by Michelle Garber (California, U.S.A.)
Content Warning: this article discusses eating disorders and topics such as food restriction, binge eating, and body dysmorphia.
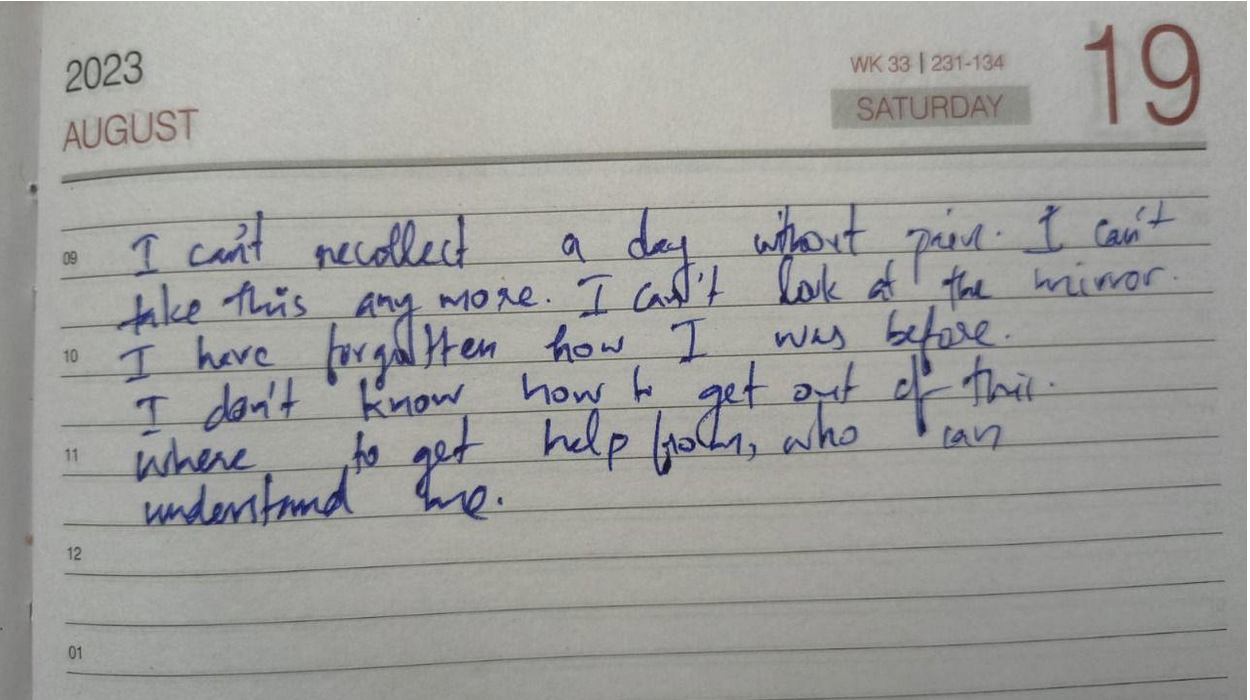
For as long as I can remember, food has never been just food. It has been comfort, control, fear, shame, and even the sole measure of my worth. I began struggling with disordered eating as a child, long before I knew anything about Inflammatory Bowel Disease (IBD) or ulcerative colitis—the chronic illness that would later reshape my relationship with my body all over again.
My earliest battle was with anorexia nervosa. I was only around twelve when I began restricting food, counting every calorie, and chasing the illusion of control that came with watching the number on the scale drop. Almost no one knew. The secrecy was part of the sickness—the quiet shame that thrived in silence. It felt safer that way. In a strange way, that shame felt familiar when I was later diagnosed with IBD. Both conditions carried a stigma. Anorexia was whispered about in terms of vanity and control, and conversations about IBD were avoided altogether because they involved the "uncomfortable" topics of bowels, bathrooms, and bodies.
By my senior year of high school, I had relapsed in terms of my anorexia. With prom and graduation approaching, I wanted to "feel confident" in my own skin, but my desire for control quickly turned into obsession again. I convinced myself that going vegan and gluten-free would "clear my acne" and "make me healthier." When it didn't, though, I continued anyway. I continued because I had found something else: the rush of watching the scale drop again. I told myself that it was about health, but deep down, it was about control, perfection, and fear.
When COVID hit, prom and graduation vanished, but my eating disorder didn't. Even though I eventually abandoned the vegan diet, my restriction continued. My hair began falling out in clumps. I was so weak that I needed to be pushed in a wheelchair on family walks and through grocery store aisles. Still, I clung to denial, blaming my fatigue and hair loss on my thyroid. I wasn't ready to admit that I was sick again—not from a medical condition, but from the same mental illness I thought I had conquered.
The human body can only endure starvation for so long before it rebels. Mine did—violently. The pendulum swung from restriction to bingeing. Binge eating disorder involves recurring episodes of eating large amounts of food rapidly, often to the point of physical discomfort, accompanied by feelings of loss of control and guilt afterward.
That was my reality. I gained weight rapidly and felt completely out of control. If anorexia gave me a false sense of control over my life, binge eating disorder stripped it away. I swung from one extreme to another, and both made me miserable. When the weight gain triggered the same familiar self-loathing, I spiraled right back into an anorexia relapse again—a vicious cycle of control and chaos that consumed years of my life.
Eventually, my body began to fail. My heart rate slowed to dangerously low levels. For the first time, I allowed myself to admit the truth: I did not want to die. Recovery, for me, began not with love for my body, but with the simple desire to stay alive.
I began eating again, slowly and carefully. On paper, it looked like recovery—my calories were adequate and my body was functioning. Mentally, though, I was still trapped. I measured every ounce of food, logged every calorie, and spent hours preparing meals to ensure perfect precision. I told myself that it was about maintaining my metabolism, but it was still about fear—the fear of losing control, the fear of gaining weight, and the fear of trusting my body.
Even when I was "eating normally," my life revolved around food. I avoided restaurants unless they posted nutrition information online. I sometimes ordered takeout, only to bring it home and weigh it myself. I had simply traded starvation for obsession. I thought that I had my eating disorder under control, but in truth, it still controlled me.
Around this time, I began experiencing digestive symptoms: constipation, vomiting, reflux, and pain. I now believe that my disordered eating—the pendulum swing from restriction to bingeing, my extremely high insoluble fiber intake in order to eat high volumes of food with the least amount of calories, and my reliance on laxatives due to my food restriction—played a role in triggering my ulcerative colitis, along with the mental/emotional stress caused by it all.
When I was finally diagnosed with IBD, I thought that my disordered eating would take a back seat. I was wrong. Chronic illness can be fertile ground for eating disorders to grow. The constant focus on diet, the fear of flares, and the unpredictability of symptoms can reawaken old patterns of control and restriction.
In the hospital, I was prescribed prednisone and given a list of "safe foods." Back home, I stuck to that list religiously. Underneath it all, though, my old compulsions still resurfaced. I limited not just insoluble fiber, spicy foods, dairy, and alcohol—which are common triggers during flares—but also carbs, sugars, and sodium. This was due to the fear of prednisone-induced weight gain—the water retention, "water weight," or "moon face" that prednisone could cause. I told others that it was about inflammation, but in truth, I was relapsing again—this time under the socially acceptable cover of a "medical diet."
This is one of the hardest truths about eating disorders and IBD: the overlap between medical management and disordered eating behaviors is often blurred. The two can feed each other in quiet, dangerous ways.
IBD can create new patterns of disordered thinking in people who have never struggled with eating disorders before. This is because when your body betrays you like it does with IBD, food becomes (or at least feels like) one of the few things that you actually can control. Plus, when your weight fluctuates rapidly—sometimes losing as much as thirty pounds in a week and then regaining it soon after—it can completely destabilize your sense of self.
For those with body dysmorphia or a history of disordered eating/anorexia, this is especially dangerous. There's no such thing as "small enough" in the mind of someone with an eating disorder. Seeing a "low" number on the scale (even when it's caused by illness) can increase your dopamine and ignite the urge to chase that number, again and again. I remember logically understanding that my low weight during my flare was unhealthy, but emotionally, I still felt anger and panic when the scale went up after treatment. Prednisone's mood swings certainly didn't help with this either—I was at war with both my mind and body.
Now, in remission from IBD, I can finally say that I am also in recovery from my eating disorders. Even so, recovery (like remission) is never as simple as it sounds.
Even in remission, disordered eating behaviors can quietly persist. For many of us with IBD, it shows up as hypervigilance around food: the fear of new foods, the obsession with "safe" meals, or the guilt after eating something "off-plan." It can look like avoiding social events involving food, fixating on weight fluctuations caused by steroids, or tying self-worth to whether symptoms worsen after a meal. These behaviors can masquerade as "caution," but they're often echoes of deeper fear—the fear of pain, the fear of loss of control, and the fear of being sick again.
The parallels between IBD and eating disorders are striking. Both involve an uneasy relationship with the body—a sense that your own physical self has turned against you. Both can make you feel powerless, trapped, ashamed, and isolated. Both can lead to cycles of control and surrender, as well as perfectionism and self-punishment. And both are often invisible to others, hidden behind a mask of composure and "doing fine."
Today, my relationship with food is no longer about control—or at least, I'm trying to keep it that way. I eat intuitively when I can, forgive myself when I can't, and I remind myself that nourishment is not a punishment or reward; it's an act of care. My body has been through battles most people can't see—battles maybe I never even noticed. My body deserves gentleness, not control or being told that it isn't "good enough." Yes, my body may have not been the kindest to me over the years, but I also haven't been the kindest to it in return. While my body may have betrayed me in some ways due to my IBD, it has also gotten me through my IBD, my eating disorders, and so much more. My body is not my enemy. My IBD is not my enemy. My weight is not my enemy. How I look in the mirror one day versus how I look in the mirror the next is not my enemy.
Living with both IBD and a history of eating disorders means constantly walking the line between vigilance and obsession, as well as between self-protection and self-harm. Even so, I've learned that healing is not about never struggling again—it's about recognizing when the struggle starts to whisper and, this time, choosing to listen with compassion instead of control.
For more information on disordered eating & IBD, check out this patient-created resource by the ImproveCareNow Patient Advisory Council.
Image from @jogaway on Unsplash.