by Aiswarya Asokan (South India)
It was on May 2nd 2016, a day before my 19th birthday, for the first time in my life, I heard the word Crohn’s, from my doctor back then. It came as a scientifically valid explanation to all the so-called “sick drama” I was exhibiting through the years. But the excitement of this achievement soon faded away when I came to know that there is no cure for this. Then came the joint family decision, we will keep this diagnosis a secret to ourselves. Anyways, who is going to accept me if they know I have got a disease that makes me run to the toilet and that I have to be on regular medication to stop this from happening. For the next 4 years, I lived like a criminal, fearing for every breath this crime will be caught. In between, I was ill informed about the dietary restrictions I was supposed to follow, and kept eating triggers from time to time, meanwhile wondering why this is happening – but was still focused on keeping the secret safe.
Still, life was a smooth sail with a few days of bad weather here and there, till 2020, when I had my worst nightmare: a serious flare that left me hospitalized for more than 2 months and unable to take my final year university exams. And my secret was out. Not being able to appear for exams was too much for an academically excellent student like me. I was experiencing such intense pain that I couldn’t even turn sides in bed. All this made me question my identity and shattered my fundamental belief system. None of the medicines were working on me. A group of surgeons visited me, and told me that if surgery was attempted, my life might be over on the table. When I realized I might die soon, I decided to live a little. Even though I was not able to eat anything, I ordered a red velvet cake and ate it. The 2020 Tokyo Olympics were going on – it was my all-time wish to watch the Olympics live, but my academic schedule did not allow me to do so. So from the hospital bed, I watched Neeraj Chopra win a gold medal for India, while all my classmates were taking final year exams.
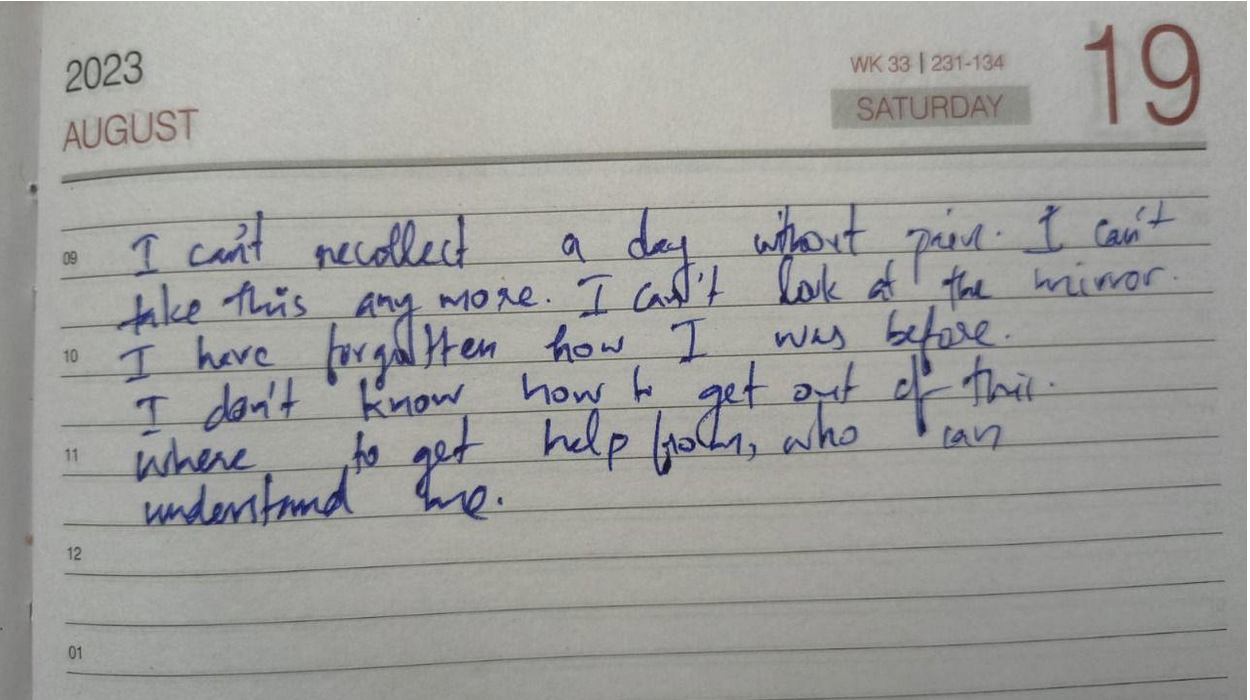
After a while, steroids started working and I started getting better. At the age of 23, I was 33 kilograms, severely malnourished and on a high dose of medication. I was not afraid to die but coming back to normal life was a challenge. I couldn’t face people nor attend phone calls. Even notifications from messages were alarming for me. I zoned out from everyone around me. I felt myself as a complete failure.
One person kept on calling me, despite me ignoring all their calls, until one day I finally picked up. He was my childhood bestie, who stood with me till I was able to manage things on my own. He made a timetable for me, which included slots for physical activity, exam preparations, and fun activities, and made sure I followed them on a daily basis. Then the exam date came up. There were times when I took supplementary exams alone, in a hall that usually accommodates 60 students. Everyday after the exam, he would ask me how it went, and suggest a movie to watch as a reward for the hard work. After a while, exam results came, and I had the highest score than previous years. Life was again on.
Whenever a flare up hits me, the first thing I notice is a keen desire for physical touch, especially a warm hug, though it sounds strange. I also clench my jaw while asleep, to an extent that my whole face and ears start to hurt the next morning, which further makes it hard to have food. Within the next 3 years, time was up again for a rollercoaster. I had a stricture, unbearable pain, my oral intake was nil, and I had to go for a hemicolectomy. The anticipated complications for the surgery were extremely frightening. This time my boyfriend came up and assured me that “no matter what, I will be there for you.” The surgery went smoothly and I was discharged. I was physically fit but started experiencing PTSD-like symptoms. I started feeling I was just a financial burden to my family.
I slept all day and night as I was not ready to face the thoughts in my head. My boyfriend used to call me every day – just for those few moments I was living, but the rest of the time I used to sleep. This time no friends nor family could help me. Then I started searching for IBD support groups, came to know about IBD India, took the free mental health counselling, and joined the peer group. For the first time, I felt less isolated and felt a sense of belonging. And slowly I replaced my coping mechanism of sleeping with painting. Gradually I was healing, and started feeling more freedom like never before.
Life goes on. Ups and downs are part of it. But when one door closes the other opens. When you feel stuck, ask for help and keep asking until you get one strong enough to pull you out — that is the bravest thing you can do for yourself.
Image from Unsplash.