NEWS
One Condition, Two Worlds, Shared Strength: Cross-continent experiences of living with IBD
by Beamlak Alebel & Kaitlyn Niznik
Kaitlyn’s experiences in the United States:
Living with microscopic colitis in the U.S. comes with its own challenges:
Months-long waits between doctor’s appointments
Expensive medications and treatments, especially without strong insurance
Delayed diagnosis despite advanced healthcare systems
Difficulty finding foods that align with dietary needs and aren’t overly processed
Being dismissed by others who don't understand the condition
A painful impact on social life and emotional well-being
Beamlak’s experiences in Ethiopia:
In Ethiopia, living with IBD means facing different (but just as heavy) burdens:
Widespread misconceptions: many believe it’s just stomach pain from bad diet
Medications are not only costly—they’re rarely available
IBD is seen as a disability, making it hard to find work
Employers are hesitant to hire people with chronic illness
Speaking openly often leads to judgment or silent gossip
There’s little public awareness, and support is nearly nonexistent
Surgery and pain are not just physical but emotional struggles too
Isolation is deep, and the future feels uncertain
Chronic illness carries stigma, creating silence and shame
Despite our different realities, our pain, fears, and desire to be understood are the same.
IBD knows no borders.
And neither does our strength.
We’re raising our voices—because IBD is real, painful, and deserves global attention.
By sharing our stories, we break the silence.
By standing together, we make IBD visible.
By speaking out, we show that shame fades when we are heard.
Let’s keep going. For ourselves. For each other. For every IBD warrior around the world.
Through
by Michelle Garber (California, U.S.A.)
World IBD Day is May 19th, and this year’s theme is “Breaking Taboos, Talking About It.” Here are 2025 CCYAN Fellow Michelle’s thoughts on stigma, shame, and talking about IBD!
Since being diagnosed with Ulcerative Pancolitis almost four years ago, I have been battling the shame that surrounds my symptoms. I often look back at who I was before my diagnosis—not only grieving that version of myself but also feeling ashamed that I can never fully be her again. Before IBD, I was fiercely independent, reliable, spontaneous, perfectionistic, energetic, athletic, social, focused, happy—and, most importantly, healthy. To put it into perspective: I was a straight-A student at a top magnet school in my district with a 4.44 GPA. I was simultaneously taking college classes, volunteering, traveling, going out with friends, exercising, and serving as the Secretary of my high school’s dance production team. Even during my first year of university—despite COVID-19 restrictions—I took 33 credits, earned leadership positions, made the Dean’s List, got straight A’s, moved into my own apartment, worked out consistently, and started two social work internships.
Then, everything changed. After my diagnosis, my life felt like it had been turned upside down—and in many ways, it had. For a couple of years, I had to move back in with my parents because I could no longer care for myself. There were days that I couldn’t brush my own hair or stand long enough to cook a meal or wash my face. If I needed to go to the hospital, I couldn’t even get myself there. I was fully dependent on my family when my IBD was active. That dependency alone filled me with shame. How could a nineteen-year-old not brush her own hair? How could I be so weak? While I managed to continue online school, I had to request disability accommodations from my university. I went from being someone who never asked for help to someone who needed it in nearly every part of her life. I no longer felt like myself. The woman I once was had seemingly vanished, and in her place was someone I didn’t recognize—someone who carried a constant, heavy shame.
Even now, despite being in remission for about two years, that shame hasn’t disappeared. It creeps in every time I’m too fatigued to answer a text or take a phone call—or worse, when I have to cancel plans. In those moments, I don’t just feel like a bad friend, I feel weak. I feel mentally, physically, and emotionally defeated. I question how someone like me, who seemed to once "do it all," can’t even hold a simple conversation anymore. That shame resurfaces every time I walk into my gastroenterologist’s office or sit in the infusion center waiting room. I think to myself, "Why am I here? I am so young, and yet I am sick. I must just be weak." Even when I pick up a stool collection kit at the lab, I look around, paranoid and embarrassed that someone might know what’s in that big, brown paper bag. I also feel ashamed of what I have to do with that kit once I get home. Especially on the days that I sleep late into the afternoon or feel too exhausted to shower, that shame becomes deafening. I can’t even manage basic self-care, and that makes me feel pathetic and exposed.
Unfortunately, I used to feel as though this shame only deepened when I tried to speak up about what I was going through. On a romantic level, I used to be extremely cautious about sharing my IBD with potential partners. This is because I didn’t want to feel embarrassed, and I certainly didn’t want to be rejected because of it. My first partner after my diagnosis knew all about my IBD. We joked about bathroom "duties" constantly—it was part of our daily rhythm. Beneath the humor, though, I knew that he wanted someone different: someone who could be spontaneous, who could have endless energy, who could cook large meals, who could host frequent gatherings, who could clean, who could work out with him, etc. That just wasn’t me anymore. I also knew that he didn’t want to be around if I ever needed to take Prednisone again since I had explained its emotional toll and side effects. Moreover, I knew that he would "never touch" me if I ever had to get an ostomy. So, I tried to be who he wanted—to become the woman I was before IBD—and for a while, I pulled it off. Over time, though, that relationship made me feel unaccepted—for who I was in that moment and for who I might become. It made me feel ashamed to be me—the real me. It intensified the shame I already carried about my illness.
Since then, dating has been rocky. I’ve met a few people who've responded with deep empathy and genuine interest, and for that, I am grateful. I’ve also encountered individuals who shut down any conversation about IBD out of their own discomfort, who incessantly question my fertility or the "quality" of my genes, or who firmly believe that "tooting" in private or using the word "poo" in a sentence would be impolite and inappropriate. For someone who loves deeply and craves a meaningful romantic connection, those reactions cut deep. They make me question and feel ashamed of the kind of partner I am—or could ever be. On a platonic level, things haven’t been easier. When friends or family joke about me "sleeping all day," "always being at home," "always needing the bathroom," "being forgetful," "not being fun," "eating boring foods," or about how my brother "takes better care" of my dog, shame crashes over me like a wave. I genuinely begin to drown in it. It’s one thing to feel shame for not meeting your own expectations—the ones you set when you were healthy. It’s another to feel shame when romantic partners judge you for something you didn’t even choose and cannot control. However, it’s something entirely different, and perhaps even more painful, to feel that shame reinforced by the people you love and value the most. When they unknowingly echo the same critical thoughts that I already battle every day, it doesn’t just hurt—it reinforces my shame and makes me feel weak and unworthy.
This compoundedness and deeply personal nature of this criticism take my shame and embarrassment to an entirely different level. The intensity of shame I’ve felt in these moments mirrors the shame I’ve carried throughout my journey with active IBD symptoms. It mirrors:
The shame I felt needing my loved ones to brush my hair;
The shame I felt crying, begging, and pleading with doctors for answers and relief;
The shame I felt discussing my symptoms with countless medical professionals;
The shame I felt from the burn marks and scars left behind by overusing a heating pad;
The shame I felt experiencing fecal incontinence;
The shame I felt wearing diapers for months;
The shame I felt needing to carry baby wipes, toilet paper, and a change of clothes;
The shame I felt when I could no longer clean myself without help;
The shame I felt asking my gastroenterologist to remove my colon;
The shame I felt when I began to question if life was even worth living;
The shame I felt being bedridden, needing a wheelchair just to get fresh air;
The shame I felt requesting accommodations from my university;
The shame I felt when a doctor asked me why I waited so long to seek help.
Still, I continue to grieve the version of myself I once was, and I wrestle with the shame of not being able to live up to that image again. Feeling stuck in your own body when your mind wants to do so much more is an agonizing experience. I acknowledge that fully. Yet—despite my doubts—those feelings of shame began to fade away as my symptoms have lessened and as I’ve found my voice within the IBD community. I've recently been able to feel pride when comparing the person I once was to the person I am today. No, I may never again be the energetic, healthy "yes woman" I once was. Nevertheless, I wouldn’t have the resilience, empathy, and sense of purpose I now carry if not for IBD. Fighting for your life, navigating a new reality, and battling stigma while the world moves on without you teaches you something profound: you are capable of surviving the unimaginable.
With this new revelation and mindset, I've come to see how my feelings of shame and beliefs of being weak/perceived as weak are rooted in fallacy because:
To cry in front of doctors and explain your symptoms is not shameful—that's strength.
To be vulnerable and advocate for yourself is not shameful—that's courage.
To decline a call, cancel plans, say "no," and set boundaries is not shameful—that's self-respect.
To rest rather than push through the pain is not shameful—that's self-love.
To wear diapers and pack supplies to manage your day is not shameful—that's determination.
To request or actually go through a life-altering surgery is not shameful—that's bravery.
To need and/or ask for help is not shameful—that's survival.
To live in a body that is constantly fighting against you is not shameful—that's perseverance.
To choose life every day, despite IBD's messiness and pain, is not shameful—that's resilience.
Furthermore, I believe with all my heart that talking openly about IBD—the good, the bad, and the ugly—is one of the greatest testaments of one's strength. Whether it's with friends, partners, family, co-workers, medical providers, or strangers, it takes immense courage to be that vulnerable. This is because, in all honesty, there is risk involved. As human beings, our minds can sometimes jump to the worst possible outcomes. When it comes to talking about IBD, there's the risk of being judged, pitied, and misunderstood. There's the risk of "becoming" your diagnosis and of losing relationships or job opportunities due to stigma. These fears are real and valid, and they’re exactly why many IBD patients tread lightly when sharing their stories. As a result, though, we often overlook the best possible outcomes. From experience, I know that talking about your IBD can: help you feel more at home in your own body; help you feel accepted for who you truly are rather than who people want you to be; help you find community; help shine a light on the genuine/empathetic people in your life; help create space in your mind for something more than just survival; help break the stigma; and help pave the way for earlier diagnoses, better treatments, and stronger support systems. Sharing your story doesn’t make you less—it makes you more. Sharing your story makes you more human, more whole, and more you than you had ever thought possible.
Taking all of this into account, I’ve come to recognize how powerful it can be to talk about IBD and share your story. If the worst that can happen is being judged, excluded, misunderstood, or left, then maybe talking about your IBD is a blessing in disguise. I know that speaking openly about my IBD has saved me from dedicating my energy and love to people who didn’t deserve it. If the best that can happen is finding your people, becoming more comfortable with your diagnosis and yourself, getting care faster, and helping to break the stigma, then sharing your story might actually be a superpower. We, as IBD patients, are in a unique position to educate and advocate—not because it’s our responsibility, but because our lived experiences often speak louder than medical textbooks ever could. I wish we lived in a world where everyone understood IBD, where institutions offered protection, and where systems were built to accommodate us. The truth is, though, most people just don’t know where to start. They rely on what they read online or hear in passing. It’s easy to see how misconceptions and stigma grow. If I read online that remission meant "no symptoms and a healthy colon," I probably also wouldn’t have much empathy for someone in remission who still canceled plans or needed extra rest. As someone in remission who is sharing her story, though, I can tell you one thing: that version of the story isn’t quite right. Nothing about IBD is so black-and-white. Everyone’s experience is different, which is why personal storytelling matters so much. Doctors, loved ones, and even other patients learn from us as IBD patients. So many vital conversations—about non-textbook flare symptoms, about “safe foods,” about unspoken medication side effects, and about what remission really looks like—don’t come from medical journals; they come from people with IBD who tell the truth about what it’s actually like. Without these stories, diagnosis and treatment can be delayed, and support systems stay broken. It’s not our job to fix the system, but by speaking up, we might just make it easier for those who come after us. We might even make it easier for ourselves in the future.
For a disease that has made me feel powerless more times than I can count, finding power with or over my diagnosis has been invaluable. Talking about IBD has helped me reclaim my own narrative. People can still judge me, but at least they’re judging something real. If someone can’t handle a story of resilience, that’s on them. No journey of survival is without its dark moments. Most movements worth remembering were forged in hardship.
That said, I don’t want to pretend it’s easy. Even now, I still struggle to talk about my IBD. I just recently began experiencing symptoms of a flare, but I only told my doctor and loved ones after a delay. This was not out of embarrassment, but out of fear—the fear of returning to that time when I felt that I had lost all independence, the fear of being blamed, and the fear of blaming myself. There’s a voice in the back of my mind that whispers, "You should’ve taken better care of yourself. You should've been stronger." And although I know that’s not true, it still stings.
Even with that fear, though, I eventually reached out because I’ve learned what happens when I don’t. I know now that silence doesn’t save me. Hiding doesn’t protect me. Every time I have tried to ignore a symptom or push through for someone else’s comfort, I’ve paid for it tenfold. I've realized that delaying diagnosis and treatment is, quite frankly, not worth anything. So, I’ve started doing the hard thing: I've started telling the truth. I’d rather speak up than wait until things become unmanageable because the truth is, IBD is messy. It’s not just a bathroom disease. It’s not just about inflammation or test results. It’s about what it does to your relationships, your identity, and your sense of safety in your own skin. It’s about mourning the life you thought you would have, and then figuring out how to build a new one—without pretending that the old one didn’t matter. It’s also about power—quiet power. This is the kind of power you reclaim when you speak up, when you stop hiding, and when you say, "Here’s what I’m going through," even if your voice shakes.
I know what it’s like to walk into a doctor’s office, share your story, and be dismissed. I know what it’s like to be lonely in a room full of people who love you. I know how scary it can be to share what you're going through. At the same time, I also know how healing it can be. Talking about your IBD—when you’re ready—can give you strength with the diagnosis and over the stigma. That kind of power is slow and sacred. It doesn’t always feel good, but it builds something stronger than "perfection" and "control." It builds truth. When I tell my story, I don’t just feel more seen. I also make space for other people to show up with their stories. Sometimes, your courage can be the reason someone else finds theirs and feels less ashamed. The more we speak, the less shame survives. The more we share the parts of IBD that don’t have tidy endings, the more human this disease becomes rather than being a punchline of a joke or a pity project. There are days that I still feel afraid—afraid of being judged, misunderstood, and left behind. Even so, I’m more afraid of going through this alone. If my story can be a hand reaching out to someone else in the dark, then I’ll keep telling it—again and again. At the end of the day, I truly believe that the only way out is through, and for me, the "through" begins with sharing my story.
Flare-up: A Downward Spiral
by Akhil Shridhar (Bengaluru, India)
It all begins with a flare-up. For most of us, the diagnosis comes only after enduring symptoms for days or months, dismissed as a stomach bug. But when the discomfort escalates into a significant disruption, we hear the term “flare-up” for the first time. The symptoms build like a chain reaction, growing worse until urgent medications—usually steroids or antibiotics—are prescribed for relief.
Difficulty with Food
Almost every food item can trigger nausea or an urgent trip to the restroom, making nutrition a frustrating challenge. While some believe short-term food restrictions might ease inflammation, prolonged deprivation causes more harm. In countries like India, navigating diverse dietary recommendations complicates matters. As newly diagnosed individuals we often seek advice in support groups, hoping for recipes or meal plans that won’t worsen symptoms. But in most households, skipping meals isn’t acceptable. Our parents insist on “good food,” unaware that their concern often fuels the next domino.
The Washroom Runs
Initially, the frequent restroom trips are an inconvenience—but soon, they dictate life. The unpredictability makes outings stressful, and hesitation around food becomes constant. Exhaustion follows, leaving us dehydrated, fatigued, and mentally drained. The cycle feeds itself: eating triggers symptoms, symptoms disrupt daily activities, and fatigue makes even basic tasks overwhelming.
The Mental Toll
Beyond the physical struggle, IBD takes an emotional toll. The anxiety of unpredictability, the frustration of adapting to a condition that doesn’t follow rules, and the isolation of feeling misunderstood weigh heavily. Conversations become filtered—friends may not fully grasp the challenges, and outings are haunted by the fear of urgently needing a restroom.
Sleep Struggles
IBD doesn’t stop at meals—it disrupts rest too. Pain, restroom trips, and anxiety make sleep elusive, worsening inflammation and fatigue. Poor rest perpetuates the cycle, making daily recovery harder. Many of us try strict bedtime routines, meal adjustments, or sleep aids to reclaim rest. While perfect sleep remains rare, small efforts help ensure the limited hours of sleep offer some recovery.
Finding Balance
What I have realised after a few misadventures is that the best way to get out of this spiral is to consult your medical team and get the required medications right away. The damage that prolonged inflammation has is quite severe and takes months if not years to reverse, sometimes is unfortunately irreversible, therefore it is not worth the risk of ignoring it.
IBD is unpredictable and exhausting, but it doesn’t define life. Over time, we find dietary adjustments, support systems, and coping mechanisms to regain control. Gradually, these adjustments help restore control—accepting the hard days, seeking support, and celebrating small victories. While flare-ups will always come and go, so does recovery. Life continues, not perfectly, but uniquely. And within that cycle, resilience proves stronger than the condition itself.
Image from meister_photos on Unsplash.
Internalized stigma in IBD, mental health, and quality of life: A study review
by Aiswarya Asokan (South India)
Living with IBD comes with a lot of constraints that no one prepares you for. Every time one goes through a major life transition like starting college, joining work, or getting into a relationship, adapting to the changes is never easy. It’s often difficult to fit in due to our IBD, which in turn puts us under a lot of stress and anxiety. Research indicates that bowel-related issues are a widespread cultural taboo and historically, IBD has been seen as “psychosomatic,” further stigmatizing the condition.
To learn more about this, I read a paper titled “The mediating role of psychological inflexibility on internalised stigma and patient outcomes in a sample of adults with inflammatory bowel disease.” This study was conducted to examine the relationship between ‘psychological inflexibility’ (when someone struggles to adapt to challenges, avoiding emotions or feels stuck) and ‘internalized stigma’ (when individuals adopt negative societal beliefs or shame as their own, and devalue their identity) on health outcomes. The authors looked at outcomes like mental distress (depression, anxiety, stress), health related quality of life, self-efficacy, self-concealment (hiding personal information that is distressing or negative from others), beliefs about emotions, and fatigue (physical and mental) in adults with IBD using an online survey of 382 participants.
This study suggested that:
Adults with IBD who had higher rates of psychological inflexibility also had higher rates of internalized stigma, negative beliefs about their emotions, self-concealment, mental distress, fatigue, and impaired quality of life.
Psychological inflexibility was inversely related to committed action, stigma resistance, and IBD self-efficacy.
Adults with IBD who had higher rates of internalized stigma also showed higher rates of mental distress, self concealment, negative beliefs about their emotions, fatigue, and poor health-related quality of life.
Internalized stigma was inversely correlated to stigma resistance, IBD related self-efficacy, and committed action.
Participant’s age and educational level showed an inverse correlation with their psychological inflexibility. Their IBD severity (in the past 3 months), the presence of an ostomy, and their COVID-19 self-isolation status were positively correlated.
Internalized stigma was higher for individuals with an ostomy, those currently taking steroids, who had experienced severe IBD in the past 3 months, and who were more self-isolated, whereas educational level was inversely correlated.
Other interesting insights from this study:
Individuals who face discrimination regarding their IBD, who are less able to employ ‘flexible’ responses may spend more energy avoiding stigmatizing experiences, making it harder for them to engage in meaningful activities.
New research indicates that general familiarity with IBD can help reduce public stigma; highlighting the importance of IBD awareness campaigns to increase public understanding of IBD, thereby reducing stigma.
These study findings suggest that lower levels of internalized stigma is associated with increased psychological flexibility and better patient outcomes. Modalities of therapy like ‘Acceptance and Commitment Therapy’ (ACT) – which aim to increase psychological flexibility by changing individuals’ relationship with their thoughts, feelings and behaviors – may be a helpful intervention.
Personally, years of living with IBD have enabled me to build a circle of people where I can take my armor off. But still, going through repeated flares, body image issues, breaks from education, social isolation, and being under steroids takes a toll on my mental health and quality of living. Often the medical team's support stops once your blood counts are under control, leaving us with the responsibility of picking up ourselves and moving on with the new normal.
Citation:
Reynolds DP, Chalder T, Henderson C. The mediating role of psychological inflexibility on internalised stigma and patient outcomes in a sample of adults with inflammatory bowel disease. J Crohns Colitis. 2025 Apr 1:. doi: 10.1093/ecco-jcc/jjaf055. Epub ahead of print. https://pubmed.ncbi.nlm.nih.gov/40168103/
Photo from “Total Shape” on Unsplash.
Life with Crohn’s – A Pantoum
by Alexis Gomez (California, U.S.A.)
This is your life now.
The burning and belly aches
instigated by none other than Crohn’s,
your forever counterpart.
The burning and belly aches,
the appointments, calls, meds, side effects.
Your forever counterparts are
memories of you in both sickness and health.
The appointments, calls, meds, side effects
force you to advocate for yourself like never before.
Memories of you in both sickness and health
remind you how quickly life can change.
You’re forced to advocate for yourself like never before but
it makes you stronger.
You’re reminded how quickly life can change,
how the world doesn’t pause when you need it to.
It makes you stronger–
the moments of grief and relief.
The world doesn’t pause when you need it to, but
you can savor times of joy and give yourself grace.
The moments of grief and relief
are ever-present with IBD.
You can savor times of joy and give yourself grace.
You deserve it because
this is your life now.
What It’s Like Working Through Phobias: Creating A Comfort Toolkit
by Kaitlyn Niznik (New York, U.S.A.)
I can't remember a time when I didn't have a blood/needle/medical phobia. I would regularly faint at the doctor's office and even talking about blood was enough to make me pass out in high school. It wasn't a problem until I developed chronic stomach issues and was diagnosed with microscopic colitis. All of the sudden, I was pushed headfirst into a world of doctors' appointments and countless medical tests. It's hard enough to find answers from doctors, but fear can make you ignore your problems, making things worse. I still struggle with this phobia today, but with the help of a therapist, I’m working through my issues. Please seek the help of a trained professional to face your phobias in the safest way possible. Here are several strategies I'm using to make progress facing my fears.
Desensitization Training/ Exposure Therapy
Desensitization and exposure therapy can start with looking at images of videos of your phobia, eventually progressing to more realistic scenarios. For instance, someone with a blood phobia might progress from viewing images to medical shows and eventually going to blood drives. The overall goal might be to get bloodwork done, but you have to build up exposure over time to get more comfortable with your fears.
I've been unknowingly trying to do this my whole life. As a kid, I would reread veterinary books to expose myself to a little literary medical gore. I would deem it a success if I didn't get woozy. Today, medical imagery has become an inherent part of my artistic practice. I find exposure more palatable if I attempt to explore images and procedures from a place of curiosity rather than fear. If I'm looking at veins, I try to ask myself what colors I see under the skin. I've progressed to the point where I can look at surgical photos of arteries and attempt to draw them without getting queasy. It's easier for me to separate myself from a picture than a procedure happening to me, so that's where my exposure therapy has started.
Working with a therapist, I did a deep dive on my phobias and my hierarchy of fears. Instead of just seeing all situations surrounding blood or needles as being equally terrifying, I was able to sort them into a list of situations with varying intensity. While younger me thought a finger prick was the worst situation possible, I now list it much lower on my list, opting to put IVs in a higher position. It's all a matter of perspective. By making a fear hierarchy, I was able to tackle lower intensity situations and gain confidence and resilience before braving my top fears.
Keeping A Sense Of Control
When I was little, my family had to trick me to get me in the doctor's office. In adulthood, I tried to mimic this strategy by being spontaneous. Instead of scheduling a flu shot and worrying about it for weeks in advance, I'd wake up and decide to go that morning. This strategy somewhat lessened my stress, but it also felt too hurried. I never had a sense of control, just urgency to get it done and over with. It didn't leave me in a good headspace and I still found myself fretting over the possibility of getting a shot for weeks ahead of time.
Now, I'm better prepared. With the help of my therapist and journaling, I've made lists of what is within my control during doctors’ appointments. I keep a “comfort bag" ready and always bring it with me to appointments. If I need blood work, I pack my own snacks for afterwards and plan to reward myself with a sweet treat from a nearby cafe. I also pick out my "victim” arm ahead of time based on which arm feels stronger than day.
When it's my turn for bloodwork, I tell my nurse right away that I'm terrified and I'm a faint-risk. I also ask for the reclining chair when possible. It's not so upright that I'll get dizzy and slump over, but through experience, I've also found that fully lying down feels more vulnerable and heightens my fear. A reclining chair puts me in a better headspace, so it is important that I advocate for my preferences. Doing small things consistently and giving yourself small choices in your healthcare can help you feel more in control and you'll know exactly what to expect.
Pack A Comfort Bag, Activate Your Senses
In an effort to ground myself, I try to pack things in my bag that activate my 5 senses of sight, sound, smell, taste, and touch. I always have these items in a bag and ready to go. Consistency is key, so I bring them with me to all of my medical appointments. When I’m in the waiting room, I grab my headphones and put on some music. I also pack sensory items that are calming like fidget toys to distract myself with. If I’m getting blood drawn, I have a tennis ball handy that I can grip, tissues for when I cry, and a snack for when it’s all over. This kit can be any size and it should be personal to you. Here’s a list of what I keep in my bag:
Snacks
Water
Tissues
Tennis ball (to grip)
Lavender essential oil
Hand warmer
Electrolytes packet
Fidget toy or comfort object (worry stone)
Headphones for calming music or ASMR
Don't Just Wing It, Strategize
Plan out your day ahead of time. Plan to have downtime afterwards to chill, recover, and reward yourself. I like to have a friend or family member drive me to and from appointments just in case I feel dizzy afterwards.
Pressure therapies or tense & release exercises have also been proven to help calm the body. Box breathing is another exercise to keep in your toolkit. It can stop you from hyperventilating and keep you calm. Make sure to try these techniques out BEFORE an appointment or exposure to your phobia. Practice makes perfect and not every therapy works for every person. Find what fits you and make a plan to tackle your phobias.
God of Small Things, Arundhati & THE LOVE EQUATION - A Crohn’s View
by Rifa Tusnia Mona (Dhaka, Bangladesh)
Stigmas Have Power! You might wonder why I say this as an IBD advocate. After all, stigmas are often baseless and untrue. But when they come at you from all directions—constantly, persistently—they start to wear you down. That’s when the real distraction, aka destruction, begins.
Imagine this:
One morning, you wake up feeling like something is coiling and twisting inside your stomach. You can’t eat. Or if you do, your body refuses to digest. Nausea takes over. You vomit again and again. The cramps hit without warning, stabbing, vanishing, then returning like waves from a storm. You feel trapped in a body that’s turning against you.
At first, people think it’s temporary—just a bug, maybe food poisoning. But then, something changes. The concern fades, and in its place, they start labeling you.
One morning, your mother decides to take you to church. If you’re Muslim, maybe it’s a hujur or a Sufi healer. Neighbors drop by. They don’t bring comfort; they bring unsolicited advice. "Have you tried this doctor?" "You should pray more."
Later, one morning, you find yourself lying in a hospital bed. A nurse enters and says, “Ask God for forgiveness.”
It hits differently. You’re not just battling a disease anymore—you’re battling judgment.
That’s the thing about stigmas: they’re powerful because they echo from everywhere. Different mouths, same message. And it always seems to come when you’re at your weakest.
But the hardest part?
When it comes from the people you love—your friends, your family—the ones who’ve always stood by you. That’s when the real confusion begins. You think, They care about me. They’ve never meant me harm. So maybe… maybe they’re right?
And just like that, you start to question yourself—not your illness, but your worth.
It took me a long time to realize that human minds are incredibly complex. I used to carry the weight of every cruel word, every dismissive act, thinking I must’ve done something to deserve it. But over time, I began to understand: most of the time, it’s not about me.
People don’t always act from a place of clarity or kindness. Sometimes, they hurt others to soothe an old scar within themselves. Sometimes, they mirror the pain they once suffered. And sometimes, they hurt simply because they don’t know how not to.
That’s when it hit me—pain is transferable.
It doesn’t just live in one person; it moves, it multiplies, it morphs into behaviors, into beliefs, into judgment. And many of those who hurt us are, in fact, carrying unresolved pain of their own.
“The God of Small Things” by Arundhati Roy feels like a masterpiece to me—layered, lyrical, and hauntingly beautiful. But if I had to pick one part that truly stayed with me, it would be the part about what Roy calls ‘The Love Laws’—or, as I like to think of it, the unspoken equation of love.
“That it really began in the days when the Love Laws were made. The Laws that lay down who should be loved, and how, And how much.”
-Page 33, Chapter 1, Paradise Pickles and Preserves, The God of Small Things
According to this idea, the amount of love we receive can sometimes feel predetermined—set by invisible rules we never agreed to. From Arundhati Roy’s words, I understood that love is often measured through two things: care and concern. These are the true units that define the depth of a relationship.
For love to feel genuine and meaningful, both must be present—together. When only one shows up, or when they're offered inconsistently, the relationship starts to feel imbalanced. It turns into something less whole, something we try to justify as "complicated" or label as, “Please, try to understand.” But deep down, we know—it’s a compromised connection.
“After Ammu died (after the last time she came back to Ayemenem, swollen with cortisone and a rattle in her chest that sounded like a faraway man shouting), Rahel drifted. From school to school. She spent her holidays in Ayemenem, largely ignored by Chacko and Mammachi (grown soft with sorrow, slumped in their bereavement like a pair of drunks in a toddy bar) and largely ignoring Baby Kochamma. In matters related to the raising of Rahel, Chacko and Mammachi tried, but couldn’t. They provided the care (food, clothes, fees), but withdrew the concern.”
-Page 15, Chapter 1, Paradise Pickles and Preserves, The God of Small Things.
There was a time when I was hospitalized for over a month. My father had a full-time job, and my mother had to juggle between caring for me and my younger sister. With both of them stretched thin, I reached out to every friend and relative I knew, hoping someone could step in as a caregiver. But no one came forward.
I was already battling an undiagnosed illness, and on top of that, navigating hospital departments alone, collecting test results while being so physically unwell—it felt like walking through fire. In that moment, a thought struck me hard: “After living over two decades, have I still not understood the love equation?”
Living with a chronic condition like Crohn’s has, in a strange way, been like being handed a special lens. I began to see certain relationships for what they truly were—fragile, one-sided, and built on illusions. That clarity gave me the strength to say “No” and walk away from connections that no longer served me.
It might sound harsh, but when your body is already carrying so much pain, the weight of empty relationships and unmet expectations becomes unbearable. Letting go became a form of relief, a way to breathe again. I’ve come to believe that sometimes, releasing old bonds opens up space for new, more meaningful ones. And life, quietly but surely, moves forward.
In a world where being "different" is often taboo, genuine relationships—the ones rooted in care and understanding—can feel like a warm shield. They make all the difference.
These are just my reflections, and as a reader, you’re welcome to hold your own. But thank you for making it this far—I appreciate your presence here, and I hope to meet you again in my next write-up.
Featured photo by Kaboompics.com from Pexels.
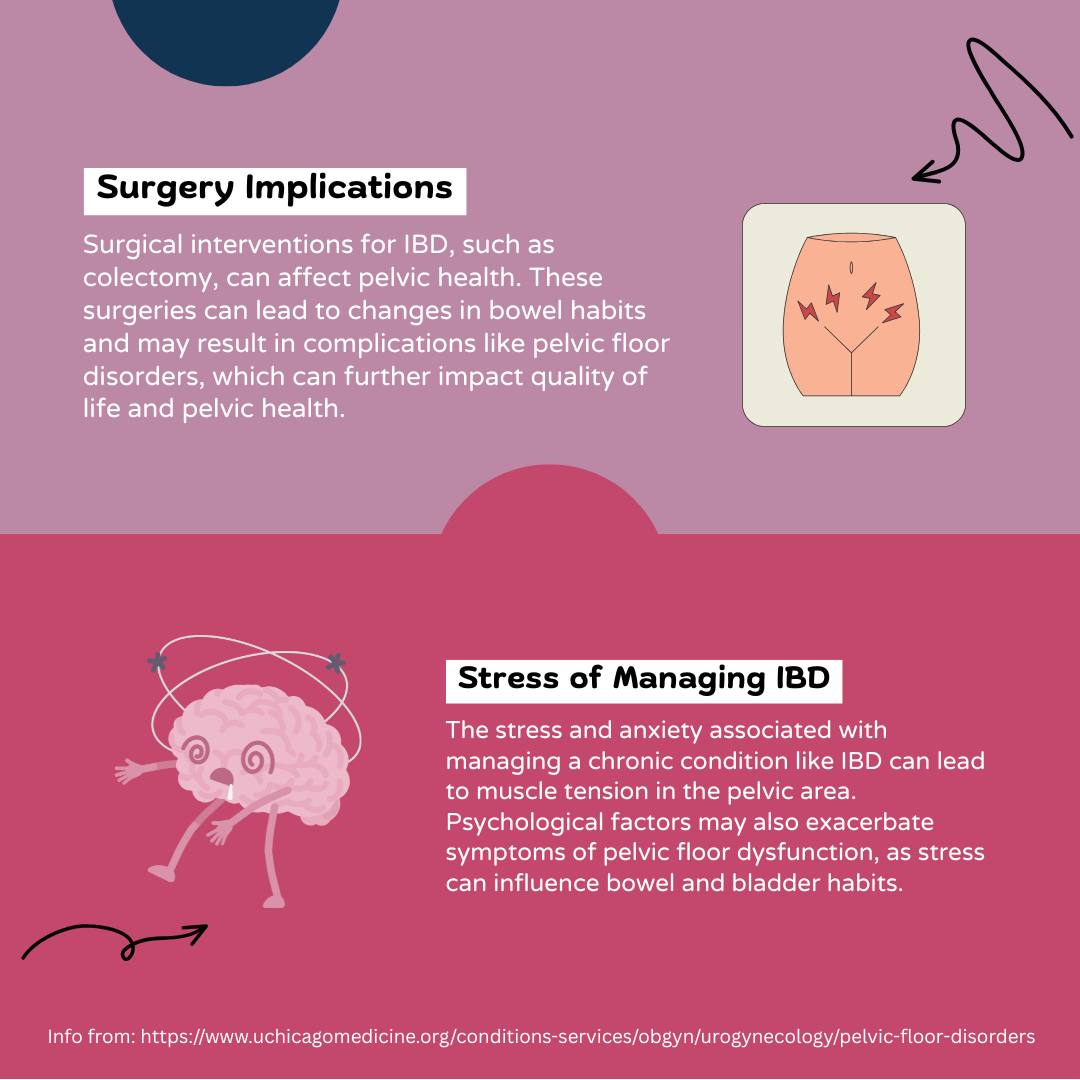
Pelvic Health and IBD: An Infographic
by Lexi Hanson (Missouri, U.S.A.)
Info from: https://www.uchicagomedicine.org/conditions-services/obgyn/urogynecology/pelvic-floor-disorders.
I am more than what you see: Living with IBD body changes
by Beamlak Alebel (Addis Ababa, Ethiopia)
Living with inflammatory bowel disease, my body has changed in ways I didn't choose. People see my outward appearance and make assumptions. Often, they don't wait to hear your story, and they judge you based on your size or looks: no words, no chance. It hurts because words can't always express what we feel inside.
They don't see the battles I fight every single day. I’ve heard it all:
"You are too skinny."
"You don't look strong."
"You must not eat enough."
But I know myself - I am strong. My journey is filled with courage, healing and hope. I don't have to be judged by my size, I am more than that. My size doesn't define my strength, my resilience does.
I have faced many tough times, but people don't see me as a serious person because of my appearance. I have survived painful flare ups, countless hospital visits, difficult medication side effects, surgery, and emotional lows and that could have broken me.
And yet, I am still here: still standing, still fighting.
I may not have a body society views as "tough," but I carry strength in my spirit.
I carry it in my story.
Being judged by my body and appearance has been painful, but it has also taught me what really matters: my ability to rise again and again.
I am not a slab of meat to be consumed or judged. Your power lies in what you overcome, not in the size of your frame or your appearance. We are more than our bodies, we are warriors.
No one knows what tomorrow holds, and what we have today is not guaranteed. Life changes, and bodies change, but our worth remains. Let’s learn to see beyond appearance, and appreciate our strength. We never know the silent battles someone is fighting – behind every look, there is an untold story.
Photo by Unsplash.
Michelle’s IBD “Burn Book”
by Michelle Garber (California, U.S.A.)
Inspired by Mean Girls and high school yearbooks, I created an “IBD Burn Book” to shed light on the invisibility of IBD and emphasize the importance of empathy when interacting with someone with IBD.
When you first open the Burn Book, you’ll see that my “Mask” has been crowned Prom Queen. The images on this page are from moments when I had my mask on—when I pretended to be “fine.” The background words reflect how others perceive me more positively when I wear this mask, which is why it was elected Prom Queen.
The next page is a Student Feature of my Inner Thoughts. Here, I am without my mask. This contrast serves as a reminder that appearances can be deceiving—what you see on the outside isn’t always real; it might just be a mask.
Following that is a Not Hot List, which consists of a collection of phrases people should never say to someone with IBD. (Sadly, every one of these remarks has been said to me).
The final page of the Burn Book is a WANTED poster—for empathy. Instead of harmful comments, this page lists empathetic phrases one should say to someone with IBD. Essentially, it serves as the “Hot List” in Mean Girls or high school terminology.
———
Invisible illnesses come with their own set of challenges—such as a widespread lack of awareness—but the focus here is how easily someone with IBD can hide their struggles. Smiling through the pain, pretending to feel well—it becomes second nature. I’m not the first person to wear a “mask” to feel accepted or to make others comfortable, and I certainly won’t be the last.
The reality, though, is that IBD is a constant battle. Even if you see me dancing with friends, traveling, or enjoying a big meal, I am still struggling. The takeaway? You never truly know what someone else is going through, so always choose kindness. More importantly, choose empathy. If you do know what someone is going through (specifically IBD in this case), be especially mindful of your words and actions. While you might assume your words and actions don’t affect us, remember—we’ve had a lot of practice hiding our pain.