NEWS
Digestive Disease Week 2022 and the Need for More Patient Voices
By Mara Shapiro (U.S.A.)
I had the privilege of attending Digestive Disease Week 2022 in person in San Diego at the end of May. I attended the conference as a member of the press for MD / alert (my employer). In addition to attending live sessions, writing articles, and interviewing doctors to create content as a medical journalist for my physician-oriented publication, I was also attending the conference through the lens of an IBD patient advocate.
This was my first time attending a medical conference, and it was a truly eye-opening experience not only professionally but personally. Getting to witness the excitement and gravitas of a major scientific gathering of top gastroenterologists from around the world was thrilling. Meeting fellow CCYAN patient advocates and CCYAN supporters was uplifting and rewarding. It is challenging to find enough adjectives for “excitement” as I describe all the highlights. I was very much like a “kid in a candy store” getting to be a part of the DDW experience.
However, I would be amiss to not mention the imbalance I felt as an IBD patient at a conference focusing so heavily on IBD research and scientific innovation. I, an IBD patient and the subject of most of these sessions and presented research, felt like my experiences were not being accurately represented. I felt lost in a slog of late breaking data and clinical trial endpoints. Where were the patient voices? How come patient narratives were not being presented? Why, in a sea of thousands of IBDologists (as they call themselves on #GITwitter), did I feel so alone?
I have to believe that there is a way to merge scientific discovery and research with patient advocacy, combine the clinician voice with the patient voice, and reach a collaborative understanding of what it means to live with IBD. So often in medicine, the patient’s experience gets forgotten or overshadowed by clinical research and treatment algorithms. Therefore, when patients do get a chance to share their story, it is often given a secondary stage or lesser attention.
What could happen if patient stories were used to aid in the contextualization of all medical research presented at these conferences?
I think we could create a discourse that is not just productive to clinicians and scientists, but that resonates with patients, the very focus and backbone of all this research. We can improve this disconnect. Patients should be able to recognize themselves in the research being presented about their disease.
Advice for clinicians and patients
For clinicians:
Please continue to support patient advocacy efforts such as CCYAN.
Continue to listen to and support your patients and their lived experiences of chronic illness.
Consider implementing more patient-reported outcomes and qualitative measures into your research.
Engage and network with patient advocates at conferences.
For fellow patients:
Continue sharing your story.
Remember that there is room for you at these conferences, and don’t be afraid to find your voice in these settings.
Digestive Disease Week: Empowered Crohn’s Disease Care
I would like to thank CCYAN for providing me this opportunity to patriciate in Digestive Disease Week (DDW) 2021. One of the sessions that I attended is “Empowered Crohn’sDisease Care: Targets, Tools and Talking Patients”. From this session, I have learned about the use of treat-to-target approach to treat Crohn’s Disease (CD), the tools that may help risk stratify patients with CD, and about the personalized approach to CD care. The session was split into three presentations, which were presented by Dr. Parambir S Durai, Dr. David T. Rubin and Dr. Corey A. Siegel respectively.
1) Treating to Target: Aiming for Endoscopic and Symptomatic Remission
By Dr. Parambir S Durai
What is the study about?
Dr. Durai presented about the use and benefits of a treat-to-target strategy in CD aimed at deep remission.
Presentation summary:
We need to understand how this treat-to-target approach work. Treat-to-target approach which is also known as a tight control strategy is used to achieve sustained disease control. Target and risk will be set during this time, assessment and continued monitoring have to be done to ensure targeted outcome has been reached. The most important goal in this treat-to-target approach is to achieve endoscopic healing, normalized quality of life and absence of disability.
The different studies mentioned in the presentation aimed to give CD patients early therapy using a treat-to-target approach. Treat-to-Target approach will be able to prevent adverse long-term outcomes. The studies suggest that the non-conventional methodsused at early treatment stage or frequently brings out positive outcomes to patients’remission.
Treat-to-target is treating CD patients until they achieve the desired target for the CD patients like us is healing. Healing can be mucosal healing where we go for endoscopy and the colon looks normal with no inflammation or ulceration. In some cases, there might even be histology healing which means when biopsy has done towards the colon or small bowel there is no inflammatory cells seen. In the case of a patient has fistula, then the target is to have closure of fistula. To achieve this target, the patient needs to be put under full remission.
According to Dr. Durai, patients whose response to the treatment by improvement in biomarkers results shown reduction in CRP and calprotectin. They may go for symptomatic remission. The next target is to achieve deep remission by continuing assessment and monitoring. At this stage, if the response is good, patient will be able to experience the huge improvement in symptoms, better quality of life, decreased in hospitalization and finally free from surgeries and disability and any serious disease- related complications.
Although the opportunities are huge and will provide patients with better quality of life or even achieving the absence of disability, there are some challenges that still exist in this approach. The first challenge is that treat-to-target is a time and commitment needed to follow through this approach as it needs more follow ups and more complexity of individualized process with the already busy clinical team. The other barrier is lack of knowledge of what might happen to patients later. Both patients and clinical team need to understand the limitation and provide active disease control to the patients.
2) Clinical Decision Tools: Assessing Risk and Taking Action
By Dr. Corey A. Siegel
What is the study about?
In his presentation, Dr. Siegel briefed about the importance of clinical decision support tools and suggested using clinical decision support tools to risk stratify patients for individualized CD care.
Presentation summary:
What are clinical decision tools? Dr. Corey explains that the decision-making tools are guidelines for medical providers to follow through different process based on different parameters. The tools can help to enhance medical decisions with provided clinical knowledge, patients information and other related information. And from the data gathered, doctors can formulating a diagnosis, assessing patients level of risk and help practitioner to improve the way they make decision to select medication for their patients from result shown from the tools.
Practitioner can apply several types of clinical decision support tools which has been developed such as AGA Clinical Decision Tool, IBD CDST, or CDPATH.
What can we learn from this presentation?
This tools help practitioner to decide right medication for patients based on the balance of risks and benefits especially at the early stage or before they develop complications.
By using these tools, it may help to reduce practitioners from making any risk of misdiagnoses and medication errors.
The tools improve efficiency and patients’ satisfaction.
. Give more confidence to practitioners to recommending right therapy and apply more aggressive monitoring technics.
3) Shared Decision Making in CD: The Path to Improving Quality of Life
By Dr. David T. Rubin
What is the study about?
Dr. Rubin discussed about the complexity of shared decision making for patient-centered and empowered CD care.
Presentation summary:
Dr. Rubin informed that the shared decision making involves three different parties. They are: -
1. Patient
- Person who suffer with IBD and request treatments.
2. Doctors/ IBD Nurses
- Medical provider who have fundamental knowledge about the disease and therapies which can be used to treat IBD.
3. Payor
- Person/company/agency who pays for the care and treatments for the patient.
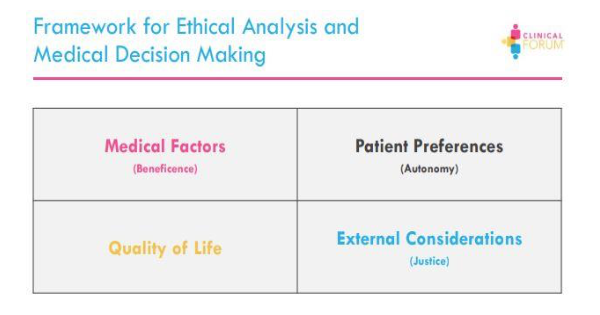
To make the relationship between the three parties happen there are several factors that should take to consideration by all the parties. Refer to diagram below:-
He further explains that, for each patient, the provider and payor must consider four variables: efficacy, safety, convenience and access. These variables help to makeprogress and provide better care for the patients. Practitioners can use “Ethical Analysisand Medical Decision Making” framework to make difficult medical decision. This can help to strengthen the doctor-patient relationship.
a. Medical Factor (Beneficence)
- This is a value in which the provider takes actions or recommends courses thatare in the patient’s best interest. The principle is based upon the objective assessment of a doctor, and what they feel is best for their patient. The points of concerns are:-
What is the patient’s medical problem? diagnosis? prognosis?
What are the treatment goals?
What are the therapies recommended?
What are the risk factors of the recommended therapies as well as the disease itself?
How are patients benefited by medical and nursing care?
How can harm be avoided?
b. Patient Preferences (Autonomy)
- Refer to the patient’s right to make decisions for themselves according to theirown preferences. They can either agree to take treatment or refuse the treatment. The points of concerns are:-
Patient’s right to accept a treatment.
Reasons for patient’s refusal of treatment.
c. Quality of Life
- A major goal of medical treatment is to restore, maintain, or improve quality of life. Care management in treat-to-target should address the patients’ life goalsand include long term plan for stability and health. Quality of life is important in CD patients and their symptoms are directly proportional to the quality of thepatient’s life. The points of concerns are:-
Perception of quality of life
Normalization of symptoms
d. External Considerations (Justice)
- Involves provider bias or influences, resource allocations and payor decisions which effects the delivery of care for patients. Payors normally balance a budget and distribute their resources which might not be enough for the care the providers think optimum for the patient. There are differences in the providers view of what is needed and the payors view of what could be distributed in term of resources. Payor can look at different solutions to be more cost-effective, be more engaging in disease managements and partner up with experts to identify better support care for patients. The points of concerns are:-
What are the financial and economic factors involved in CD care?
Are there any problems for resource allocation?
Do payors have enough budget to cover the treatment?
Dr. Rubin gave us an overview of how decision in CD are made and the complexity of it involving the three parties. Although decisions are individually based on differing onpriorities and values, the ultimate goal should be the patients’ sustained functionalremission. Therefore, the three parties involved should figure out how to care for CD patients and optimize the quality of life and involve payor more in the CD care.
In summary, treat-to-target could be an effective way of treating CD patients with applying proper decision-making tools and involving all the decision makers (patient, provider and payor) to provide a better care, early treatment and allocate resources optimally.
Digestive Disease Week: Positive Gluten Sensitivity Seriologies and the Impact of Gluten Free Diet in Patients with IBD
There are a lot of strong opinions surrounding gluten free diets. Some view them as a fad diet, popularized by media and celebrities. Others report real improvements in their GI symptoms when going gluten free. And of course there are those with Celiac Disease, for whom a gluten free diet is a life changing therapy. Throughout my time as an undergrad studying dietetics, I have learned about the gluten free diet from all angles. I think a lot of the confusion surrounding the gluten free diet in IBD comes from two sources. First, there appears to be a difference between what patients report and what the limited research has shown. Second, this limited research and lack of conclusive evidence has created a difference of opinions among healthcare professionals themselves. It is a difficult situation where providers using their clinical judgement can recommend for or against IBD patients going on a gluten free diet, and both recommendations would be completely justifiable.
In this article, I plan to give some background on the gluten free diet, and the current evidence for and against its use for patients with IBD. Then, I will summarize the wonderful study I learned about during DDW 2021 presented by Dr. Maria Moomal Dahar titled: Positive Gluten Sensitivity Seriologies and the Impact of Gluten Free Diet in Patients with IBD.
What is a Gluten Free Diet?
Gluten free diets are designed to eliminate the protein gluten from one's diet. Gluten is a storage protein found in some grains, including wheat, barley, and rye. Gluten is an important protein for baked goods, as it forms a sticky network that gives dough its characteristic stretch and elasticity. I don’t want to go too much in depth, as there is already an amazing article on the CCYAN website written by Leah Clark that describes the gluten free diet. If you desire to learn more about the specifics, her article can be found here.
The Gluten Free Diet and IBD
The main reasons to follow a gluten free diet are Celiac Disease, non celiac gluten sensitivity, and wheat allergy.
Previously, there had been conflicting data regarding whether IBD patients are at a higher risk of developing Celiac Disease than healthy people. Some older, smaller studies have found increased risk, while others have found no increased risk or even decreased likelihood of having Celiac Disease.1 A recent, larger study has shown that IBD patients have an increased risk of having celiac disease.
Non celiac gluten sensitivity is characterized by abdominal pain, discomfort, bloating, changes in bowel habits, fatigue, or depression after consuming gluten. The prevalence of non-celiac gluten sensitivity in IBD patients surveyed is reported to be between 5-28%.1 Those IBD patients who reported non-celiac gluten sensitivity were more likely to be following a gluten free diet. One thing I found interesting was that IBD patients were more likely to report gluten sensitivity if they also had a flare in the past 60 days. This points to the possibility that gluten sensitivity might be worsened in patients who are currently flaring or who have recently had a flare up of their IBD.
Most research on the gluten free diet in IBD patients has been done through survey based studies. Unfortunately, these types of studies can only provide weak evidence at best. The surveys did find that of IBD patients who had tried a gluten free diet, about 2/3 reported an improvement in one of abdominal pain, bloating, diarrhea, nausea, or fatigue. About 40% of patients following a gluten free diet reported less severe or less frequent flares. Contrary to those positive results, a different survey study found that there were no significant differences in disease activity, hospitalization, or rate of surgery in IBD patients following a gluten free diet versus those who were not.
A few different organizations and guidelines have weighed in on the gluten free diet and IBD:
The International Organization for Inflammatory Bowel Diseases currently states that in IBD “there is insufficient evidence to recommend restriction of wheat and gluten.”
The Crohns and Colitis Foundation states that “some IBD patients have found that a gluten-free diet reduces their symptoms, but researchers have not proven that it reduces IBD inflammation.”
The Asain Working Group guidelines on diet and inflammatory bowel disease state that “a gluten-free diet is not of a proven value in patients with inflammatory bowel disease.”
There are also some confounding factors when discussing gluten free diets. Gluten is often paired with fructans in foods, which are a type of fermentable carbohydrate that is associated with gastrointestinal symptoms. One study showed that 80% of patients with suspected non-celiac gluten sensitivity couldn’t be diagnosed after a gluten challenge.2 This points to the possibility that something found alongside gluten might be the culprit. Fructans offer a convincing alternative cause for why some might experience GI symptoms while eating gluten containing foods. Indeed, research has shown that in patients with suspected non-celiac gluten sensitivity, eating fructans was associated with more gastrointestinal symptoms when compared to eating gluten.3
Positive Gluten Sensitivity Seriologies and the Impact of Gluten Free Diet in Patients with IBD
When I first noticed this study as a part of DDW I was excited. I think that the study design is well thought out. The term “Celiac serologies” means that antibodies to proteins associated with consuming gluten were found in patients’ blood. These patients have immune systems that have already falsely identified these specific proteins as foreign invaders. By studying patients with positive celiac serology, the researchers were able to look at the effect of a gluten free diet in the patients that were likely to experience the greatest benefit from going gluten free.
The goal of this study presented by Dr. Maria Moomal Dahar was to determine if there were any differences in clinical outcomes between IBD patients with positive celiac serologies following a gluten free diet compared to those who were not following a gluten free diet. Out of the 1537 patients IBD patients looked at, only 89 had positive celiac serologies. Of these 89 patients, 29 reported adhering to a gluten free diet.
One interesting finding was that of the 89 patients with positive celiac serologies, those who were not on a gluten free diet were more likely to have a high ESR (measure of inflammation) and eosinophilia (associated with inflammation and infection).
Based on this study, the authors recommend testing for celiac serologies in patients with IBD. They also suggest a trial of a gluten free diet in IBD patients with confirmed celiac serologies.
My Closing Thoughts
It is so important that research is being done to evaluate the gluten free diet in IBD. Any time where a large majority of patients report improvement following a dietary trend, that should at least warrant some investigation into whether or not those improvements can be replicated in a randomized controlled trial. I am thankful for researchers like Dr. Dahar and her colleagues who are making efforts to further our knowledge in regards to the gluten free diet and its use in IBD.
One thing I also want to note is that the majority of therapeutic diets studied in IBD (IBD-AID, CDED, EEN, and SCD) all exclude gluten containing grains. Some of these diets show real promise in treating inflammation or alleviating symptoms of patients with IBD, and it is a trend worth noting. On the contrary, the mediterranean diet has also shown similar promising results, and includes gluten containing grains.
In my opinion, current literature is frustratingly inconclusive. Like many nutrition topics, there isn’t enough evidence to be able to make any strong recommendations one way or another. In light of that, I think that the best approach is the same one I echo all the time: Find out what works for you individually. You know your own body better than any study, scientist, or doctor ever will. So if you notice feeling better on a gluten free diet, maybe that is something you decide you want to continue even if the evidence isn’t quite there yet to show benefit in IBD patients.
Digestive Disease Week: New Concepts in Optimizing Bowel Prep for Colonoscopy
Needless to say, attending Digestive Disease Week (DDW) was a phenomenal and educational experience. Getting the opportunity to sit in on sessions led by medical professionals was an invaluable experience that will forever frame my way of thinking about IBD. DDW allowed me to expand my knowledge in a safe and inclusive space; some topics can be taboo, which can be a barrier to learning, but DDW truly allowed me to feel comfortable being able to synthesize, understand, and communicate complex medical information. I am forever grateful for this amazing experience! Dr. David Johnson, Dr. Douglas Rex, and Dr. Jack Di Palma were all amazing moderators and they helped expand my understanding of how we can modernize the almost universally hated colonoscopy prep experience. In this session, they discussed important aspects of bowel preparation in colonoscopy, including the efficacy, safety, and patient preferences of different prep options, overcoming barriers to bowel prep, and patient engagement and education.
As people who live with IBD, colonoscopies are routine to us, but as explained in the session, there haven’t been many advances in making the colonoscopy prep process more tolerable. As explained, “bowel preparation is often suboptimal, resulting in poor outcomes.” Speaking from personal experience, I have always felt like I’ve been prescribed too much prep, which has always made the experience even more daunting and unpleasant. Colonoscopy preparation should not be seen as one size fits all. This is where communication with your medical team is extremely important. During the presentation, the doctors gave a number of specific points related to modernizing colonoscopy prep. Some of these points include:
Involve nurses and pharmacists in the process
Having an interdisciplinary team can reinforce prep success. For example, having your pharmacist or nurse review all steps, discuss different prep options, as well as give you tips and tricks can lead to a more successful prep.
Increasing engagement and education
This section was particularly interesting for me as the doctors discussed different methods to increase patient engagement and education. One way was establishing a system where patients can opt in to receive reminder and educational texts during the prep process to ensure a higher prep success, understanding, and quality.
Moving toward a Low-Residue Diet as opposed to a clear liquid diet
The rigidity of the traditionally prescribed clear liquid diet can actually reduce the quality of prep. Having more leeway during colonoscopy prep and switching to a low residue diet can increase success and patient satisfaction. For example, instead of exclusively doing broth, gatorade, and jello we can slowly switch to a more tolerable diet that consists of whole foods like soft scrambled eggs, toast, bananas, and mashed potatoes, etc.
In conclusion, this session highlighted many ways that colonoscopy prep can be modernized and more successfully tolerated. We are all familiar with the prep process, the long nights, extreme hunger, and discomfort are just a few of the many feelings and symptoms we experience. It’s important to note that how well each person tolerates the prep is very individualistic; there is no universal remedy, which is why staying communicative with your medical team is extremely important.
I am especially excited to see further research over this topic so we all can have better colonoscopy prep. One of the overall goals, as stated by the doctors, is reducing the stigma of the terrible prep experience. We all deserve to have as smooth of an experience as possible, and there is so much hope and innovation waiting! Now, let’s hope a flavor-less prep is on the horizon, too.
This article is sponsored by Connecting to Cure.
Connecting to Cure Crohn’s and Colitis is a grassroots, volunteer organization that brings together the IBD community with a focus on caregivers and families. Connecting to Cure Crohn’s & Colitis provides community and support for those coping with these chronic illnesses, while raising awareness and funds for research as well.
Digestive Disease Week: Efforts to Understand Disease and Improve Management of Inflammatory Bowel Disease
DDW is one of those experiences I don’t think I will ever forget. Whenever I used to think about how researchers are out there studying Crohn’s Disease, it always felt detached. Like they are faceless people in labs hundreds of miles away. That changed with DDW. I could see the men and women working enthusiastically towards the betterment of my life. I could see their faces, I could hear their excitement, and suddenly research wasn’t this abstract idea any more. Research is now Ashwin Ananthakrishnan, Pabitra Sahu, and the countless other researchers who spend their time and resources in pursuit of a better life for people with IBD.
I could probably write about each and every IBD session at DDW, but I have chosen to focus on the session titled Efforts to Understand Disease and Improve Management of Inflammatory Bowel Disease. This was one of the first sessions I attended at DDW, and it covered a wide variety of topics. Within this session, two presentations stood out: Higher Resource Utilization and Economic Burden Associated With Fatigue in Inflammatory Bowel Disease and Randomized Clinical Trial: Exclusive Enteral Nutrition Versus SOC for Acute Severe Ulcerative Colitis.
Higher Resource Utilization and Economic Burden Associated With Fatigue in Inflammatory Bowel Disease
Fatigue can be one of the most debilitating parts of having IBD. Most of us have had days where everything we have planned becomes derailed because our bodies are exhausted. There is this idea that fatigue is a normal part of life for people with chronic diseases. Like it is expected, and therefore it isn’t worth addressing. I certainly know that fatigue gets put on the backburner at most GI offices. I’m not even sure if in my 5 years as an IBD patient that I have ever had a discussion about fatigue with my doctor.
I think that most IBD patients would agree that fatigue has not only a large impact on their disease, but on their life in general. This disconnect between how providers and patients view the importance of fatigue is challenged by the research presented by Dr. Ashwin Ananthakrishnan. He discusses the findings from his study focused on determining the economic burden of fatigue in IBD patients. Before we get into his findings, it is important to set the stage. The study presented was a Retrospective Nested Case Controlled Study.
Retrospective - looks at the past.
Nested - The case control was taken from a specified group of people
Case Controlled - IBD patients with fatigue were matched with IBD patients without fatigue.
The study looked at patients with both CD and UC who were newly diagnosed (<12 months). There were 21321(!) patients in the fatigue and non fatigue groups. Outcomes compared include rate of:
IBD surgery
Hospitalization
ED visits
Outpatient Visits
Total, medical, and pharmacy costs
The researchers looked at the above outcomes from all causes and from IBD specific causes. That is just to say that they wanted to determine if the hospitalizations, ED visits, and outpatient visits were because of the patient's IBD or some other outside factor.
So what did they find?
That is a significant difference in every. Single. Outcome. IBD patients with fatigue are more likely to be hospitalized, visit the emergency department, and have outpatient visits than those without fatigue. What did that mean for the costs? The researchers also found that IBD patients with fatigue had higher direct costs than those without fatigue. This was true in both mild and moderate/severe disease, showing that even in patients with mild disease fatigue increases healthcare costs.
This is huge. A lot of the time, in America at least, healthcare is focused on cost-benefit analysis. That is to say: if the insurance company spends the money, is the benefit great enough to justify that expense. This study shows that leaving fatigue untreated in IBD patients results in significantly greater expense, which in turn means that there is a huge benefit in making sure that fatigue is treated in IBD.
Overall, the study presented here reinforces the importance of treating fatigue in IBD patients. Fatigue appears to be a source of economic burden that warrants an increased attention and interventions. For IBD patients, hopefully this means that our providers have increased awareness of how fatigue impacts our day to day lives. Now that there is an understanding that fatigue is a problem, the logical next step in my mind is for research to determine how best to address fatigue in IBD. For now, frequent naps and an unholy amount of coffee will have to do.
Randomized Clinical Trial: Exclusive Enteral Nutrition Versus SOC for Acute Severe Ulcerative Colitis
The next study from this session I wanted to hone in on discussed exclusive enteral nutrition (EEN) in severe ulcerative colitis. EEN is when patients are fed enteral formula either by mouth or through a feeding tube for a period of time. It has been shown to promote mucosal healing, correct dysbiosis, modulate the immune system, and improve nutritional status. Currently, the best research for its use is in the pediatric Crohn’s Disease population, where it is considered a first line therapy. I am a huge proponent of the need for more research in EEN, which is why this study is so exciting.
The goal of this study presented by Dr. Pabitra Sahu was to evaluate + EEN vs standard of care for acute severe ulcerative colitis. Both groups received steroids treatment, so the main difference between groups was diet: EEN vs a normal diet in the standard of care group. EEN consists of peptamen, which is a semi elemental (partially broken down, easier to digest) formula. The study evaluated 62 patients, 32 in the EEN group and 30 in the standard of care group. The authors primarily wanted to know if EEN had a significant effect on corticosteroid failure, with a few secondary outcomes including measuring markers of inflammation and fecal microbiome analysis.
As far as the primary result, this study found that there was no significant difference between the EEN group and standard of care group when comparing the rate of steroid failure. This doesn’t take into account that 5 patients in the EEN group were found to be intolerant to EEN, and thus had to stop therapy early. When the authors compared the EEN group without these patients to the standard of care group, a significant difference in steroid failure rate was observed.
As far as secondary outcomes, there are a few worth mentioning. The EEN group had a significantly shorter duration of hospitalization when compared with the standard of care group. The EEN group also had greater reduction in CRP (measure of total inflammation) from day 1 to day 5 than the standard of care group.
Analysis of the fecal microbiome showed that there was a significant difference in the distribution of four bacterial genera. One bacteria, Erysipelotrichaceae (who thought that name was a good idea?), was increased in EEN. Erysipelotrichaceae has been linked with increased inflammation and disease activity in pediatric IBD, so it appears to be beneficial that the EEN group had an increased number of this genus.
To conclude, this study showed that there is a possible benefit to a short course of EEN alongside steroid treatment to improve steroid response rate, decrease duration of hospitalization, decrease inflammation, and modify the microbiome. While this study might not be strong enough to warrant using EEN for each and every severe UC patient, it at least provides another option to discuss with motivated patients looking to improve their chances responding to therapy. I know that if I were to be hospitalized I would want to do everything possible to increase my chances!
Digestive Disease Week: Diagnosing and Managing Pediatric IBD in the 21st Century
I am grateful to have had the opportunity to attend Digestive Disease Week (DDW) 2021. Learning about diagnosing and managing pediatric IBD in the 21st century allowed me to reflect on my own experiences as a pediatric patient through a different perspective. Two presentations stood out to me in this session.
To begin with, the first presentation that stood out to me,“Therapeutic Drug Monitoring with Newer Biologics”, was led by Dr. Lissy de Ridder who highlighted ustekinumab, vedolizumab and infliximab treatments. Dr. Ridder emphasized “treating-to-target” pediatric patients because of the lack of treatment options for this patient population.
Dr. Ridder explained what Anti-TNF therapeutic drug monitoring (TDM) has taught us about secondary loss of response:
A secondary loss of response that is immunogenic is categorized by a decrease of the drug and an increase of antibodies in the patient.
A secondary loss of response that is pharmacokinetic is categorized as a decrease of the drug and no antibodies in the patient.
A secondary loss of response that is pharmacodynamic is categorized as a sufficient level of drug and no antibodies in the patient but the patient does not respond to the drug.
The course of action for these different types of secondary loss of response according to Dr. Ridder:
A patient who has an immunogenic secondary loss of response to a drug will have the drug exchanged for a new drug in the same class and an immunomodulator will be added to the treatment plan.
A patient who experiences a pharmacokinetic secondary loss of response to a drug will have the dose of the drug increased and/or decrease the intervals that the drug is received.
A patient who experiences a pharmacodynamic secondary loss of response requires that the drug be exchanged for a drug of a different class or surgery.
Additionally, Dr. Ridder and her team conducted a study analyzing trough levels of young pediatric patients using infliximab and found that 75% of these patients were underdosed at the beginning of their treatment. As a result, these patients also did not have the recommended trough level and therefore responded less to infliximab. These results reveal that young pediatric patients responded less to infliximab because of underdosing.
Because of Dr. Ridder and her team’s study, the Medical Management of Pediatric Crohn’s Disease ECCO-ESPGHAN Guideline has changed to:
“In patients on anti-TNF agents, early proactive therapeutic drug monitoring [TDM] followed by dose optimisation is recommended. LoE:2 Agreement: 87.5”
Other highlights of Dr. Ridder’s presentation were:
Vedolizumab is more successful in UC patients compared to CD patients and is used after failure to anti-TNF in patients
Vedolizumab should not be used in patients with acute severe colitis
Ustekinumab should be used for CD patients who experience failure to anti-TNF and also patients who have severe psoriasis
The second presentation that stood out to me, “Results of the First Pilot Randomized Controlled Trial of Faecal Microbiota Transplant for Pediatric Ulcerative Colitis” was led by Dr. Nikhil Pai who highlighted patient interest in FMT and the barriers to FMT.
Dr. Nikhil Pai stressed that this trial was a result of a “significant patient and parent interest and emerging FMT data”. The study compared patients who received FMT treatments vs. patients who received placebo treatments for six weeks. The patients involved in this study were “UC patients between the ages of four to seventeen, had active disease, no CDI and no significant change in Rx in four weeks”.
The study highlights:
Fecal calprotectin significantly decreased in FMT recipients compared to placebo group
FMT is beneficial six months after initial treatment
Future studies of FMT should consider at-home treatment or oral encapsulated therapies due to the lack of feasibility of the study
Supports FMT for pediatric UC patients
Need for more FMT research
Overall, I am excited to see future studies about new treatments for pediatric patients with IBD and how these treatments will transition into adulthood.
Digestive Disease Week: Epidemiology & Natural History of IBD
DDW 2021: Epidemiology & Natural History of IBD
The Digestive Disease Week virtual conference kickstarted on Friday, May 21, 2021, with 5 societies (AASLD, AGA, ASGE, DDW, SSAT) taking part and over 15 different tracks. In the Inflammatory Bowel Diseases track, I joined the Epidemiology & Natural History of IBD session. Dr. Sunanda V. Kane, from Mayo Clinic, Rochester MN, opened the session, with the aim to understand how Inflammatory Bowel Diseases (IBD) are distributed through race, ethnicity and gender in the United States. The session hosted six speakers, covering the following sessions:
Session #1: Dr. Edward Lee Barnes – RACIAL AND ETHNIC DISTRIBUTION OF INFLAMMATORY BOWEL DISEASE IN THE UNITED STATES
This study used PCORnet (National Clinical Research Network) data as well as US Census data (2015).
Through this study, we learnt that:
Adult and pediatric patients with Crohn’s Disease (CD) or Ulcerative Colitis (UC) are more likely to be White and non-Hispanic.
Both adult and pediatric populations of Black/African American and Hispanic ethnicity are less likely to have a diagnosis of CD or UC as compared to White patients.
Comparing adult to pediatric populations, across race, shows that IBD diagnoses is rising among non-White populations, while staying more or less constant for White populations.
For drawing further inferences, it is important to conduct more research on health equity patterns among IBD patients, with an improved understanding of the demographics and epidemiology of these varied IBD patients.
Session #2: Dr. Fernando Velayos – PREDNISONE, BUT NOT BIOLOGICS OR IMMUNOMODULATORS ARE ASSOCIATED WITH SEVERE COVID-19 OUTCOMES: A COMMUNITY BASED STUDY
IBD management includes a series of immune-system-altering medications. In the context of COVID-19, this study sought to find out whether certain management techniques/medications put IBD patients at a greater risk for developing severe COVID-19 outcomes.
This study suggested:
The use of oral prednisone prior to SARS-CoV-2 diagnoses, is associated with hospitalization, ICU admission, and death. Thus, during the pandemic, doctors are advised to minimize outpatient steroid use where possible.
Immunomodulators and biologics are not associated with severe COVID-19 outcomes.
IBD is not an independent risk factor for severe COVID-19 outcomes.
Session #3: Dr. Mehwish Ahmed – CROHN’S DISEASE, ANXIETY AND DEPRESSION, AND BASELINE C-REACTIVE PROTEIN LEVEL PREDICT RISK FOR INCIDENT IRRITABLE BOWEL SYNDROME-LIKE SYMPTOMS IN QUIESCENT INFLAMMATORY BOWEL DISEASE
Approximately 41% of patients with inactive IBD report having IBS-like symptoms, leading to a lower quality of life. This study aimed to identify risk factors associated with IBD-like symptoms in patients with inactive IBD.
The study suggested:
Those with moderate to heavy alcohol use, comorbid anxiety or depression, use of psychotropic medications, increased C-reactive protein and the presence of rheumatologic intestinal manifestations are at higher risk for developing IBS-like symptoms.
Crohn’s disease, comorbid anxiety or depression, and increased CRP levels are independent risk factors.
Confirmatory data is required for further analysis.
Session #4: Dr. Mohamed Tausif Siddiqui – PREVALENCE AND OUTCOMES OF ALCOHOL USE DISORDERS IN PATIENTS WITH INFLAMMATORY BOWEL DISEASE
Alcohol has always been a potential trigger for IBD. However, more than half of the total number of patients with CD or UC, who identify as current drinkers, are moderate or heavy drinkers. This study sought to find out whether Alcohol Use Disorder (AUD) is associated with in-hospital mortality, keeping age, gender and ethnic trends in mind.
This study observed:
Irrespective of CD or UC, IBD in general, is affected by AUD, causing in-hospital mortality.
The risk factors associated with AUD are: (1) Age bracket [51-65], (2) Gender [Male], Race [Caucasian].
Session #5: Dr. Poonam Beniwal-Patel – RACIAL AND GENDER DISPARITIES EXIST IN INFLUENZA VACCINATION RATES AMONG PATIENTS WITH INFLAMMATORY BOWEL DISEASE
Patients with IBD are observed to have overall lower vaccination rates than the general population and are associated with an increased risk of infection, especially vaccine-preventable diseases (VPD). This study determined if disparities in race or ethnicity exist within immunization rates of patients with IBD.
The findings were:
Black patients had significantly lower rates than white patients for influenza vaccinations.
Female patients had significantly higher rates than their male counterparts for influenza vaccinations.
Future studies can assess the causes for these disparities, and advise on strategies to combat vaccine hesitancy. In the context of COVID-19, this research will be especially important for IBD patients.
Session #6: Dr. Chung Sang Tse – LOW HEALTH CONFIDENCE IS ASSOCIATED WITH SIGNIFICANTLY MORE HOSPITAL-BASED, ACUTE HEALTHCARE UTILIZATION IN PATIENTS WITH INFLAMMATORY BOWEL DISEASE: A NATIONAL SAMPLE OF OVER 18,000 ADULTS
Patient engagement and activation with regards to their health is a growing concern for positive engagement with healthy lifestyle choices and lessened emergency department (ED) visits and hospitalizations. Health Confidence is a proxy measure for this and is influenced by a multitude of factors, including personal beliefs, socioeconomic status, health literacy and disease specific knowledge.
This study showed that
The health confidence of patients who had an ED visit or hospitalization were lower than those without an ED visit or hospitalization.
A health confidence score of 7 (range 0-11 on Likert scale) appeared to be an inflection point for ED visits and hospitalizations, and thus for score less than 7, they should be considered at increased risk for the same.
Health confidence was not different between UC or CD patients.
“Interventions that increase health confidence may reduce high-cost, acute healthcare utilization.”
Digestive Disease Week: Role of Diet, Lifestyle, and Environment in IBD
I thoroughly enjoyed attending Digestive Disease Week’s session on Role of Diet, Lifestyle, and Environment in Inflammatory Bowel Disease. Let's start from the beginning and understand why studies surrounding diet, lifestyle, and environment are so important in understanding IBD.
IBD affects nearly 3 million Americans and over 200,000 Canadians. IBD is an immune-mediated disease that occurs due to certain, unknown environmental exposures in those with underlying genetic predispositions. Research on environmental exposures is needed to discover what environmental factors may contribute to an individual receiving an IBD diagnosis. This research will not only create an overall improved understanding of IBD, but also contribute to reducing the onset of IBD as well as cures for IBD.
Ultra-Processed Foods and Risk of Crohn’s Disease and Ulcerative Colitis
Two speakers in this session I found extremely interesting, the first being Dr. Chun-Han Lo. Dr. Lo reviewed his study on ultra-processed foods and risk of Crohn’s Disease and ulcerative colitis. The Western diet is thought to increase the risk of IBD through changes in the gut microbiome which can trigger immune function when compared to the Mediterranean diet.
Foods were separated into four categories from least to most processed:
Unprocessed
Processed culinary ingredients
Processed foods
Ultra-processed food products
Dr Lo explains that right now, it is widely known that higher consumption of ultra processed food products is associated with all-cause mortality, cardiovascular disease, metabolic syndrome, obesity, and cancer. Agents and thickeners, that are often added to ultra-processed food products, were also examined. The study aimed to examine the associations between ultra-processed food products and the risk of incident of Crohn’s Disease and ulcerative colitis.
The results indicated that higher consumption of ultra processed food products, specifically ultra processed grain foods and fat and sauces, was associated with an increased risk of Crohn’s Disease. Additionally, emulsifiers and thickener containing foods increased the risk of Crohn’s Disease. No subgroups had an association with risk of ulcerative colitis. This differentiates the impact food may have on Crohn’s Disease versus ulcerative colitis, furthering complexifying IBD. Further studies are needed on the effect of ultra processed food products in patients with established IBD may be warranted.
Although you may not be surprised by the results, studies like these are so important to allow room for more niche research and continue to allow researchers and doctors to understand the WHY behind IBD. As a Crohn’s Disease patient with many food intolerances, I am excited to see research surrounding diet and quality of food. There is little research backing the quality of food, and many suggest following a specific diet such as low FOD-map, gluten free, dairy free, among many others. It’s extremely exciting to see additional research surrounding foods, specifically processed versus unprocessed foods. My hopes are that this study can contribute to encouraging people to eat better quality foods and, in turn, reduce Crohn’s Disease diagnoses. Further, my mind jumps to future research covering whether reducing ultra processed food products after an IBD diagnosis could help treatment and management of disease.
Development of a Composite Environmental Score to Predict Age of Onset and Outcomes in IBD
Dr. Nidah Shabbir Khakoo spoke on the development of a composite environmental score to predict age of onset and outcomes in IBD. Specifically, Dr. Khakoo focuses on the fact that many environmental exposures associated with IBD are increasingly seen with Westernization. The study aimed to explore the relationship between individual environmental exposures and the age of onset of IBD. This study is extremely important in order to come to the understanding of what can cause a person to be diagnosed with IBD earlier in life, rather than later.
As someone with IBD, I have frequently wondered what environmental exposures in my life have caused my IBD to have an earlier onset? Why did I receive my IBD diagnosis in my early twenties compared to others that are diagnosed in their fifties? These studies are crucial to understand potential causes for earlier disease onset and overall understanding of IBD.
This study was administered on adult patients previously diagnosed with IBD. An environmental survey that queried age-dependent and lifetime exposures to various environmental factors were given among the participants to identify the environmental exposures each subject has had throughout their lifetime while looking at the age of their diagnosis. It is important to note that this study had a large number of hispanics, an underrepresented group in IBD research. The study looked at the age of disease onset, specifically comparing hispanics vs non-hispanics and Crohn’s disease vs ulcerative colitis patients.
Earlier Ulcerative Colitis Onset:
US Born
C-section Delivery
Fewer bathrooms
Decreased housing density
Ex-smokers
No farm contact
Earlier Crohn’s Disease Onset:
US Born
Water source - plastics
Fewer bathrooms
Decreased housing density
Smokers
Dr. Khakoo shares that the environmental score presented explains a greater amount of the variation in the age of UC onset than Crohn’s Disease onset. Additionally, weighted and not-weighted scores did not predict disease location, presence of extraintestinal manifestations, likelihood of surgery or hospitalization, or number of biologics needed. Certain environmental exposures, such as bottle feeding, showed opposing effects in ethnic groups with IBD, leading to assume that cultural and socioeconomic factors may influence disease onset.
These results give a baseline that other research needs to build off of. It is becoming increasingly evident that ethnicity differentiates environmental factors contributing to IBD and more research is needed to understand these differences. I’m looking forward to hearing of future studies regarding this subject and am hopeful more nuances regarding environmental exposures and the timing of IBD onset will be discovered.
It was great to hear from multiple experts about diet and environmental factors relating to IBD. I think that the data so far shows that there is a lot of work to do to understand what environmental factors contribute to IBD. I am looking forward to seeing future studies dive more in-depth to discover the causes of IBD. I am incredibly grateful to have heard from Dr. Chun-Han Lo and Dr. Nidah Shabbir Khakoo, and am confident these studies will have a large influence on future research on Inflammatory Bowel Disease.