NEWS
Little Wins: Things that Keep you Going
This article is by Nandani Bhanot from India.
To be very honest, a little over a year ago, I had little to no idea about the presence of chronic illness patient-led advocacy efforts around the world. It is a real pity because as I look back, it would have helped me navigate many of my IBD experiences better. I would have been armed with more information to vouch for my safety, comfort and rights. However, I am glad I started now rather than later, and I look at the many things I have learned thanks to the Crohn’s and Colitis Young Adults Network (CCYAN) with great satisfaction. Yet, patient-led advocacy is harder than it seems, especially in the South Asian context.
When I was first diagnosed with IBD, I was at a stage in my life where taking up space felt complicated and wrong. So at moments where my illness conflicted with social plans, I would push my needs away rather violently in favor of not making other people uncomfortable or having to explain my uncertain situation. Sometimes, when I ignored my needs too often, I would bitterly burst open – they were highly volatile moments of trying to advocate with very little information. It was akin to a baby taking its first steps and learning how to walk on shaky ground. The feedback during these first years was overwhelmingly negative, with people underestimating the severity of my illness, disbelieving my experiences and ignoring my needs. I admit, the advocacy was ungraceful and thus perhaps, I received unfavorable feedback. Cut to now, I am still learning how to best advocate for myself, people with IBD, and the larger chronic illness community. Now, I’m starting to receive positive feedback.
Being vulnerable requires immense courage in the South Asian community. The society thrives on critiquing and scrutinizing everything that is a part of it, and with very rigid definitions of what success is and what the many shortcomings are, to put yourself right in the middle of it all is a courageous task. I started actively and unabashedly talking about my illness only after I joined CCYAN this past year. I did not expect to impact the social circles around me, even though part of my goal was to reach out to someone like me in the past and help with information and support. Unfortunately, every time I posted something, I was simultaneously fighting internalized shame from the vulnerability of allowing it to be shared. The society can make you feel like you are exaggerating your experiences, asking for attention, and can even make you question your own reality. Fighting your immune system, the ableist world system, people’s misunderstanding of your disability and your own thoughts can be exhausting and can make one feel demotivated easily and frequently. With basic rights not covered for the majority of the Indian population, raising awareness for invisible disabilities can seem completely pointless rather quickly, and like your efforts aren’t making a difference. But this is not true.
Ever since I embraced advocacy wholeheartedly, multiple people have approached me to say their thanks in helping them understand the chronically ill in their personal circles, or in helping them understand their own symptoms. Connections have been made where otherwise we would have remained strangers, and strong support systems have been established where before, people may have felt extremely alone in their struggles. And while there is no lack of unsolicited opinions and unhelpful feedback, the weight of the positive interactions is not to be underestimated. They make the whole thing worth it. Even if the posts impact one person positively, especially in knowing they are not alone, it can make a world of a difference. For instance, think back to when you felt alone with a certain aspect of your illness/significant life event. Coming across something that resonated with the most vulnerable part of you must have had an extreme impact. In my case, when an adult had opened up about navigating a life with ulcerative colitis, it changed my life. I’d previously thought that being diagnosed with IBD meant my life had basically ended. With all the restrictions and future health risks, this person showed me life could go on, just differently than we imagined. So in these moments, when I realize someone is actually impacted by what I’ve posted, that is what keeps me going.
Starting a New Treatment: My Experience with Humira and Stelara
This article is by Jennifer Lee from the United States.
Here’s a picture of me before my treatment! A bit nervous, but hanging in there.
This past week, I received my very first dose of Stelara, my latest biologics treatment, at Mount Sinai in New York City! Unfortunately, even after a year on Humira subcutaneous injections, my Crohn’s symptoms have not subsided as we had originally hoped. After having seton drain placement done back in December 2020, along with another operation in June 2021, my healthcare team at Mount Sinai’s IBD Center decided that it may be best to try a new method of attack with a new set of biologics treatment.
Before starting the treatment, I had multiple healthcare workers stop by my room to explain what exactly Stelara was. I’m grateful that my mom was there to be by my side during this transition, but I also know what a blessing this is. When I was first diagnosed back in June 2020, I was completely alone in the hospital while COVID-19 infection and hospitalization rates were through the roof. The simple comfort of being surrounded by a loved one went a long way.
Here’s me while receiving my first dose of Stelara intravenously! The next dose will be done via injection, hopefully on my college campus.
While I originally had a bit of trouble breathing in the first few minutes, my nurses assured me that this was not an allergic reaction to Stelara and that I was reacting well to the medication. It only took about an hour for the entire round of Stelara to be infused, but I did wait an additional 30 minutes to ensure that I would not experience any additional side effects. Truth be told, I was surprised at how efficient and fast-paced the entire infusion center at Mount Sinai was; I felt completely safe and well taken care of in their midst. Shoutout to the tireless effort of the amazing healthcare workers at Mount Sinai!
The day immediately after my first dosage of Stelara, my chronic fatigue kicked in, leaving me completely knocked out the morning after. Even after a year of living with Crohn’s disease, I’m still surprised by the ways that chronic fatigue manifests in my life. Although self-care admittedly goes a long way in understanding my body’s signals, I was most definitely caught off guard by how exhausted I was after the first dosage.
Moving forward, it’s a bit terrifying knowing that my treatment plan may or may not work. However, I feel so grateful to have access to doctors that specialize in IBD care and surgery; all IBD patients deserve access to the most effective treatments for their specific condition. My first dose of Stelara was a reminder of not only how fortunate I was to have a second chance at a biologics treatment, but also of how much more work needs to be done to ensure that healthcare becomes equitable for all.
Tips to Improve Your Quality of Life with a Stoma
This article is by Saravanan Nagappan from Malaysia.
Photo by George Becker from Pexels
Many of my ostomy friends confided that their life has changed since they became an ostomate. They feel their quality of life has deteriorated after having a stoma. They are unable to enjoy their life as before they became an ostomate. They mention changes to their diet, workout, and their social activities not remaining the same as before. Yes, I have to agree with them, because what they say is a common fact for an ostomate to experience and I personally faced the same issue as well even a decade being an ostomate, still my life is not the same as before. I’m going to share with you a few tips on how I have managed to reduce the impact a stoma has on quality of life based on my experiences.
Accepting your new life as an ostomate
The first tip is acceptance. We need to accept that we are ostomates and prepare for it both mentally and physically. At the end of 2011, my surgeon approached me and suggested that I have to go for Ostomy surgery as it was the best way to heal my fistula. My surgeon informed me regarding the complications I would be facing. At that time, I was confused and worried. I took a few days to decide whether I want to do it or not. The decisions involved many considerations, especially the changes in my life that come from being an ostomate and living my entire life as one afterward. After a long discussion with my family, I finally agreed to go for the surgery. I psyched myself up mentally by listing the benefits of this surgery and the changes it would bring to my life especially the physical ones. Since I accepted my situation and geared up for it, post-surgery changes were not monumental. My goal at that point in my life was to heal my fistula and get my Crohn’s under control. It was more than enough for me.
Adapting to new norms
The next piece of advice is adapting to new norms. This is important for an ostomate because a new ostomate is like a newborn. We are reborn into a new physical self and the changes it brings to our routine are something we have to relearn all over again. Without a choice, we have to adjust to new norms. Common new norms are our diet, daily routine, and social activities. It’s impossible to change everything overnight, but focus on small changes in our daily life and we will be able to see the impact in the long term. Once we learn how to slowly accept and adapt to our new norms, we will find it easier to live our life as an ostomate. The problem occurs when we refuse to accept new changes or routines. Inability to accept the changes can lead to deterioration of life quality.
Pre-planning your days
The following tip is to pre-plan. Pre-planning everything you want to do is one of the ways to improve an ostomate’s quality of life. Pre-planning a daily routine or outing is common in anyone’s life. However, it could be an essential habit for an ostomate. For example, assume that you need to attend an event in a few days’ time. In order to attend this event, you need to pre-plan your diet so you can avoid any food that can cause gases. By doing this you may avoid visiting the washroom all the time in front of others and enjoy the event more. Not only diet, but you can also pre-plan for other matters such as your physical and emotional wellbeing as well. Remember pre-planning can help to prevent any last-minute mishaps or emergency withdrawal from a situation.
Physical exercise for a better quality of life
As a final tip, I personally suggest that ostomates perform some physical exercises. After my surgery, I thought that my workout routine had come to an end. However, my thoughts had changed after I met a few senior ostomates. They advised me to not abandon my workout and they guided and motivated me on how ostomates should do their workouts. I started again with basic workout routines and challenged myself to go for the harder level. So how do workouts improve our quality of life? Doing physical exercises help to build our body muscles, reduce unwanted fats, keep our body fit and flexible and also improve our blood circulation and digestive systems. Moreover, workouts help to remove toxins from our bodies. which will keep our bodies healthier. Exercises also help to keep our minds active and create more positive energy within us. All these could tremendously improve ostomates’ quality of life.
In a nutshell, ostomy surgery is a life-saving procedure for many patients. Therefore, it should not be treated as a burden. Rather, we must take our own individualized care and explore new choices to improve the quality of life after ostomy surgery. I hope these tips can help you in your ostomy journey.
Let’s control our quality of life, it is in our hands!
"But You Don't Look Sick" - A Photo Journal
By Vasiliki-Rafaela Vakouftsi from Greece.
“But you don’t look sick”. How many times I have heard this? Maybe I don’t look sick to you but I am sick and my daily life is far from what you may think.
I tried to captures in pictures my daily routine as a chronic patient and I’m going to share them with you.
First of all, let me tell you some things about me. My name is Vasiliki-Rafaela, I’m a musician and I have Crohn’s Disease, Adrenal Insufficiency, Psoriasis and Psoriatic Arthritis. I have written a book about my journey with Crohn’s and a book about my life with Adrenal Insufficiency. Also, I really like traveling and I really miss it with the pandemic.
Now let’s start with the hospital visits…
...the hospital stays and therapies…
...the hospital stays and therapies…
...take the pills, medicines and supplements…
...and maybe today is the day of the week for the injection for Crohn’s…
...or maybe I need the emergency shot for Adrenal Insufficiency…
And now it’s time for a walk.. Don’t forget to carry the pills with me...
...and of course my medical ID…
Back at home again.. Really exhausted...Let’s check the e-mails and read a book before going to sleep
That’s a little idea of how my daily life is. But, you’re right. So before saying “You don’t look sick” think of what is behind the image and what you cannot see…
What I Eat in a Day
TW: mention of eating disorders & disordered eating
I really didn’t want to write this article. I am pretty open about how I have a lot of dietary restrictions. When I go out to eat with friends, I usually tell them that I follow a strict diet for my Crohn’s Disease. Then they’ll ask if I can have anything on the menu, and I will say No. The inevitable next question is always: So, what can you eat? I’ll list off a few foods like oats, bananas, blueberries, broccoli, chicken, and buckwheat, and that's usually the end of that conversation. I’ve had it so many times; honestly pretty much any time I meet somebody new.
I tend to think that when I give people that list that they just assume I stop listing things because it would get excessive if I named every food I could eat. I imagine that they might think I am going through a typical day, and maybe other days look different than the short food record I have given. I don’t think that anybody really considers what it feels like to eat the same 5-10 foods over and over and over and over again. But I do. I do because that has been my life since January of 2019 when I entered “remission”.
Remission for me has always been rocky. I noticed really quickly that while I felt better overall (you know, my body wasn’t trying to set records for lowest hemoglobin and highest CRP simultaneously), I still had some symptoms. I decided to take the advice I give a lot of my IBD patients these days and start a food journal to try to find my trigger foods. Slowly I started feeling better as I cut back on the foods that I noticed were giving me hives, acne, bowel cramps, diarrhea, and a whole host of other symptoms.
So I got to a baseline diet with some foods I knew I felt good on and did that for a bit. It was wonderful, as long as I ate these foods, I felt pretty much “normal” and could do all the activities I wanted. But I wanted to find more things I could eat, so I started to do food reintroduction. I would try a new food for one meal and see how I felt afterwards. If I felt worse, I knew that food wasn’t a good fit and I’d mark it as a trigger food.
Fast forward to 2+ years of trying a new food every weekend and you’d expect my diet to be all normal and varied with only a few restrictions. Haha I wish. I’m pretty sure after all this time it has gotten worse. I guess the problem really is that my body thinks pretty much everything other humans call edible is unfit for consumption, and it lets me know that loud and clear.
That all is the much needed background to my current diet. I guess I should share what it looks like at some point as that is the main reason I wrote this article, so here goes:
Breakfast
3 cups of cooked rolled oats with ½ sliced banana and ½ cup blueberries.
1 Orgain Nutritional Shake
Snack
1 Orgain Nutritional Shake
Lunch
2 cups of cooked buckwheat, ½ sliced banana, and ½ cup blueberries
1 Orgain Nutritional Shake
Dinner
2 cups of cooked buckwheat, 1 ½ cups cooked broccoli, ½ a cooked chicken breast.
So…..yeah. I’ve pretty much been eating that or some slight variation (I used to eat a lot of plantains too) day in and day out for a few years now. Pretty messed up right? I am pretty sure from the outside this looks like at least disordered eating if not a full blown eating disorder. But, like, what am I supposed to do? It's not like I am not trying to expand my diet, I just can’t without Crohn's kicking my butt. Also I promise I’ve told every GI doc I’ve had about this and unfortunately there hasn’t been anything they have been able to do to help.
I decided to write this article because during the few years I’ve had these issues with all these trigger foods I’ve never really found anything online that mirrors what has happened to me. My hope is that if there are more people with IBD out there who struggle with these food issues as much as I do, that you at least feel validated that you aren’t the only one going through this. It sucks, and maybe one day we will have an answer as to why it happens.
Until then, if you are having issues with foods triggering your disease, bring it up to your doctor or dietitian. Spread the word. Even if, like in my case, the doctors or dietitian isn’t able to fix the problem, at least we are fostering awareness and discussions that will bring about solutions in the future.
Digestive Disease Week: Impact of COVID-19 on GI Patients and Practices
The Impact of COVID-19 on GI Patients and Practices was an eye opening session that shed light on the effects the coronavirus has on GI patients. Adam VanDeusen shared his study covering how crucial colonoscopies and endoscopies are in the management and diagnosis of inflammatory bowel disease, among many other illnesses and cancers, an area that is being profoundly affected by the COVID-19 pandemic. Timely diagnostic and management procedures, such as colonoscopies, are critical to ensure that patients receive the treatment they deserve in a quick and timely manner, whether that be an IBD diagnosis, management of IBD including a switch in medication, screening for anemonas and colorectal cancer. I’m sure many of you reading this with inflammatory bowel disease or other digestive diseases can relate to how the pandemic has hindered your healthcare and treatment. This reiterates why studying how to decrease backlogs and improve patient care in a critical part of every digestive illness, including colonoscopies and endoscopies, are so important.
VanDeusen discussed the reality of COVID-19 and its detrimental effect on colonoscopies needed for patients. The COVID-19 pandemic has caused a high number of cancelled or deferred endoscopies and colonoscopies since March 2020 due to health system policies, staff and facility re-deployment, and distancing measures. For my fellow IBD readers, I’m sure this doesn’t come as a surprise to you. Across the world, many colonoscopies and endoscopies were delayed or cancelled, causing stress, chaotic management of treatment, and prolonged diagnoses. In addition to IBD, colonoscopies to detect colorectal cancer, a type of cancer that can be prevented and treated when undergoing timely diagnostic colonoscopies, have been backlogged and delayed. VanDeusen dives into simulation predictors that forecast solutions to reduce the backlog and wait times patients are experiencing to ensure diagnostic treatments via colonoscopies and endoscopies are available for patients. As an alternative to colonoscopies, many gastroenterologists have been using a high-sensitivity stool-based test (FIT) as a way to detect colorectal cancer to prolong screening wait time from five to seven years if the results come back negative.
Benefits of high-sensitivity stool-based testing:
Alternative to colonoscopies to detect colorectal cancer
Lessens wait times
Extend time between colonoscopy screening
The three strategies in the simulation are Overtime, Exchange, and Extend. Through Exchange, GI clinics utilized the stool-based tests as an alternative to colonoscopies for patients that were referred strictly for colorectal cancer screening. Stool-based testing resulted in reducing the wait times for patients undergoing colonoscopy screening referrals as well as allowing quicker wait times for patients with no alternative diagnostic treatments. The second strategy, Extend, extended screening colonoscopies for patients with 1-2 adenomas on previous colonoscopy exams from five to seven years. Lastly, the Overtime strategy added one weekend endoscopy day to result in quickly seeing more patients for endoscopies and colonoscopies.
VanDeusen highlights that the study aimed to quantify the impact of evidence-based strategies to improve endoscopy access during the COVID-19 pandemic. The method created a model of a single endoscopy unit with an integrated healthcare system using a discrete event simulation in C++. The model began in March 2020 for 150 weeks and each simulation was replicated 100 times to ensure accuracy. To simplify the model used, when a patient arrives to book a colonoscopy and that patient is unable to secure a scheduled appointment, that patient is then put into the queue. This study looked at four different simulations to provide the best approaches for GI clinics to achieve the lowest wait time, Extend, Exchange, Overtime, and a combination.
VanDeusen explains that the study shows that triaging patients effectively will result in performing more diagnostic and high-risk surveillance procedures in a timely fashion. Without offloading strategies, prolonged queues and wait times develop, especially for screening colonoscopies. The Overtime strategy of one weekend endoscopy day increased colonoscopy volume and had the greatest impact on the number of screening procedures completed. The Exchange strategy reduced overall wait times more than Extend and Overtime. Combining strategies is the most effective solution, especially given the fact that doctors and healthcare staff have been continuously overworked during the pandemic.
Takeaways:
Effective triage will reduce colonoscopy backlog and queues
Doctors working overtime is the single best strategy to reduce colonoscopy wait times
Combining strategies will best reduce colonoscopy wait times and allow more patients to be seen in a timely fashion
This study was extremely important and was desperately needed to provide a solution to reduce wait times experienced in gastroenterology clinics across the world. The importance of this study is paramount and must be recognized and implemented by GI clinics and doctors to reduce wait times and improve treatment for patients for not only colorectal screening and diagnosis, but also for all patients with digestive diseases, including IBD. For those patients whose treatment has been affected by the pandemic, including me, this provides great hope and comfort that medical treatment can return back to normal and can withstand future uncertainties.
Growing Pains: IBD Lessons Learned from the COVID-19 Pandemic
In March 2020, the COVID-19 pandemic turned the world upside-down as we knew it -- that, in and of itself, is already the understatement of the year. Disability activist Alice Wong spoke of how the nation’s need for ventilators in hospitals directly conflicted with her needs as a disabled patient; Tiffany Yu, founder of Diversability, used her platform to raise awareness of transparent masks for easy lipreading access. Already, at-risk patients suffered from a lack of attention and space, only for this to be exacerbated by a public health crisis.
However, the pandemic also offered a chance for those with disabilities, and specifically IBD, to rethink our routines and lives. For example, in my own experience with Crohn’s disease, I’ve found that staying at home during the school semester had me re-thinking all my prior decisions in my relationship with food. It was, in fact, possible to regulate my diet and work in my medications without compromising my education -- the flexibility of virtual classes in university had opened up a new way of life for myself, one where I could sneak off to the bathroom during lecture without worrying about missing key points or bumping into desks.
Living with Crohn’s, it often feels as though my time is not my own. This phenomenon of constantly running on other people’s schedules is not exactly unique to Crohn’s or IBD as a whole -- in fact, it refers to a concept known as ‘crip time,’ in which society and its timetables ought to bend to meet the needs of disabled bodies and minds. It’s a community-inspired term that essentially encourages us all to work on our own time, taking up space as necessary to meet our individual body and mind’s requisites.
Whether it’s knowing where the nearest bathroom is, or having accommodations to turn the Zoom camera off, accessibility is an essential cornerstone of working with IBD. As a college student, I’ve found that communication with professors and administrators has become easier in a virtual setting, allowing for flexible office hours and minimal commute to buildings. In all workplaces, key lessons should be taken and continuously applied from the pandemic, particularly in regards to accessibility for disabled folks.
With this being said, a major caveat is that we as a society are almost always ‘plugged in’ or online -- being available on Zoom has made it near impossible to draw the (much-needed) line between home and the office, allowing professionals to work around the clock. As the world shifts back to a new state of burgeoning normalcy, may we all remember the importance of accommodating disabled folks in the workplace, in-person and virtually.
For those with IBD or any chronic illness, it is of the utmost importance that we too learn where to place boundaries in our work lives, prioritizing our physical and mental health above all.
Diversity in IBD: Being Disabled and Asian American
Almost exactly one year ago, I was diagnosed with Crohn’s disease after a grueling few months of trial-and-error diagnoses by my medical team. Truth be told, the news was a shock to my family, but not for the reasons you may first think of.
In my mother tongue, there is no widely accepted translation for “Crohn’s disease,” not to mention “Inflammatory Bowel Disease.” In a way, my Asian American identity is one reason why it took so long for me to receive my diagnosis of Crohn’s disease in the first place; my gastroenterologist had not previously thought to test for a condition that was thought to be more common in Caucasians or Ashkenazi Jews. Even amidst official resources from various foundations, it is admittedly difficult to find Asian representation within the IBD community.
As a disabled Korean American woman, I experience IBD through the lens of multiple marginalized identities. At the intersection of ability, ethnicity, and gender lies an incredibly complex set of conversations that society has yet to fully parse out and create space for.
While chronically ill and disabled folks found themselves facing a morphing status quo that was being overturned by a worldwide pandemic, their fight for accessibility and accommodations was simultaneously accompanied by embroiled racial justice initiatives. The Health Advocacy Summit has written extensively on how racism is a public health crisis, underscoring the need to include all marginalized communities in our activism efforts.
Personally speaking, I came face-to-face with the inevitable intersectionality of advocacy in the fight against anti-Asian hate. In the wake of 2020, the United States began to witness an alarming surge in anti-Asian racism that quickly escalated to violence and hate crimes. As a chronically ill patient, I knew exactly how it felt for an entire community to be marginalized, vulnerable, and at-risk, making it all the more urgent for me and my fellow student leaders to speak up against these acts of hate.
The intersectionality of these two identities is rarely discussed, yet they both mold and inform the other. My diet, my language, and my roots are so intimately tied to my Korean heritage, and in turn, my Asian American identity shapes the way I understand my chronic illness. As Sandy Ho wrote in Alice Wong’s Disability Visibility, “taking up space as a disabled person is always revolutionary,” but especially in the ways in which traditional East Asian attitudes often conflict with the mindset of the evolving American immigrant.
The same goes for the ways in which Asian culture influences food options for those with IBD. Nandani Bhanot, another 2021 CCYAN Fellow, wrote about how IBD diets and treatments are rarely created with people of color (POC) in mind, alluding to the lack of content on modified diets with traditionally Asian dishes.
Moving forward, I believe that my journey with Crohn’s disease and Asian American advocacy are not unrelated, but in fact, closely tied. Perhaps the best next step our IBD community can take is to create space for disabled POC, uplifting their stories and amplifying their voices.
Digestive Disease Week: Empowered Crohn’s Disease Care
I would like to thank CCYAN for providing me this opportunity to patriciate in Digestive Disease Week (DDW) 2021. One of the sessions that I attended is “Empowered Crohn’sDisease Care: Targets, Tools and Talking Patients”. From this session, I have learned about the use of treat-to-target approach to treat Crohn’s Disease (CD), the tools that may help risk stratify patients with CD, and about the personalized approach to CD care. The session was split into three presentations, which were presented by Dr. Parambir S Durai, Dr. David T. Rubin and Dr. Corey A. Siegel respectively.
1) Treating to Target: Aiming for Endoscopic and Symptomatic Remission
By Dr. Parambir S Durai
What is the study about?
Dr. Durai presented about the use and benefits of a treat-to-target strategy in CD aimed at deep remission.
Presentation summary:
We need to understand how this treat-to-target approach work. Treat-to-target approach which is also known as a tight control strategy is used to achieve sustained disease control. Target and risk will be set during this time, assessment and continued monitoring have to be done to ensure targeted outcome has been reached. The most important goal in this treat-to-target approach is to achieve endoscopic healing, normalized quality of life and absence of disability.
The different studies mentioned in the presentation aimed to give CD patients early therapy using a treat-to-target approach. Treat-to-Target approach will be able to prevent adverse long-term outcomes. The studies suggest that the non-conventional methodsused at early treatment stage or frequently brings out positive outcomes to patients’remission.
Treat-to-target is treating CD patients until they achieve the desired target for the CD patients like us is healing. Healing can be mucosal healing where we go for endoscopy and the colon looks normal with no inflammation or ulceration. In some cases, there might even be histology healing which means when biopsy has done towards the colon or small bowel there is no inflammatory cells seen. In the case of a patient has fistula, then the target is to have closure of fistula. To achieve this target, the patient needs to be put under full remission.
According to Dr. Durai, patients whose response to the treatment by improvement in biomarkers results shown reduction in CRP and calprotectin. They may go for symptomatic remission. The next target is to achieve deep remission by continuing assessment and monitoring. At this stage, if the response is good, patient will be able to experience the huge improvement in symptoms, better quality of life, decreased in hospitalization and finally free from surgeries and disability and any serious disease- related complications.
Although the opportunities are huge and will provide patients with better quality of life or even achieving the absence of disability, there are some challenges that still exist in this approach. The first challenge is that treat-to-target is a time and commitment needed to follow through this approach as it needs more follow ups and more complexity of individualized process with the already busy clinical team. The other barrier is lack of knowledge of what might happen to patients later. Both patients and clinical team need to understand the limitation and provide active disease control to the patients.
2) Clinical Decision Tools: Assessing Risk and Taking Action
By Dr. Corey A. Siegel
What is the study about?
In his presentation, Dr. Siegel briefed about the importance of clinical decision support tools and suggested using clinical decision support tools to risk stratify patients for individualized CD care.
Presentation summary:
What are clinical decision tools? Dr. Corey explains that the decision-making tools are guidelines for medical providers to follow through different process based on different parameters. The tools can help to enhance medical decisions with provided clinical knowledge, patients information and other related information. And from the data gathered, doctors can formulating a diagnosis, assessing patients level of risk and help practitioner to improve the way they make decision to select medication for their patients from result shown from the tools.
Practitioner can apply several types of clinical decision support tools which has been developed such as AGA Clinical Decision Tool, IBD CDST, or CDPATH.
What can we learn from this presentation?
This tools help practitioner to decide right medication for patients based on the balance of risks and benefits especially at the early stage or before they develop complications.
By using these tools, it may help to reduce practitioners from making any risk of misdiagnoses and medication errors.
The tools improve efficiency and patients’ satisfaction.
. Give more confidence to practitioners to recommending right therapy and apply more aggressive monitoring technics.
3) Shared Decision Making in CD: The Path to Improving Quality of Life
By Dr. David T. Rubin
What is the study about?
Dr. Rubin discussed about the complexity of shared decision making for patient-centered and empowered CD care.
Presentation summary:
Dr. Rubin informed that the shared decision making involves three different parties. They are: -
1. Patient
- Person who suffer with IBD and request treatments.
2. Doctors/ IBD Nurses
- Medical provider who have fundamental knowledge about the disease and therapies which can be used to treat IBD.
3. Payor
- Person/company/agency who pays for the care and treatments for the patient.
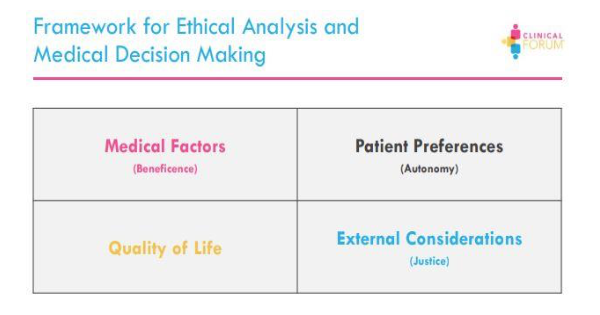
To make the relationship between the three parties happen there are several factors that should take to consideration by all the parties. Refer to diagram below:-
He further explains that, for each patient, the provider and payor must consider four variables: efficacy, safety, convenience and access. These variables help to makeprogress and provide better care for the patients. Practitioners can use “Ethical Analysisand Medical Decision Making” framework to make difficult medical decision. This can help to strengthen the doctor-patient relationship.
a. Medical Factor (Beneficence)
- This is a value in which the provider takes actions or recommends courses thatare in the patient’s best interest. The principle is based upon the objective assessment of a doctor, and what they feel is best for their patient. The points of concerns are:-
What is the patient’s medical problem? diagnosis? prognosis?
What are the treatment goals?
What are the therapies recommended?
What are the risk factors of the recommended therapies as well as the disease itself?
How are patients benefited by medical and nursing care?
How can harm be avoided?
b. Patient Preferences (Autonomy)
- Refer to the patient’s right to make decisions for themselves according to theirown preferences. They can either agree to take treatment or refuse the treatment. The points of concerns are:-
Patient’s right to accept a treatment.
Reasons for patient’s refusal of treatment.
c. Quality of Life
- A major goal of medical treatment is to restore, maintain, or improve quality of life. Care management in treat-to-target should address the patients’ life goalsand include long term plan for stability and health. Quality of life is important in CD patients and their symptoms are directly proportional to the quality of thepatient’s life. The points of concerns are:-
Perception of quality of life
Normalization of symptoms
d. External Considerations (Justice)
- Involves provider bias or influences, resource allocations and payor decisions which effects the delivery of care for patients. Payors normally balance a budget and distribute their resources which might not be enough for the care the providers think optimum for the patient. There are differences in the providers view of what is needed and the payors view of what could be distributed in term of resources. Payor can look at different solutions to be more cost-effective, be more engaging in disease managements and partner up with experts to identify better support care for patients. The points of concerns are:-
What are the financial and economic factors involved in CD care?
Are there any problems for resource allocation?
Do payors have enough budget to cover the treatment?
Dr. Rubin gave us an overview of how decision in CD are made and the complexity of it involving the three parties. Although decisions are individually based on differing onpriorities and values, the ultimate goal should be the patients’ sustained functionalremission. Therefore, the three parties involved should figure out how to care for CD patients and optimize the quality of life and involve payor more in the CD care.
In summary, treat-to-target could be an effective way of treating CD patients with applying proper decision-making tools and involving all the decision makers (patient, provider and payor) to provide a better care, early treatment and allocate resources optimally.
Young, Nice, and Chronic Patient
Growing up is a process that we will all inevitably go through. We tend to live our lives with a sense that we are immortal. We learn to walk, we fall, we get up, we continue. Yes, life is pretty good. You learn a lot, you see new things, you spend a lot, you enjoy it. It is something that everyone does - living their life. It looks pretty simple until we start growing up.
In adolescence we begin to feel "older.” We go to school, we work for the coming of our adulthood. I looked like an ordinary teenager, I felt like an ordinary teenager - I thought everything was fine.
It was not exactly like that inside me. The reality was a little different. I was always the petite one of the class and I got sick often. The first symptoms of Crohn's disease began, which soon brought the psoriasis, then arthritis, and, recently, adrenal insufficiency.
New and full of life as I was, I was already setting goals for the future and dreaming. Yes, I was sure I would become an artist, I had decided.
Apart from some minor health issues, such as abdominal discomfort and lack of appetite, there was nothing wrong with me. That is, as far as I knew. I did not live in them, I was new. I was full of ambition!
I was about 15 years old when I began to realize that I should not take my health for granted.
I was at home relaxing listening to music when I suddenly collapsed in pain. I could not stand up.
A little later I was in the emergency room of a provincial hospital. Examinations, medications, but it seemed something temporary - it was not, as it turned out later. I was young, nothing could hurt me - or so I thought.
Then, I got some gastroenteritis (!) and it took me over a month to "recover" - obviously, since it was not gastroenteritis. Suddenly I started to get sick quite often. It had become difficult for me to live like an ordinary teenager, yet I was trying to go to school, the conservatory, and the orchestra.
I did not care much then, though. I was probably used to it. That was what I knew. I think my attitude started to change about a year later, when the visits to doctors and hospitals had increased significantly and I started to have more problems.
It was hard for me, as I suddenly had to struggle with things I had never imagined. I could no longer do what normal teens did.
As time went on, the "mysterious" disease then dissolved me more and more.
And life was moving on. I had to make brave decisions - it was not easy at the age I was then - as my health was deteriorating. I had to stop several things I liked or adjust them to the rhythms my body could handle.
I didn't do many things anymore. The only thing that kept me going was the music; it was becoming an increasingly important part of my life. I went to concerts very often because it was one of the few things I could do during that time. This made me face some of the difficulties I was going through.
After several years passed, I was then diagnosed with Crohn's Disease, psoriasis and arthritis. With the treatment I was receiving I was in remission and I had started to do everything. I was in university, I went on many trips, I went out and had fun, I went to concerts , I played in concerts. I no longer had almost any restrictions.
Until I began to feel very tired, nauseous, have a lack of appetite, and dealt with some other symptoms. I spent months looking for what had "broken" and why I felt that way. My examinations did not show any exacerbation of my known diseases. And then the day came when my rheumatologist told me to visit an endocrinologist and get tested for adrenal insufficiency, as the symptoms I mentioned made her believe that this diagnosis was very likely.
I could not make it to visit an endocrinologist because it was in the first wave of the pandemic, when everything was frozen around us, until I ended up in the hospital. A little later we had the results of my exams. My cortisol was very low, marginally detectable. My rheumatologist was right.
I was -again- newly diagnosed with something I knew absolutely nothing about and with a prescription for drugs I had never taken before.
In the following weeks I made the mental and physical adjustments to live with this new diagnosis that had just been added to my list of diagnoses.