NEWS
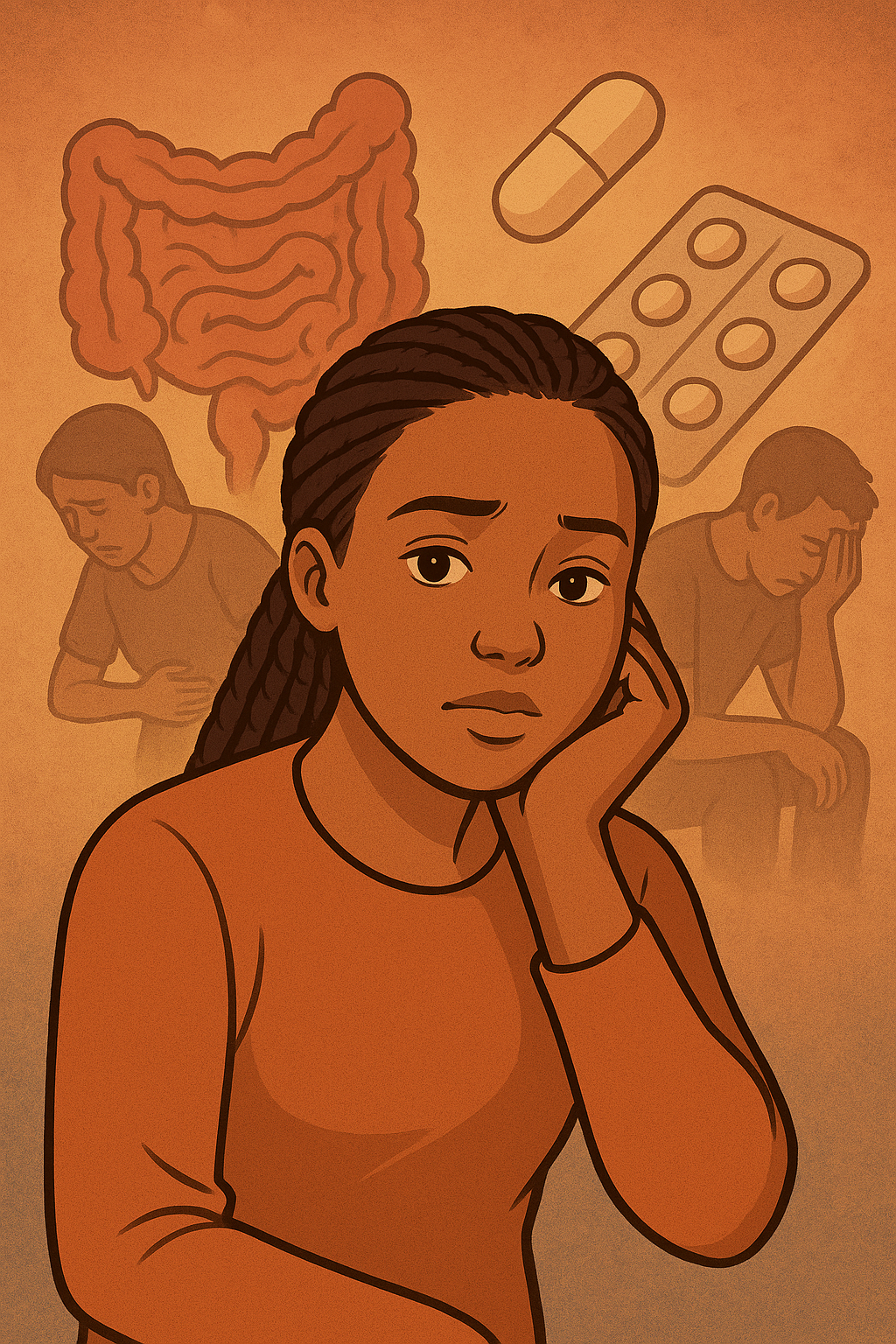
Lessons from My Gut
by Beamlak Alebel (Addis Ababa, Ethiopia)
Yes, I am unique —
my gut became my greatest teacher.
It whispered truths through pain and peace,
showing me the strength in stillness,
the courage in listening,
and the power in being mindful of my body and mind.
I learned to honor,
to protect my quiet spaces,
to find balance between struggle and strength,
between ambition and acceptance,
between the heart’s desires and the body’s needs.
Through pain, I discovered patience.
Through discomfort, I discovered resilience.
Through every challenge, I discovered myself.
Awareness became my guiding light —
a lens through which I saw not just my struggles,
but my strengths, my possibilities, my growth.
It taught me not to blame,
not to expect perfection,
but to understand, accept, and nature.
Now, I walk as an all-rounded soul,
shaped by scars,
strengthened by storms,
yet softened by compassion.
I have learned that life’s lessons are never small;
each one shapes us, molds us,
and pushes us to rise higher than we imagined.
In the CCYAN community, I have found reflection.
Here, voices rise together,
hearts open together,
stories weave together into one shared hope.
We are not alone in our journeys —
our struggles are witnessed, our victories celebrated,
our voices lifted to inspire one another.
My gut has taught me more than pain;
it has taught me presence,
purpose,
patience,
and peace.
It has taught me that even in moments of uncertainty,
even when life feels heavy,
we can remain mindful, balanced, and whole.
And through it all, I continue to grow —
an all-rounded human,
aware, strong, compassionate, and ever-learning.
Photo Credit to: Shutterstock
To See What Cannot Be Seen: Living with Chronic Pain and IBD
by Michelle Garber (California, U.S.A.)
When most people hear the word "remission," they imagine relief, a clean slate, and the end of suffering. For those of us living with Inflammatory Bowel Disease (IBD), remission is supposed to mean that we can finally be free of the pain that controlled our lives and simply breathe again. Unfortunately, for so many IBD patients, remission doesn't mean that the pain disappears. Rather, our pain changes form. Our pain becomes quieter, more private, and more invisible. It becomes the kind of pain that can exist in silence. The kind of pain that may not scream for help, yet it still whimpers day and night. The kind of pain that is easy to be overlooked while the rest of the world assumes you're fine.
Chronic pain is one of the most misunderstood aspects of IBD. It lingers long after flares fade, threading through your days in ways that are impossible to explain. It's invisible, yet constant. It's being in pain every single day, but learning to function anyway because you have no other choice. Chronic pain has become a part of my life—like a ringing in my ears that I've had to learn to ignore. I've learned to appear "fine" because visible pain tends to make others uncomfortable, and because I've discovered that admitting the truth often leads to dismissal. I have become so adept at masking my pain that I've become fluent in pretending. Pretending that I'm not silently calculating how much longer I can keep standing before the pain in my abdomen forces me to sit down. Pretending that the subtle grimace that escaped when I moved the wrong way was just a product of my "resting b*tch face." And pretending that "pain" is no longer in my vocabulary.
The pain of IBD patients also commonly goes unrecognized by medical professionals because the traditional 1-10 pain scale was not built for those living with chronic pain. For example, if I tell a doctor that my pain is at a "6/10," they may interpret that as "moderate discomfort." For those without IBD or chronic pain, though, my "6" might be their "10." Our baseline is simply so different from those without chronic illness/chronic pain, therefore making the standard 1-10 pain scale almost meaningless for us. This can have dangerous consequences as pain is typically the body's signal that something is wrong. When we are constantly experiencing pain, it can be difficult to determine whether it's "significant enough" to seek help or whether it's just our "new baseline." The fact of the matter is that any pain should be and is "significant enough," but we've been conditioned to not view it as such. We've been conditioned to accept a new and distorted "baseline level of pain" due to our illness, when those without chronic pain are not encouraged to do the same. Therefore, it can be hard for both us and medical professionals to know when something is "wrong," creating the potential for treatment delays, disease progression, prolonged suffering, and—depending on the illness—even fatal consequences.
Living with chronic pain often means learning to downplay your pain. No matter how much pain I'm in, I never rate my pain as a "10." I rarely even rate it as an "8" or a "9" because I know what happens when I do. I've seen "the look." It's that flicker of suspicion that crosses a medical provider's face when you say you're in severe pain, but you don't exactly "look" like it. I have felt the shift in tone when my honesty is mistaken for medication-seeking or when my tears are assumed to be those of ‘crocodiles.’ Because as it has been made quite clear by many medical professionals, if you don't have overwhelmingly visible evidence of your pain, then it must be exaggerated. Or, you must have a mental illness since "it's just anxiety," and "it's all in your head." So, like many others, I minimize my pain. I say that it's a "4" or "5." I'll tell doctors that my pain is manageable, even when it's often very much not.
The stigma of simply wanting relief is one of the cruelest aspects of IBD and chronic pain. The truth is, it's terrifying to need help in a system that might not believe you. IBD also presents unique challenges when it comes to pain management. Nonsteroidal anti-inflammatory drugs (NSAIDs) are usually off-limits because they can actually trigger flares. Opioids, while sometimes the only medications strong enough to even touch the pain, are approached with understandable caution due to their risks (i.e. the potential for constipation, dependency, and/or substance use disorder). As a result, we're often left to "cope." We're told to meditate, breathe, use heating pads so often that we burn ourselves, and/or use methods of distraction while our insides feel as though they're literally being twisted inside-out. If we're lucky, we might just get a pamphlet or a link to a video explaining these coping mechanisms. We're essentially almost abandoned by most medical providers as they expect us to endure significant pain without the use of effective pain relief options.
Don't get me wrong, these coping skills can help, but they certainly don't erase our pain. They just make it more bearable. Over time, the constant strain of pushing through the pain can wear down even the strongest person—the person who has "been through it all" and has a "high pain tolerance." Chronic pain doesn't just live in the body. Chronic pain infiltrates the mind and can chip away at one's patience, hope, and even will to keep fighting.
Yet, I understand why providers are cautious when it comes to pain management because I've seen the other side of it too. I currently work at a substance use disorder treatment center as a soon-to-be therapist. I've noticed that many clients' struggles with substances began in the same place: pain. Some struggled with physical pain, some with emotional pain, and many with both. Some clients even suffered from chronic illness(es)/injuries, were told that there was nothing that could be done for their pain, and were never provided with any sort of pain relief by their doctors. Others were prescribed opioids for a while and were then abruptly cut off from them by their medical providers. Much of their substance use history echoes the desperation that many IBD patients have also experienced—the desperation to simply function. The desperation to hold down a job and just get through the day. The desperation to be able to sleep through constant throbbing and aching. The desperation to escape one's pain for "just five minutes." The desperation to just be.
These stories serve as a reminder that pain affects so much more than what meets the eye. That's why it hurts so deeply when our pain is minimized by doctors, friends, family members, partners, and even by ourselves. We tell ourselves that our pain isn't as bad as it feels, while we're quietly counting the minutes until we can lie down. We tell others that we're "fine" because we don't want to be seen as "fragile" or "dramatic." We tell doctors lower numbers on the pain scale so that they'll take us seriously. Many of us would rather suffer quietly than risk being labeled. We learn to mask pain so well that even those closest to us never usually realize the strength it takes for us to just get out of bed.
Masking pain comes at a cost, though. Each time we minimize our pain, we invalidate our own experience. We erase a little bit of our own truth, piece by piece—a small but painful act of self-betrayal that we've been conditioned to commit in order to be believed. Masking pain also isolates us. It makes our struggle invisible, and in doing so, it allows others—including medical professionals—to not be able to see the undeniable pattern of IBD patients with chronic pain.
Pain is not just a symptom. It's a lived experience that profoundly shapes our relationships, our work, our self-worth, our future, and our sense of identity. For example, we might pursue occupations that don't require physical labor, and we might choose living environments that are close to our caregivers/doctors, have bathtubs over showers, and lack staircases. For those of us living with a chronic illness, pain becomes part of who we are—not because we want it to, but because it demands to be acknowledged.
Living with chronic pain and IBD means existing somewhere in a space between endurance and exhaustion. Between being believed and being dismissed. It means learning to hold compassion for yourself, even when the world doesn't. It means carrying an invisible burden that requires extraordinary strength to bear, even though it feels as though you have no strength left to do so. It means showing up—for others, for yourself, and for life itself—often without anyone realizing just how much effort it all takes.
That quiet persistence is something that I have come to admire deeply, both in myself and in others who live this reality. Because even when our pain is invisible, our resilience is not. It serves as a powerful testament to every person who keeps going despite their own body making the simplest things feel impossible. And even though our pain may be a part of who we are, our resiliency proves that it is certainly not all of who we are. We are so much more than our pain and our illness.
Still, our pain deserves to be acknowledged. Our stories deserve to be believed. Our healthcare system must learn to see what cannot be seen—not to just treat the illness, but to honor the full human experience of actually living with it.
Therefore, we need a better way to talk about chronic pain, especially in regards to IBD. We need providers to understand that our "normal" is not their "normal." That just because we appear to be "fine" does not mean that we are not suffering. That pain in remission is real. And that asking for pain relief isn't manipulation—it's survival.
Living with chronic pain and IBD means learning to navigate a world that often doubts what it can't see. But we exist, and our pain is valid. It's time for the system and the world to finally see us because if you look hard enough, you'll see that our pain is actually not as invisible as it seems—it just continues to go unseen.
Image by @gnikomedi on Unsplash.
Reflections on Curating the “Familial Patterns” Art Show
by Kaitlyn Niznik (New York, U.S.A.)
If you haven't already, you can watch a video tour of Kaitlyn’s “Familial Patterns: Generations of Patients” art show here!
Acknowledgements: My warmest thanks to Shelly Philips - my co-conspirator for the show, to Deborah Reid and Tracy Hayes who run Gallery RAG, CCYAN alum Selan Lee for helping me find my message, and to all the CCYAN members and chronically ill creatives who submitted work! This was my first time curating a show and I'm so thankful I had that opportunity!
Since the start of my CCYAN fellowship, I wanted to make an art show highlighting people's shared experiences with chronic illness. In July, I went to Gloucester with a goal and a promised gallery space – while I couldn't fully visualize the show until everything was up on the walls, and imagined so many variations of the themes, ultimately focusing the show on family connections to chronic illness made it much more personal.
Shelly and I spent the duration of the show gallery-sitting and having conversations with visitors about the show's theme. As we reflect back on our time at Gallery RAG, Shelly and I have some final thoughts we'd like to share:
The stigma associated with Crohn's, colitis, and other chronic conditions is something rarely seen, let alone talked about openly. Gallery RAG, which stands for Radical Acts of Generosity, was the perfect place for us to launch this exhibition and confront people's preconceived notions of illness. The show was just a drop in the bucket to spread awareness and promote acceptance. It allowed people to come together from isolated communities - even crossing oceans to create connections. One visitor reflected on her husband's chronic illness and his struggle to find motivation to get out of the house. She thought a creative outlet might help him feel seen and accepted. Others also shared stories with us, about different loved ones struggling with their health. Sometimes just showing up is half the battle, making a safe space to create, breaking the cycle of isolation, and talking about taboo topics that are usually swept under the rug. It felt good to normalize our medical issues and talk about them casually with visitors. We hope the gallery guests and livestream viewers were able to connect with the amazing variety of pieces in the show.
Looking into the future, Shelly wants to explore how to reverse the curse of chronic illness by lessening its impact on future generations. She hopes to look into how that in itself could break family cycles of trauma. Shelly wants her future work to shed light on the mothers who never knew that they had undiagnosed autoimmune or inflammatory disease. She plans on investigating how history repeats patterns in the things handed down - after mothers have already passed down the cellular dysfunction - and exploring what immune modulation, environmental changes, and the microbiomes change such patterns. During our conversation, Shelly also talked about Alexis Gomez’s poem about seeing her mom in a different light and how much that touched her. We hope to collaborate more in the future to share the patients’ perspective and focus on how art/writing can be a healing tool.
We loved how the poems and art in the exhibition worked together. Seeing all the different submissions from poetry, collage, zines, prints, paintings really showed there are so many expressive outlets to utilize. It felt larger than us and we are so grateful we had the opportunity to share your stories. We enjoyed the challenge of making the show accessible for everyone - whether international or on the other side of the country and we can't wait to see what our next chapters bring!
If you haven't already, you can watch the video tour of Kaitlyn’s “Familial Patterns: Generations of Patients” art show here. Below, you can also see some of the pieces submitted by CCYAN fellows and other community members!
Beamlak Alebel’s (CCYAN Fellow, Ethiopia) poem, “A Heart That Heals,” thanked all the doctors, nurses, surgeons, family, and friends for helping her on her journey to healing. Her heartfelt gratitude shined through to readers who shared their appreciation for their own support systems.
Aiswarya Asok’s (CCYAN Fellow, India) poem, “Mosaics.” tackled the grief and emotions attached to carrying her mother’s hidden pain. Aiswarya’s piece offered a glimmer of hope, in that through our endurance and shared suffering, we might find more answers and a better prognosis to bring about change.
Alexis Gomez’s (CCYAN Fellow, USA) poem, “Letter to Mom,” also reflected on her relationship with her mother and how similar yet different their medical journeys are from one another. Her writing felt like a sincere attempt to grapple with mixed emotions, her mother’s guilt, and their shared perseverance in the face of IBD.
Multiple works from artist Andreana Rosnik, including: “Recipes for a Flare,” a collage communicating the danger and inflammation that comfort foods might cost us internally, which took me back to my own fights with food. “Portrait of the Artist as a Colon,” a zine (a small art booklet) illustrating her challenges living with Ulcerative Colitis. As an artist who also draws colons, I appreciated Andreana’s refreshing take on a digestive system fraught with issues. Her “colon wyrm” and “biblically-accurate intestines” deserve a spotlight as well, and could easily be made into merch and tshirts for other folks with colon issues.
Nancy Hart’s acrylic painting, “COW,” (top right) depicted a pink cow silhouette on a black and white backdrop to represent one of her many inherited allergies. Marnie Blair’s print, “Snakes and Rivers,” (center) echoed ideas of transformation and survival on the surface of a blue disposable medical drape. The layers of meaning and the subtle ties to both the body and environment appealed to us as we were curating the show.
See the rest of the featured artwork from Kaitlyn and other CCYAN community members in the video tour!
The Hidden Struggle: Medication Access and Equality for IBD Patients
by Beamlak Alebel (Addis Ababa, Ethiopia)
Treatment is more than a diagnosis or a prescription — it’s about whether the medicine you need is available, affordable, and within reach. For many IBD patients, that uncertainty becomes a heavy burden. It’s hard to stay strong when your survival depends on something you might not find or afford tomorrow.
For me, the struggle is deeply personal. Every month, when it’s time to get my medication, I feel both guilt and sadness. I can’t ignore the heavy burden it places on my family. Watching my parents worry about how to afford my treatment hurts more than the illness itself, especially since the medicine is rarely available in public hospitals. Even though they never complain and always care for my feelings, I can see the stress in their eyes — the quiet fear of what might happen if one day the medicine becomes too expensive or unavailable. It’s painful to live knowing that your survival is also your family’s financial struggle. I wish the medicine could at least be less expensive and easily accessible everywhere, so no one would have to choose between health and hardship.
The world has powerful medicines with great potency — but what is the use of their strength if only a few can afford them? True progress in healthcare means making effective treatments available and affordable for everyone, not just for those who can pay the high price.
Access to medication is not a privilege; it is a lifeline. Yet in many places, that lifeline is fragile. I have seen patients lose hope — not because their illness defeated them, but because the system failed them. Seeing people treated as if their lives are less valuable simply because they are sick is one of the deepest pains a person can feel. It makes you question your worth. It makes you feel invisible.
But we are not invisible. We are fighters, dreamers, and survivors. Our illnesses may have changed our bodies, but they have not taken away our strength or our right to be seen, respected, and included.
Equality should not only exist in words or promises. It must exist in action — in how policies are written, in how medications are distributed, and in how people with chronic illnesses and disabilities are treated. I know how it feels to be looked at differently, to be judged for something beyond your control. What we have is an illness, not a choice.
Even in schools and health-related fields, there are times when lecturers or professionals do not fully understand what it means to live with a chronic condition. They see our physical state but not the strength it takes to show up, to keep learning, and to keep fighting. Being judged for taking sick leave or missing class because of health reasons can make a person lose hope. For now, we keep silent — but one day, we may speak as a volcano when the time comes. Because silence does not mean weakness; it means patience, and patience has power.
I dream of a world where no one loses hope because of a lack of medicine or misunderstanding — where being different is not a reason for exclusion, and where compassion leads policy and practice. Modern research is advancing, but true progress will come when every patient, everywhere, is valued equally — when access to care and empathy become rights, not struggles.
Advocacy is how we get there. By speaking up, sharing our stories, and reminding the world that every life matters, we turn our pain into purpose. Because in the end, access to medication and equality are not just medical or social issues — they are matters of dignity, compassion, and humanity.
Everything will change one day — the policies, the systems, and the hearts of people. Until then, we keep raising our voices, believing that our struggles today can open doors for those who come after us.
Fatigue and IBD
by Aiswarya Asokan (South India)
Check out Aiswarya’s presentation slides on fatigue & IBD! She shares about the prevalence of fatigue, types of fatigue, risk factors, the impact fatigue can have on IBD patients, and some suggestions for managing fatigue.
Life with Crohn’s: A Visible Person with an Invisible Disability
by Rifa Tusnia Mona (Dhaka, Bangladesh)
It’s already been a month since I moved to Lisbon. As an Asian girl setting foot in Europe for the first time, almost everything feels new — the culture, the streets, even the rhythm of everyday life. My university is about an hour away from my dormitory, and each morning I take the Carris — the public bus. It’s often crowded, especially during rush hour. On days when I’m carrying groceries, standing becomes a real struggle.
At the front of the Carris, there are four seats reserved for the elderly, pregnant women, parents with children, and people with disabilities. Every time I see those signs, I ask myself quietly:
Where do I fit in?
Am I “normal”?
Am I someone with a disability?
For a blind person or someone in a wheelchair, the condition is visible — their challenges are seen and, therefore, more understood. But for someone like me, living with Crohn’s disease, the weakness is invisible. Even carrying my laptop sometimes feels like lifting a boulder. On bad days, groceries are out of the question.
A few times, I’ve taken one of those reserved seats just to rest for a moment — and on more than one occasion, an older passenger scolded me in Portuguese. I didn’t have the words, or the energy, to explain.
To make things easier, I sometimes order my groceries online. But when the delivery person arrives and I ask them to carry the bags up the stairs, I often get that same puzzled, slightly judgmental look — as if I’m just being lazy.
The truth is, many people still don’t know what Crohn’s disease is. And when you’re in a new country with a language barrier, explaining your condition to every stranger sometimes isn’t possible.
One day, I was sharing this with a senior from my university. She listened and then said something that stuck with me:
“From the outside, you just look a bit tired and thin. A lot of people are like that. How would anyone know what you’re going through?”
And she was right. There’s no visible “signature” for people with invisible illnesses like IBD. No sign that quietly says, I’m struggling, even if you can’t see it.
That “signature” matters — not just for access to certain rights or support, but also for empathy. When people can recognize what you’re dealing with, even without words, life becomes just a little more humane.
I’ve been thinking: instead of only pushing for general awareness, maybe it’s time for a more practical step — some kind of universal identifier for invisible disabilities. It could be a color band, a card, a small badge — something that lets others know that, while we may look fine, we’re fighting battles they can’t see.
Because when life is already heavy with these hidden challenges, constantly having to explain yourself shouldn’t be another weight to carry.
Thank you for reading. See you next month.
Featured photo by Kyle Miller from Pexels.
Preparing for an International Trip: Chronic Illness Edition
by Lexi Hanson (Missouri, U.S.A.)
Everything I Did to Prepare for my Trip to Southeast Asia (Chronically Ill Edition):
I made sure I had a plan for hydrating and receiving my water intake. Tap water in the parts of Asia I was traveling was not safe to drink. I also needed a liquid to take my medications daily. 7-11 and other nearby stores had many options and I made sure to always have a bottle with me.
I requested vacation override with my health insurance company to ensure I had enough medications for my trip (and then some). If you’re taking medications, I’m sure you understand the daily/weekly/monthly struggle with pharmacies and/or insurance companies to fill your prescriptions, so make sure to get a head start on this one!
I educated myself on street food safety and what I needed to do to stay healthy, while also experiencing the culture! I did not accept any fruits that were unpeeled or could be washed with tap/unclean water. I was careful about meat at street food markets, and spoke with my tour guide about how to identify whether food was sitting out for long periods of time and deemed not fresh.
Tip: Make sure you’re familiar with the vaccines that are necessary and highly suggested in the area(s) you are traveling. Most importantly, check with your doctor about if any of your medications make it unsafe to receive a live vaccine.
The Day I Chose to Fight: Surgery, Strength, and the Power of the Mind
by Beamlak Alebel (Addis Ababa, Ethiopia)
There are days that change us forever — not because we are not ready, but because life gives us no choice. For me, it was the day I faced surgery.
That moment came with fear, complications, and a sense of losing control over my body and even my appearance. I wasn’t prepared — not mentally, not emotionally. Yet I had to choose: risk everything or let everything fall apart.
Before that day, I never imagined hearing the words: “You may be moved to the ICU.” No one is ready for those words. Your heart races, your mind fills with unfinished dreams, and suddenly life and death sit together in the same breath.
But when that moment came, I made my choice. I chose life. Even with all the unknowns. Even with the pain. Because sometimes the bravest step you’ll ever take is the most uncertain one.
Over time, I learned that strength isn’t about muscles or energy — it’s about mindset. When your body feels defeated,your mind becomes your strongest weapon. Deep inside me, beneath all the fear, I found a hidden strength I never knew I had.
Yes, I cried. Yes, I doubted. But I rose.
Living with IBD has stolen parts of my childhood, but it has also taught me to fight. My strength didn’t appear overnight — it grew through countless painful moments that shaped me into the woman I am today.
And here’s the truth I want others to know: we don’t need approval from anyone to define us. We know our own limits, and we know our own strength. Scars don’t make us less — they prove we survived.
If you’re standing at the edge of fear right now, please remember: you are not alone. The fear is real, but so is your courage. Even when your body is tired, even when others don’t understand — your mind can carry you further than you think.
We are not broken.
We are not our scars.
Photo from @vicky49 on Unsplash.
Mental Health & IBD Series
by the 2025 CCYAN Fellows
This month, some of our fellows worked together to share perspectives on mental health and IBD. Check out their articles and videos on this topic below!
Insights from Beamlak (Ethiopia), Aiswarya (India), and Lexi (U.S.A.)
Living with inflammatory bowel disease (IBD) is never just about physical symptoms. It impacts mental health, education, relationships, and self-worth. For many patients, the emotional toll can be as heavy as the physical pain. We came together to explore the connection between IBD and mental health, and each of us shares a different perspective, facts, lived experiences, and personal reflections. Together, they form one message: mental health in IBD care is not optional, it is essential. We wanted to show that IBD is both a physical and mental health journey. Data highlights the need for better systems of care, and personal stories remind us of the resilience and strength it takes to keep moving forward. Together, we call for greater awareness, compassion, and support for every person living with IBD.
Read their perspectives:
Facts we Can’t Ignore - Lexi
Diagnosis is a Light, not a Lampshade - Aiswarya
“Let it” - My Rule for Living with IBD - Beamlak
Insights from Akhil (India) & Alexis (U.S.A.)
Akhil & Alexis (alongside 2022 CCYAN Fellow Maalvika & CCYAN’s Program Manager Rosa) presented about the intersections of Chronic Illness, Mental Health, and Cultural Considerations at the 2025 Bridging Voices, Building Futures: Youth Innovation in Mental Health Conference (hosted by Generation Mental Health). View the presentation below:
Check out more of our 2025 fellow’s articles and videos on other mental health topics:
What it’s Like Working Through Phobias - Kaitlyn Niznik
Through (on Stigma, Shame, and Talking about IBD) - Michelle Garber
God of Small Things: A Crohn’s View (on Stigma and Connection) - Rifa Tusnia Mona
IBD & Grief by Akhil Shridhar
Internalized Stigma in IBD, Mental Health, and Quality of Life by Aiswarya Asokan
Mental Health & IBD (An Infographic) by Lexi Hanson
The Facts We Can’t Ignore (Mental Health & IBD Series)
by Lexi Hanson (Missouri, U.S.A.)
According to the American Gastroenterological Association (AGA), 35–36% of IBD patients report anxiety or depression—far above national averages. Yet, too often, providers prioritize physical health while overlooking mental health needs. Supporting mental health is not a luxury for IBD patients—it is a necessity.
What are some supports that can make a difference for Young Adult IBD patients?
Embedding mental health professionals (psychologists, social workers) in IBD care teams.
Routine mental health screening for young adults.
Coping toolkits to build self-advocacy, communication skills, and emotional resilience.
Extending transition support to age 25, not just 18–20.
Availability of peer and lived-experience communities for validation and advice.
Access to reliable information tools about nutrition, travel, accommodations, relationships, fatigue, and brain fog.
IBD-aware university services: bathroom access, class accommodations, and counseling.
Policy reforms to ease insurance challenges and improve navigation.
Education on ADA rights and workplace accommodations.
Self-compassion training to protect mental health.
Check out Lexi’s July post for more facts about Mental Health & IBD!
Photo from Unsplash.