by Beamlak Alebel (Addis Ababa, Ethiopia)
There are days that change us forever — not because we are not ready, but because life gives us no choice. For me, it was the day I faced surgery.
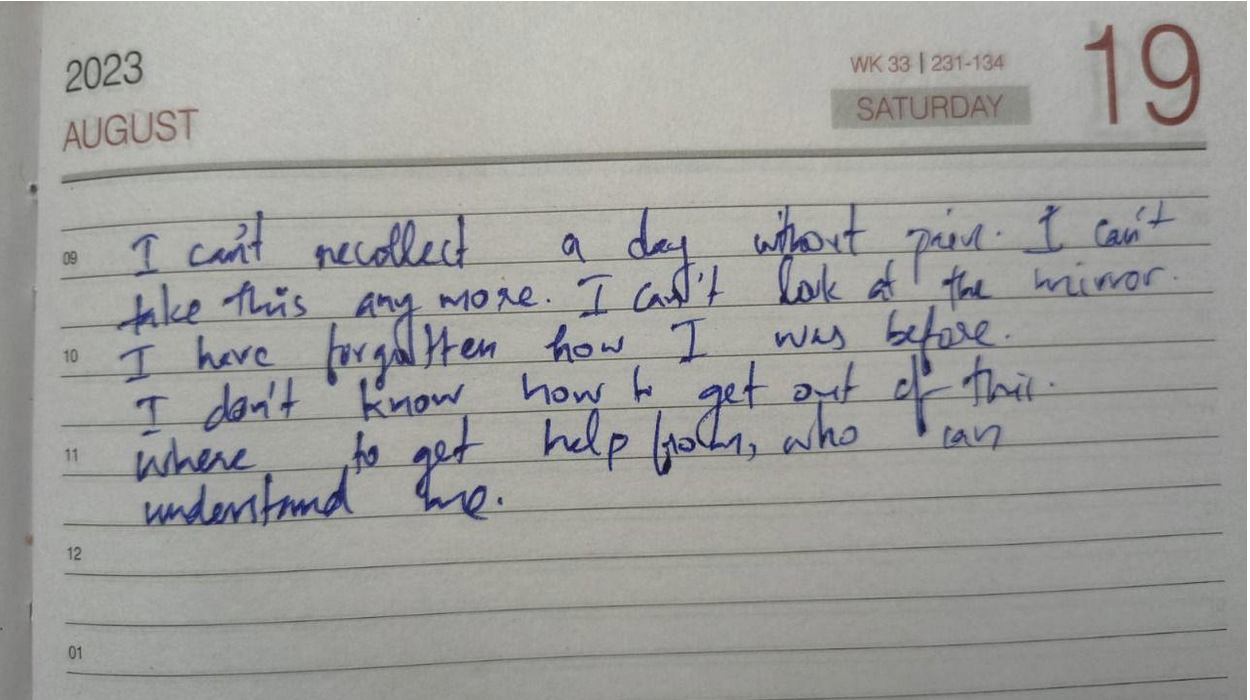
That moment came with fear, complications, and a sense of losing control over my body and even my appearance. I wasn’t prepared — not mentally, not emotionally. Yet I had to choose: risk everything or let everything fall apart.
Before that day, I never imagined hearing the words: “You may be moved to the ICU.” No one is ready for those words. Your heart races, your mind fills with unfinished dreams, and suddenly life and death sit together in the same breath.
But when that moment came, I made my choice. I chose life. Even with all the unknowns. Even with the pain. Because sometimes the bravest step you’ll ever take is the most uncertain one.
Over time, I learned that strength isn’t about muscles or energy — it’s about mindset. When your body feels defeated,your mind becomes your strongest weapon. Deep inside me, beneath all the fear, I found a hidden strength I never knew I had.
Yes, I cried. Yes, I doubted. But I rose.
Living with IBD has stolen parts of my childhood, but it has also taught me to fight. My strength didn’t appear overnight — it grew through countless painful moments that shaped me into the woman I am today.
And here’s the truth I want others to know: we don’t need approval from anyone to define us. We know our own limits, and we know our own strength. Scars don’t make us less — they prove we survived.
If you’re standing at the edge of fear right now, please remember: you are not alone. The fear is real, but so is your courage. Even when your body is tired, even when others don’t understand — your mind can carry you further than you think.
We are not broken.
We are not our scars.
Photo from @vicky49 on Unsplash.