, stomach illness, and pain, or emotional triggers like anxiety, trauma, fear, or stress (Bolen, 2025).
**It’s important that if you experience syncope or pre-syncope symptoms that you get checked out by a doctor. Tests like an Electrocardiogram, echocardiogram, tilt table test, CT, MRI, carotid artery ultrasound, and more can be used to rule out serious heart problems, seizures, or conditions like POTS.** (Johns Hopkins Medicine, Syncope)
According to the paper “The autonomic nervous system and inflammatory bowel disease,” there is strong evidence supporting the connection and interaction between the central nervous system and the intestines. When the body is triggered by high stress or chronic stress, it can have a direct effect on our gut’s inflammatory response. Vagal neurons permeate the gut wall and play an important role in the transfer of information from the gut to the central nervous system and vice versa. This connection is commonly known as the gut-brain axis. These sensitive nerve connections can even affect our perception of IBD-associated pain and disease symptoms can be exacerbated (Taylor & Keely, 2007). Our bodies need to find a balance between the nervous system and gut. Too much or too little activation can trigger responses in multiple areas of the body and have unforeseen consequences.
Some common vasovagal response symptoms are:
Tunnel vision/blurred vision
Dizziness
Weakness
Ringing in the ears
Cold or clammy skin
Feeling hot
Nausea
A temporary drop in blood pressure (Bolen, 2025)
Syncope or fainting
Short term amnesia or confusion upon waking
Brief convulsions of the limbs (Wang et al., 2024)
What can you do during a vasovagal episode?
Sit or lie down (injury prevention)
Put your head between your knees
Avoid straining
Stay hydrated
On top of those tips, this is how I deal with repeat vasovagal episodes:
Firstly, I document everything so I can give my doctor a better idea of what I experience and how frequently. A smart watch is also useful so I can keep track of my bpm. There are a few trusted friends and family members that know of my condition and the warning signs. Of course, it’s helpful if you know your own body’s warning signs - it can help you predict it before it happens.
I also keep my phone on me at all times in case I need to call for help. After a vasovagal episode, I give myself time to feel better - usually curling up on the couch with a blanket and some water. I always use electrolytes to help my body recover faster and I keep heating pads with me since I can feel cold or shaky afterwards.
Possible forms of treatment that I’ve learned about:
Medication
Physical counterpressure maneuvers (Wang et al., 2024)
Pelvic Floor Therapy
Vagus Nerve Stimulation
Psychotherapy
I found it interesting that one medical professional recommended looking into psychotherapy to address the psychosocial component of vasovagal responses. Having fainting episodes or those revolving around intense pain can be terrifying and that fear can stick around long after the incident ends. Traumatic memories of pain around bowel movements can cause increased anxiety and escalate vasovagal responses. Confronting your anxiety and the reasons behind your fight/flight/freeze can help mitigate symptoms. By always having a plan and knowing the signs, I can better prepare myself to deal with vasovagal responses.
Works Cited:
Bolen, B. (2025, October 30). Common causes and triggers of the vagal response. Verywell Health. https://www.verywellhealth.com/vasovagal-reflex-1945072
Syncope (fainting) | Johns Hopkins Medicine. Johns Hopkins Medicine. (n.d.). https://www.hopkinsmedicine.org/health/conditions-and-diseases/syncope-fainting
Taylor, C. T., & Keely, S. J. (2007). The autonomic nervous system and inflammatory bowel disease. Autonomic Neuroscience, 133(1), 104–114.https://doi.org/10.1016/j.autneu.2006.11.005
Vagus nerve: What it is, function, Location & Conditions. Cleveland Clinic. (2022, November 1). https://my.clevelandclinic.org/health/body/22279-vagus-nerve
Wang, J., Li, H., Huang, X., Hu, H., Lian, B., Zhang, D., Wu, J., & Cao, L. (2024, April 10). Adult vasovagal syncope with abdominal pain diagnosed by head-up tilt combined with transcranial Doppler: A preliminary study. BMC neurology. https://pmc.ncbi.nlm.nih.gov/articles/PMC11005138/#:~:text=The%20value%20of%20HUT%20combined,the%20adoption%20of%20safety%20measures
Featured image from Henrik Dønnestad on Unsplash.
To See What Cannot Be Seen: Living with Chronic Pain and IBD
by Michelle Garber (California, U.S.A.)
When most people hear the word "remission," they imagine relief, a clean slate, and the end of suffering. For those of us living with Inflammatory Bowel Disease (IBD), remission is supposed to mean that we can finally be free of the pain that controlled our lives and simply breathe again. Unfortunately, for so many IBD patients, remission doesn't mean that the pain disappears. Rather, our pain changes form. Our pain becomes quieter, more private, and more invisible. It becomes the kind of pain that can exist in silence. The kind of pain that may not scream for help, yet it still whimpers day and night. The kind of pain that is easy to be overlooked while the rest of the world assumes you're fine.
Chronic pain is one of the most misunderstood aspects of IBD. It lingers long after flares fade, threading through your days in ways that are impossible to explain. It's invisible, yet constant. It's being in pain every single day, but learning to function anyway because you have no other choice. Chronic pain has become a part of my life—like a ringing in my ears that I've had to learn to ignore. I've learned to appear "fine" because visible pain tends to make others uncomfortable, and because I've discovered that admitting the truth often leads to dismissal. I have become so adept at masking my pain that I've become fluent in pretending. Pretending that I'm not silently calculating how much longer I can keep standing before the pain in my abdomen forces me to sit down. Pretending that the subtle grimace that escaped when I moved the wrong way was just a product of my "resting b*tch face." And pretending that "pain" is no longer in my vocabulary.
The pain of IBD patients also commonly goes unrecognized by medical professionals because the traditional 1-10 pain scale was not built for those living with chronic pain. For example, if I tell a doctor that my pain is at a "6/10," they may interpret that as "moderate discomfort." For those without IBD or chronic pain, though, my "6" might be their "10." Our baseline is simply so different from those without chronic illness/chronic pain, therefore making the standard 1-10 pain scale almost meaningless for us. This can have dangerous consequences as pain is typically the body's signal that something is wrong. When we are constantly experiencing pain, it can be difficult to determine whether it's "significant enough" to seek help or whether it's just our "new baseline." The fact of the matter is that any pain should be and is "significant enough," but we've been conditioned to not view it as such. We've been conditioned to accept a new and distorted "baseline level of pain" due to our illness, when those without chronic pain are not encouraged to do the same. Therefore, it can be hard for both us and medical professionals to know when something is "wrong," creating the potential for treatment delays, disease progression, prolonged suffering, and—depending on the illness—even fatal consequences.
Living with chronic pain often means learning to downplay your pain. No matter how much pain I'm in, I never rate my pain as a "10." I rarely even rate it as an "8" or a "9" because I know what happens when I do. I've seen "the look." It's that flicker of suspicion that crosses a medical provider's face when you say you're in severe pain, but you don't exactly "look" like it. I have felt the shift in tone when my honesty is mistaken for medication-seeking or when my tears are assumed to be those of ‘crocodiles.’ Because as it has been made quite clear by many medical professionals, if you don't have overwhelmingly visible evidence of your pain, then it must be exaggerated. Or, you must have a mental illness since "it's just anxiety," and "it's all in your head." So, like many others, I minimize my pain. I say that it's a "4" or "5." I'll tell doctors that my pain is manageable, even when it's often very much not.
The stigma of simply wanting relief is one of the cruelest aspects of IBD and chronic pain. The truth is, it's terrifying to need help in a system that might not believe you. IBD also presents unique challenges when it comes to pain management. Nonsteroidal anti-inflammatory drugs (NSAIDs) are usually off-limits because they can actually trigger flares. Opioids, while sometimes the only medications strong enough to even touch the pain, are approached with understandable caution due to their risks (i.e. the potential for constipation, dependency, and/or substance use disorder). As a result, we're often left to "cope." We're told to meditate, breathe, use heating pads so often that we burn ourselves, and/or use methods of distraction while our insides feel as though they're literally being twisted inside-out. If we're lucky, we might just get a pamphlet or a link to a video explaining these coping mechanisms. We're essentially almost abandoned by most medical providers as they expect us to endure significant pain without the use of effective pain relief options.
Don't get me wrong, these coping skills can help, but they certainly don't erase our pain. They just make it more bearable. Over time, the constant strain of pushing through the pain can wear down even the strongest person—the person who has "been through it all" and has a "high pain tolerance." Chronic pain doesn't just live in the body. Chronic pain infiltrates the mind and can chip away at one's patience, hope, and even will to keep fighting.
Yet, I understand why providers are cautious when it comes to pain management because I've seen the other side of it too. I currently work at a substance use disorder treatment center as a soon-to-be therapist. I've noticed that many clients' struggles with substances began in the same place: pain. Some struggled with physical pain, some with emotional pain, and many with both. Some clients even suffered from chronic illness(es)/injuries, were told that there was nothing that could be done for their pain, and were never provided with any sort of pain relief by their doctors. Others were prescribed opioids for a while and were then abruptly cut off from them by their medical providers. Much of their substance use history echoes the desperation that many IBD patients have also experienced—the desperation to simply function. The desperation to hold down a job and just get through the day. The desperation to be able to sleep through constant throbbing and aching. The desperation to escape one's pain for "just five minutes." The desperation to just be.
These stories serve as a reminder that pain affects so much more than what meets the eye. That's why it hurts so deeply when our pain is minimized by doctors, friends, family members, partners, and even by ourselves. We tell ourselves that our pain isn't as bad as it feels, while we're quietly counting the minutes until we can lie down. We tell others that we're "fine" because we don't want to be seen as "fragile" or "dramatic." We tell doctors lower numbers on the pain scale so that they'll take us seriously. Many of us would rather suffer quietly than risk being labeled. We learn to mask pain so well that even those closest to us never usually realize the strength it takes for us to just get out of bed.
Masking pain comes at a cost, though. Each time we minimize our pain, we invalidate our own experience. We erase a little bit of our own truth, piece by piece—a small but painful act of self-betrayal that we've been conditioned to commit in order to be believed. Masking pain also isolates us. It makes our struggle invisible, and in doing so, it allows others—including medical professionals—to not be able to see the undeniable pattern of IBD patients with chronic pain.
Pain is not just a symptom. It's a lived experience that profoundly shapes our relationships, our work, our self-worth, our future, and our sense of identity. For example, we might pursue occupations that don't require physical labor, and we might choose living environments that are close to our caregivers/doctors, have bathtubs over showers, and lack staircases. For those of us living with a chronic illness, pain becomes part of who we are—not because we want it to, but because it demands to be acknowledged.
Living with chronic pain and IBD means existing somewhere in a space between endurance and exhaustion. Between being believed and being dismissed. It means learning to hold compassion for yourself, even when the world doesn't. It means carrying an invisible burden that requires extraordinary strength to bear, even though it feels as though you have no strength left to do so. It means showing up—for others, for yourself, and for life itself—often without anyone realizing just how much effort it all takes.
That quiet persistence is something that I have come to admire deeply, both in myself and in others who live this reality. Because even when our pain is invisible, our resilience is not. It serves as a powerful testament to every person who keeps going despite their own body making the simplest things feel impossible. And even though our pain may be a part of who we are, our resiliency proves that it is certainly not all of who we are. We are so much more than our pain and our illness.
Still, our pain deserves to be acknowledged. Our stories deserve to be believed. Our healthcare system must learn to see what cannot be seen—not to just treat the illness, but to honor the full human experience of actually living with it.
Therefore, we need a better way to talk about chronic pain, especially in regards to IBD. We need providers to understand that our "normal" is not their "normal." That just because we appear to be "fine" does not mean that we are not suffering. That pain in remission is real. And that asking for pain relief isn't manipulation—it's survival.
Living with chronic pain and IBD means learning to navigate a world that often doubts what it can't see. But we exist, and our pain is valid. It's time for the system and the world to finally see us because if you look hard enough, you'll see that our pain is actually not as invisible as it seems—it just continues to go unseen.
Image by @gnikomedi on Unsplash.
Fatigue and IBD
by Aiswarya Asokan (South India)
Check out Aiswarya’s presentation slides on fatigue & IBD! She shares about the prevalence of fatigue, types of fatigue, risk factors, the impact fatigue can have on IBD patients, and some suggestions for managing fatigue.
Listening to Your Body with IBD: The Stoplight System
by Michelle Garber (California, U.S.A.)
When you're living with Inflammatory Bowel Disease (IBD), your body becomes its own navigation system. Your body is constantly sending you signals, just like traffic lights do. But unlike the red, yellow, and green lights on the road that we instantly respond to, many of us with IBD have learned to ignore or minimize the "rules" or "drills" that we should follow when our body sends us our own, personal warning signs.
So why is it that we respect a blinking car dashboard, a low battery warning on our electronic devices, and traffic signals/signs more than the signals coming from our own bodies? We wouldn’t ignore our car’s check engine light for weeks (and if we did, we’d expect it to eventually break down). So why do we ignore our body’s warnings? Why don't we listen? As with most things, the answer is complicated.
Here are a few reasons why as people living with IBD, we might forget to listen to these warnings, or try to “push past” them:
Living with IBD means that a few warning lights are always on. That is, we might always have some level of fatigue, bloating, or discomfort. This "always-on" background noise becomes our new normal, and we stop noticing when new signals show up. This is risky because it can lead to ignoring major warning signs or missing slow-building flare-ups.
Our symptoms can become our new normal or "background noise," so we're used to pushing through pain. This means that even when our bodies give us that "red" or "yellow" light signal to slow down or stop due to a symptom/pain that is out of the ordinary, we are still conditioned to push through it. For a lot of us, that is a survival mechanism of having chronic pain (pain that never fully becomes "background noise") in a medical system and society that often tells us to "push through." The world is constructed for those who are able-bodied, and having chronic pain/IBD can force us to sink or swim.
We are often taught to minimize our symptoms, for ourselves and others. Sometimes, doctors dismiss our warning signs, maybe because medical literature doesn't acknowledge all the intricate traffic signals for IBD. Maybe, they're just burned out. Or, maybe doctors—and people in general—can't fully understand the severity of IBD symptoms if they haven't gone through it themselves. Whatever the reason, though, we are conditioned to minimize our symptoms. We are taught that our illness "could be worse." In fact, when explaining IBD to others who don't quite listen closely enough, the false notion that IBD is simply "stomach problems" circulates. So much so that we, ourselves, sometimes say this to others or even believe it ourselves. We don't want to be sick. We wish it was just stomach problems. Being told that our personal traffic lights/signals are simply a result of "anxiety" or "are in our heads" make it easy to eventually believe it ourselves because, why would we want to be sick?
We don’t want to "miss out." Sometimes, we’d rather have a moment of fun—followed by a flare/low-spoons day—than not experience the fun at all. Ignoring the signals can sometimes feel "worth it" since it can give us a small glimpse of what "normal" might be like. We are forever torn between the notions of "respect your body's limits" and "you only live once."
Finding a way to make a choice, despite the consequences, can feel liberating in the short-term. This can look like eating a food that you know isn't "safe" just because you want to make a CHOICE and have autonomy over your own body. As IBD patients, choice is often not in our vocabulary – so pushing through the pain of IBD is often the only way we can feel slightly in control of our own bodies. This is a sense of freedom that we greatly lack as IBD patients.
We don't want to be a “burden.” IBD, in itself, is a burden that we already have to carry. Living with it every day is extremely difficult, and that is an understatement. Even so, we still notice how it affects those around us— our caregivers, partners, family members, friends, co-workers, employers, and even doctors. Carrying the burden alone is never the solution, but it sometimes seems like the right one since it feels wrong to allow someone else to feel even remotely similar to us. It doesn't feel right to allow anyone to be down in the trenches with us—at infusion appointments, at ER visits, at ICU admissions, or at "bathroom sleepovers." It doesn't feel right to allow anyone to feel so wrong, even if they want to. Therefore, we ignore the signs, because if we took action that would mean that we'd need help, whether we like it or not. We'd have to reach out to someone, even if that's just a doctor. Simply alerting your doctor that you've failed another biologic can make you feel like a burden since you might feel as though you're giving them more work. Reaching out to loved ones can be even harder as they will often want to be there for you, and you simply don't want to burden anyone anymore.
We’re afraid of what we’ll find if we stop and really listen. As previously mentioned, we don't want to be sick again. We don't want to discover a new co-morbidity again. We don't want to switch medications again. We don't want to be flaring again. We don't want to go to the hospital again. We don't want to experience medical trauma again. We don't want to put life on pause again. We don't want to miss out again. We don't want to be a burden again. We don't want to lose control again. Listening to your body, and truly paying attention to what it's telling you poses the risk of you having to accept the fact that you might have to go through all of these things again. And at the end of the day, we just want to live—freely. It feels like a constant tug-of-war between surviving and actually living.
The truth is: Your body will always tell you what it needs. It’s just your job to check in—gently and consistently.
Since there is no cure for IBD yet, much of this disease has to do with symptom monitoring and, thus, taking as many preventative measures as possible. I, for one, know that I would like to stay in remission and avoid a flare-up for as long as possible. Even so, I know that's only possible if I listen to my body—genuinely listen. Whether that's taking note of unusual fatigue or nausea, a new sensitivity to food, etc., these are acts of listening to your body and its signals. While we are taught from a young age what traffic lights mean and why it's important to follow them, we aren't taught how to notice and follow the signals that our bodies give us.
A few simple things that you can do to start the practice of ‘checking in’ with yourself and your body:
Create your own ‘traffic light:’ write down some of the signs you notice, when you’re feeling ‘green, yellow, or red!’
Set aside a few minutes each day to ask yourself: What "color" am I today? What makes me that color? What am I feeling, and where am I feeling it? If I’m yellow or red, what needs to change? If I’m green, what can I do to stay there?
Not sure where to start? Here’s an example of my “traffic lights,” and some of the signals I use to check in with myself and my body!
A few things to remember/keep in mind:
Checking in doesn’t mean obsessing. It simply means being mindful enough to care. Just like we do for our phones, our cars, and our jobs—we deserve to offer ourselves the same level of awareness, support, and maintenance.
Living with IBD doesn’t mean you’ll always be stuck in red or yellow. Some days are green—some weeks or months, even. You deserve to honor those days as much as you manage the hard ones.
This stoplight system isn’t about fear. It’s about empowerment. You are not weak for needing rest, medical support, caregiving, or time. You are wise for knowing when to go, when to slow down, and when to stop.
Your body isn’t the enemy—it’s the messenger. Listen to it. Trust it. Respond with love. Your body is doing the best it can to keep you alive. Let’s return the favor.
Image from @tsvetoslav on Unsplash.
Flare-up: A Downward Spiral
by Akhil Shridhar (Bengaluru, India)
It all begins with a flare-up. For most of us, the diagnosis comes only after enduring symptoms for days or months, dismissed as a stomach bug. But when the discomfort escalates into a significant disruption, we hear the term “flare-up” for the first time. The symptoms build like a chain reaction, growing worse until urgent medications—usually steroids or antibiotics—are prescribed for relief.
Difficulty with Food
Almost every food item can trigger nausea or an urgent trip to the restroom, making nutrition a frustrating challenge. While some believe short-term food restrictions might ease inflammation, prolonged deprivation causes more harm. In countries like India, navigating diverse dietary recommendations complicates matters. As newly diagnosed individuals we often seek advice in support groups, hoping for recipes or meal plans that won’t worsen symptoms. But in most households, skipping meals isn’t acceptable. Our parents insist on “good food,” unaware that their concern often fuels the next domino.
The Washroom Runs
Initially, the frequent restroom trips are an inconvenience—but soon, they dictate life. The unpredictability makes outings stressful, and hesitation around food becomes constant. Exhaustion follows, leaving us dehydrated, fatigued, and mentally drained. The cycle feeds itself: eating triggers symptoms, symptoms disrupt daily activities, and fatigue makes even basic tasks overwhelming.
The Mental Toll
Beyond the physical struggle, IBD takes an emotional toll. The anxiety of unpredictability, the frustration of adapting to a condition that doesn’t follow rules, and the isolation of feeling misunderstood weigh heavily. Conversations become filtered—friends may not fully grasp the challenges, and outings are haunted by the fear of urgently needing a restroom.
Sleep Struggles
IBD doesn’t stop at meals—it disrupts rest too. Pain, restroom trips, and anxiety make sleep elusive, worsening inflammation and fatigue. Poor rest perpetuates the cycle, making daily recovery harder. Many of us try strict bedtime routines, meal adjustments, or sleep aids to reclaim rest. While perfect sleep remains rare, small efforts help ensure the limited hours of sleep offer some recovery.
Finding Balance
What I have realised after a few misadventures is that the best way to get out of this spiral is to consult your medical team and get the required medications right away. The damage that prolonged inflammation has is quite severe and takes months if not years to reverse, sometimes is unfortunately irreversible, therefore it is not worth the risk of ignoring it.
IBD is unpredictable and exhausting, but it doesn’t define life. Over time, we find dietary adjustments, support systems, and coping mechanisms to regain control. Gradually, these adjustments help restore control—accepting the hard days, seeking support, and celebrating small victories. While flare-ups will always come and go, so does recovery. Life continues, not perfectly, but uniquely. And within that cycle, resilience proves stronger than the condition itself.
Image from meister_photos on Unsplash.
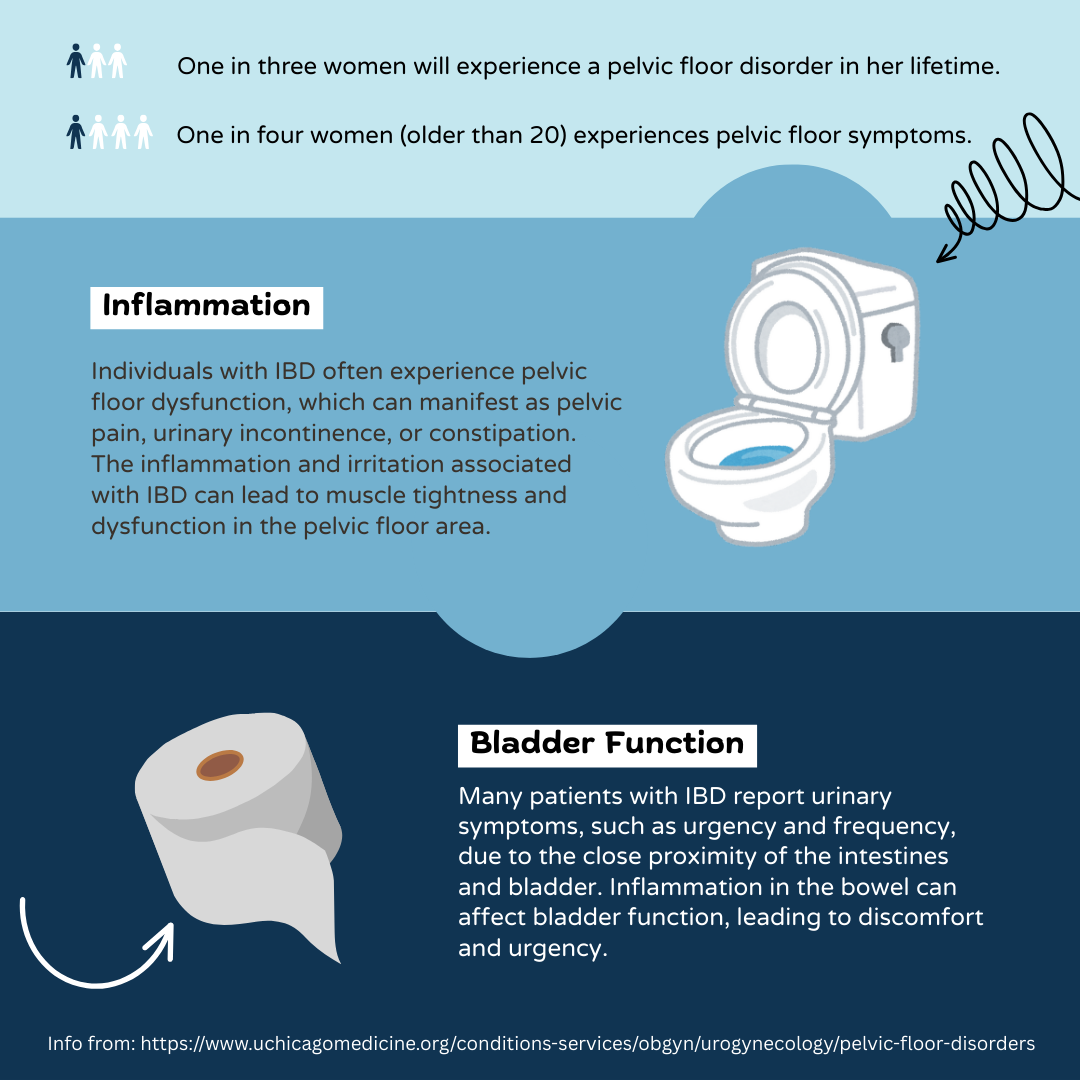
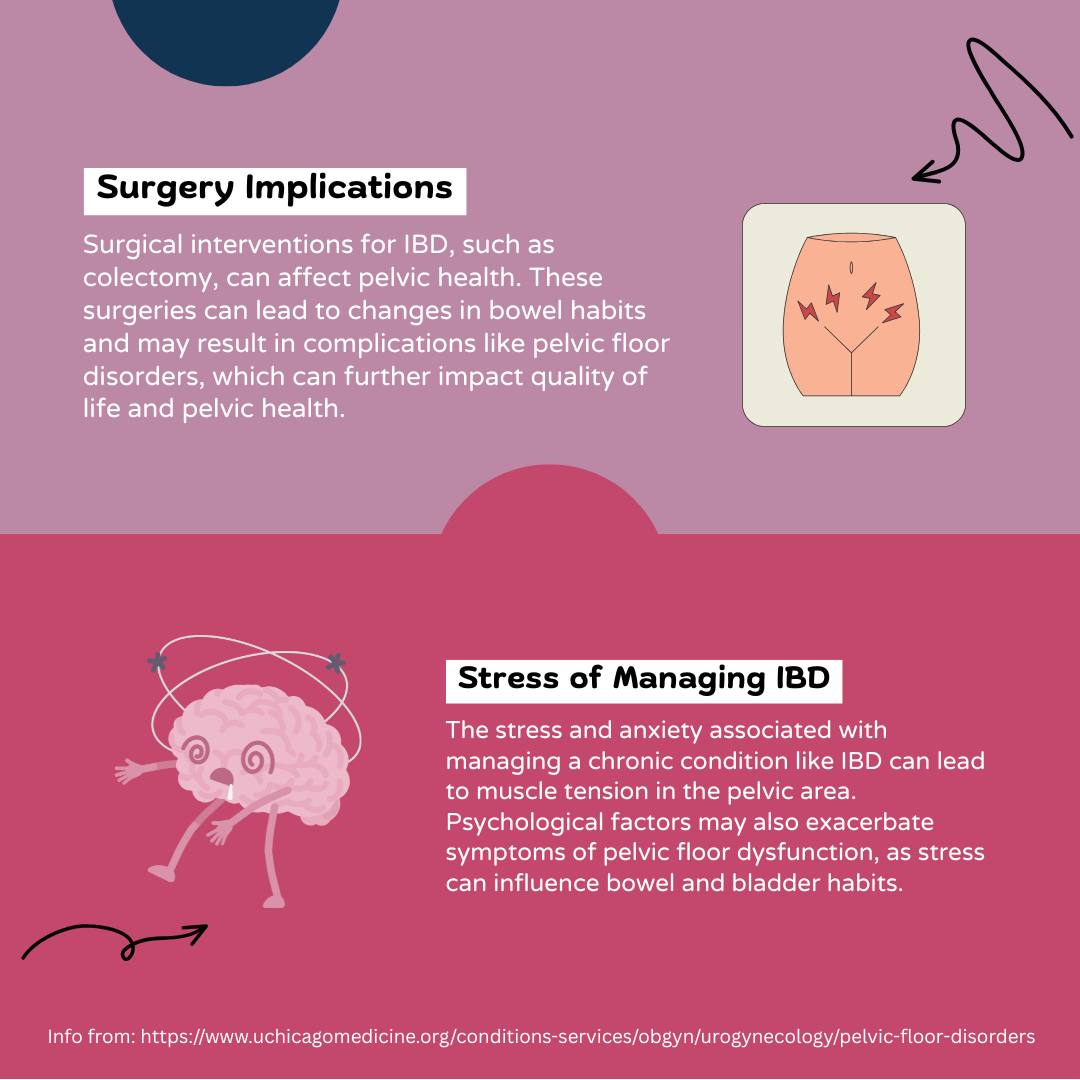
Pelvic Health and IBD: An Infographic
by Lexi Hanson (Missouri, U.S.A.)
Info from: https://www.uchicagomedicine.org/conditions-services/obgyn/urogynecology/pelvic-floor-disorders.
Navigating the Fatigue Roller Coaster: My Personal Journey with Crohn's Disease
By Yeabsira Taye from Addis Ababa, Ethiopia
Living with Crohn's disease, a type of inflammatory bowel disease (IBD) which is chronic, comes with its unique set of challenges. Among the many symptoms that accompany this condition, fatigue has been a constant companion on my journey. Fatigue in Crohn's disease is unlike any tiredness I had experienced before. It goes beyond feeling simply tired or sleepy. It is a bone-deep weariness that affects every aspect of my life. The unpredictability of fatigue is one of the most frustrating aspects. Some days, I wake up feeling relatively energetic and ready to take on the world, only to be struck by an overwhelming wave of exhaustion a few hours later. Other days, the fatigue is ever-present and weighs me down from the moment I open my eyes.
The constant battle with fatigue takes a toll on my emotional well-being as well. It can lead to feelings of guilt, frustration, and even isolation. I often find myself feeling guilty for not being able to fulfill commitments or meet the expectations I have for myself. The inability to keep up with social activities or spend quality time with loved ones can lead to a sense of isolation and a fear of missing out.
As a medical student with Crohn's disease, battling chronic fatigue in the midst of hectic schedules is a formidable challenge. The unpredictable nature of the fatigue makes it difficult to plan and commit to my studies. There are days when I wake up feeling relatively energetic, only to have my energy levels plummet suddenly, leaving me unable to fulfill my obligations. This inconsistency can be disheartening and can lead to feelings of guilt and self-doubt.
The experience of thriving for two years with Crohn's disease taught me that living with fatigue of Crohn's disease is an ongoing journey that requires patience, resilience, and self-compassion. By accepting the realities of fatigue and implementing strategies such as energy management, rest, nutrition, exercise, stress management, and building a support network, I have transformed my experience from one of mere survival to one in which I am thriving, despite the challenges.
Remember, you are not alone in this journey, and with perseverance and a tailored approach, it is possible to reclaim control over your life and find moments of joy and fulfillment amidst the shadows of fatigue.
Featured photo by lalesh aldarwish from Pexels.
Haemoglobin Heist: Anaemia as a Complication of IBD
By Zahraa Chorghay, Montreal
I transformed into a vampire in a field of daffodils
their lips drooped aghast as I soaked in the blood
of another human
my body was consumed with insatiable hunger
a voracious appetite for haemoglobin and oxygen
for life
the first miracle of life is birth, the second is living
with all its defiance of the inevitable
of death
Do you know where all my blood went when I showed up to my hospital’s emergency department (ER), my head pounding and tests showing anaemia so acute as if I’d just bled out? They patched me up — a needle inserted into my left antecubital area (inner elbow) to deliver a unit of blood, stat, and some iron too — but remained bewildered as to the cause. On a stretcher parked next to the nurse station, I stared up at the ceiling tile painted with five daffodils, feeling like absolute shit yet relieved at the thought that maybe when all this was done, I would finally be rid of the headaches that had haunted me continuously for over a month.
It’s always the same, believe it or not; “It’s always the Crohn’s, believe it or not,” I told the tired attending doctor. Then, I headed home after an eventful day spent in the ER.
Anaemia is “the most common metabolic complication” of inflammatory bowel disease (IBD), defined as a haemoglobin level of less than 13 g/dL in men or 12 g/dL in non-pregnant women (Mahadea et al., 2021). Given that haemoglobin is the oxygen carrier within your red blood cells, individuals will have reduced blood oxygen levels in anaemia, underlying the following symptoms:
fatigue
weakness
low blood pressure
shortness of breath, even at rest or with mild activities
rapid heart rate
numbness or tingling in your extremities
irritability
headaches
pale skin
slight fever
What makes anaemia particularly complicated in people with IBD is the susceptibility to blood loss, dehydration, malabsorption, and malnutrition from chronic intestinal bleeding, inflammation, and ulcerations. IBD symptoms such as chronic fatigue, along with side effects of medications or surgical procedures, can further mask symptoms that medical practitioners otherwise rely upon to diagnose anaemia. To demonstrate just how complicated it can be, over months, I gradually had all of the symptoms listed above, which I complained about to my family doctor (GP) a couple of times, yet my anaemia remained undiagnosed.
The decrease in haemoglobin levels seen in anaemia can arise from iron deficiency since iron is necessary for haemoglobin formation. To increase iron intake, you can consume iron-rich foods, such as red meat, eggs, legumes, and leafy green vegetables like spinach and kale (Mayo Clinic, accessed 2024). (Palak ghosht, anyone?) Iron supplements, either oral tablets or IV infusions, may also be administered to individuals with anaemia, but those can have adverse effects so dietary changes are preferred.
Unfortunately, even people who consume sufficient iron can show low haemoglobin levels due to lack of absorption through a diseased or surgically excised gut in IBD, other deficiencies (e.g., of folic acid or vitamin B12), early destruction of red blood cells in hemolytic anaemia, inherited disorders like sickle cell disease or thalassemia, menorrhagia (excessive menstrual bleeding), or adverse effects of certain medications (Penn Medicine, accessed 2024). Depending on the aetiology of the anaemia, different treatment options can be pursued.
In case you’re wondering how anaemic you need to be for your suggested treatment to be a blood transfusion — a last resort option due to its well-documented adverse effects, including potentially immune rejection — I showed up to the ER with a haemoglobin level of just 4.2 g/dL. I can’t get over how I was still able to get through that month of continuous headaches and shortness of breath everytime I stepped out of the house, appearing relatively functional to everyone else, despite calamity looming within me, literally within my veins. The human body is marvelously resilient, subhanallah! Nevertheless, I hope that having read this piece, you will be more easily able to recognize these signs and symptoms of anaemia as well as to advocate for yourself in medical settings, preventing you from having to find out firsthand just how resilient your body can be.
Featured cover photo by Irina Iriser from Pexels.
A Not So Invisible Illness: Inflammatory Bowel Disease
By Maria Mutka from NC, USA
Content Warning: Body dysmorphia, abnormal eating and exercise patters.
As a high school teenager, I thought I was doing well at hiding my illness from my friends and peers. When there were snacks or meals served at school that I knew would send me straight to the bathroom, I deftly avoided them and made excuses that I had already eaten or just wasn’t hungry. If I was experiencing extreme abdominal pain, bloating, and gas during the school day, I tried to ignore it while positioning myself as close to the door as possible, just in case.
For most of high school, I experienced a constant flare that fluctuated between mild and moderate symptoms. This made hiding the tangible symptoms of my ulcerative colitis somewhat possible in my mind, although my friends and peers undoubtedly knew I was experiencing gastrointestinal health issues. I had briefly mentioned to them before that I had inflammatory bowel disease (IBD), but avoided elaborating on what that meant out of embarrassment and fear that it would make them uncomfortable.
I soon realized that there was one facet of my illness I could not hide from my classmates: while being a sophomore in high school, I was 5’2” and barely 80 lbs., with the face and the body of an 11- or 12-year-old. This visible manifestation of my illness through delayed puberty caused me to experience a lot of insecurity, which in turn led to becoming obsessed with food intake and exercise. I was constantly trying to find the perfect balance between food and exercise that could overcome the deleterious impacts of my ulcerative colitis on the absorption of nutrients critical to my growth.
Perhaps the reality of my underdeveloped body so heavily impacted me because of my journey with ulcerative colitis since the age of 6. I had gotten used to the other physical manifestations of the disease: frequent bowel movements, diarrhea, blood, pain, and extreme fatigue, but this limbo stage of early pubescence was new to me. It was extremely damaging to my adolescent attempts at processing and accepting my body for what it was, and at developing anything resembling a positive body image.
At the time, it felt as though with my IBD symptoms continuing, the very least my body could offer me was a sense of somatic belonging and self-worth that I felt could only come from looking like my peers. I was determined that looking my age would help me finally feel like I had access to the same sort of normal teenage experiences they did. Maybe once I looked like everyone else, I would feel more confident in making new friends, being involved in athletics, straying outside the comfort of a singular, perfectionistic focus on academic success by making mistakes, and dating.
For so long, I let my physical appearance dominate my social interactions and extracurricular activities because I felt like an imposter in my own body, completely estranged from what I thought it meant to be a teenager like my peers. In my mind, I was only able to watch from the sidelines as high school, along with the seminal memories and lessons that accompany adolescence, unfolded for everyone else.
Part of the issue was that I was not simply imagining my peers’ perceptions of my physical appearance. Under the guise of concern, while trying on costumes for high school theater productions, several of my peers would tell me that I needed to eat more, bluntly stating that I looked like a twig. In those moments, I could not have felt more infantilized or more childlike not only in appearance but in how my peers treated me.
It was not only my peers who infantilized me. Eventually, I was referred to an endocrinologist for my stalled growth. While I had looked forward to identifying possible solutions to my inability to gain weight and progress further in puberty, all I received from my doctor were vague assurances I would eventually grow and that my endocrine system was in working order. These small efforts at placating the concerns that were wreaking havoc on my mental and social quality of life while well-meaning, were harmful. They reinforced my ever-growing anxiety that my situation would never change and that my mental health and social quality of life did not matter.
My experience with US health care systems’ large deficits in addressing chronically ill youths’ psychosocial needs and quality of life is, unfortunately, not at all unique. Whether these needs are avoided intentionally through health systems causing direct medical trauma, or through omission in failing to address social determinants of health (e.g., housing needs or food needs), the harm done is impactful and lasting. If providers had screened for or discussed my mental health and psychosocial needs related to my IBD at any point, I would have jumped at the chance to talk about it. However, my physical symptoms were the only topic of discussion and implied to be the only issue that could even concern me.
I know now that delayed puberty is not an uncommon comorbidity of pediatric inflammatory bowel disease, as many studies on the subject have shown. Despite my at-the-time unassuageable fears, I did eventually grow and complete puberty, although I do still receive comments that I look young for my age.
Looking back at my adolescence, when I felt like I was perpetually stuck in a Groundhog Day scenario due to my delayed puberty, in hindsight, I can appreciate all my body did for me. I was able to make it through a multi-year-long flare, and all things considered, my body managed it pretty well. Looking back, I try to have compassion for my perfectionistic teenage self who was determined to look like her peers to an unhealthy extreme. What she needed was a pat on the head or vague assurances everything would turn out okay. She did not even need hormone therapy, medication, or any sort of quick fix to help her start puberty earlier. It was in many ways a lot simpler than that: she needed providers and a broader health care system that could recognize her need for mental health support and do something about it.
Featured photo by mododeolhar from Pexels.
My Fog is Feeling Very Brainy
By Carina Diaz (Texas, USA)
FYI, this is about brain fog (in case you’re confused about the title). It’s one of the most complicated symptoms to explain to able-bodied people, along with fatigue. Because anyone can feel those things, right? Well … kind of. A person with IBD experiences it very differently.
Since being on inflectra and having ileostomy surgery, my brain fog hasn’t been too bad, but it’s still something I feel often. Sometimes when I’m having a conversation with someone, it’s like my brain glitches for a moment, and I not only have to remember where I am, but what I was even saying a second ago. It causes me to stumble over my words and say “um” a lot. So much for sounding articulate. It also conveniently happens a lot at doctors appointments.
It’s true that anyone can have moments like these, but when you have IBD it’s a more common occurrence. I can get a full night’s sleep, eat right, exercise, and take care of myself as much as possible, but brain fog will still happen. I’ve lost track of the number of times I’ve opened an app on my phone or walked into a room just to forget what I’m doing in the first place.
This is a very hard symptom to put into perspective. It almost sounds like it’s not that big of a deal. Especially when compared to the laundry list of awful symptoms that IBD can bring. So let me try to paint a picture. For me, brain fog is like a cloud that follows me. Some days it’s big and other days it’s barely visible, but it’s still always following me around. I’ve learned I need to write everything down in my notes app and use Google Calendar to keep track of work and appointments, or else I’ll forget everything in an instant.
Brain fog mostly affects me in social situations. It’s very hard to follow along with conversations that involve multiple people. It’s as if existing, breathing, listening, and thinking are all too difficult to do at once. It tires me out, and the only thing I can really do about it is to take time to rest.
Instead of my brain forming thoughts, it feels like a big empty space. Or sometimes it’s the opposite and turns into that one episode from SpongeBob where there’s multiple filing cabinets on fire and he’s running around frantically. Nickelodeon
It also makes it difficult for me to communicate. The process of thinking thoughts, forming those into words, and then my mouth saying them becomes quit tedious.
It can be easy some days to feel very frustrated about dealing with this. These are some things that help me to deal with this symptom:
Being gentle with myself
Doing a brain dump in my journal or a voice note on my phone
Leaning on my community
Taking a nap
Brain fog is a friend I didn’t ask to make, so I just try my best to use the coping skills that I’ve learned over the years.