NEWS
AIBD 2020: Clarifying Complications of Therapy
One of the sessions I delved deeply into on the first day of AIBD was “Clarifying Complications of Therapy”, which began with a presentation by Dr. Laurent Peyrin-Biroulet, MD from Nancy University Hospital, on malignancy (cancer) in IBD patients. Following Dr. Peyrin-Biroulet, was a presentation on infectious complications in IBD, by Dr. Edward V. Loftus Jr., MD from the Mayo Clinic.
Before delving into the details of risks and complications associated with immunosuppressive therapy, let us first outline which factors play into how immunosuppressed an individual is. First and foremost, not every patient with IBD is inherently immunosuppressed, rather only those who are on immunosuppressive medications fall into this category. Even amongst patients on the same drug, the following factors alter the amount of immunosuppression an individual may experience:
Increased age
Malnutrition
Comorbidities
Medications
Hospitalization
In other words, if two patients are both on the same immunosuppressive drug, but patient A is 20 years old with no comorbidities, and patient B is 60 years old and has COPD, patient B may be at a higher risk.
During the presentation on cancers in IBD patients, Dr. Peyrin-Biroulet noted that the focus was on anti-TNF drugs specifically, and that no robust data was available for other immunosuppressants. I want to make note of that, because this data does not speak for all IBD treatments, or all IBD patients.
Three of the cancers that were discussed in this presentation were skin cancers, lymphoma, and cervical cancer, all of which are associated with heightened risk in IBD patients who are immunosuppressed. That being said, Dr. Peyrin-Biroulet noted certain measures physicians can take to mitigate these risks as much as possible. I’ve created a simplified outline below for each of the cancers discussed:
Skin Cancer
Risk: there is an increased risk of non-melanoma skin cancer in IBD patients.
Prevention: use of sun protection and skin surveillance.
Lymphoma
Risk: there is a risk of lymphomas in IBD patients who are immunosuppressed.
Prevention: avoid more than 2 years of combination therapy in young males, and for older males who have tested positive for Epstein-Barr in their past, restrict the use of thiopurine drugs such as 6-Mercaptopurine (6MP), and azathioprine, as they may pose a greater risk of lymphoma in the patient.
Cervical Cancer
Risk: there is an increased risk of cervical dysplasia and cervical cancer in IBD patients.
Prevention: HPV vaccine is recommended to protect against HPV, which may lead to cancer.
In addition to Dr. Peyrin-Biroulet’s presentation on cancers associated with IBD and immunosuppression, Dr. Loftus spoke to the increased risk of other types of infections among immunosuppressed IBD patients. This included an increased risk of fungal infections, an increased risk for herpes zoster, and the importance of testing (and if necessary, treating) tuberculosis prior to starting anti-TNF therapy.
In the presentation, Dr. Loftus included a table that I found interesting and informative on determining whether or not to pause immunosuppressant treatment for IBD during an infection, in addition to treating the infection. I’ve simplified the table below, and added examples to the different drug classifications. Please note to consult with your doctor before making any changes to your actual drug treatment plan.
For Thiopurine (Including azathioprine and 6-mercaptopurine [6MP]):
Viral: you may need to stop immunosuppressants
Bacterial: stop, then individualize plan
Fungal: stop, then restart when cleared
C.Diff: continue
For Anti-TNF (Including but not limited to infliximab and adalimumab):
Viral: probably OK to continue (exception of Hepatitis B)
Bacterial: stop, then individualize plan
Fungal: stop, then restart when cleared
C.Diff: continue
Anti-Integrins (Including but not limited to vedolizumab):
Viral: continue
Bacterial: continue
Fungal: continue
C.Diff: continue
An Ecosystem of Advocacy
My fellowship at CCYAN is coming to an end. Coincidentally, I have felt short of ideas these few weeks. I’m writing this one late, partly because it has taken me a long time to fully recover from COVID, and partially because I was torn inside my head about what I wanted to say. Lately, my brain has felt like a cauldron with a stew of thoughts in it. I had been hiding safely in my home from COVID, but now that it got me, it’s time for me to go back to my pre-covid life.
At the time of writing, I’m about to fly back to my campus. I had deferred my exams for the previous semester hoping that the pandemic would settle down by Sept/Oct. That did not happen. I have lost a whole academic year. I now need to work twice as hard to get my degree. The pandemic has also doubled my healthcare expenses, and hence I need to work more than usual, which decreases the time I can devote to my academic work. I have also not been to the doctor in more than a year. After a long time, I have once again felt the fear of things going wrong and beyond my control.
One of the things that I’ve come to realise and feel in recent days is how isolating IBD can be. IBD symptoms can vary from person to person, but when you look at those symptoms in conjunction with life experiences, every one of us is on a very different path and fighting a very different battle. It is true for every chronic condition. One community, one group, can never be the answer. We need multiple communities composed of people with diverse experiences to thrive and work with each other. An ecosystem. Without that, there’ll always be someone feeling alone in their experience.
I have always been someone for whom repressing is more comfortable than expressing. Does that not make me inadequate for the job of a patient advocate? Repressing pain and trauma has enabled me to survive. The goal of life shouldn’t be to survive, though. I have compromised on every other aspect of my life so that every day I can do enough to stay on track with my goals and ambitions. Some compromises must be made, but some are forced upon by circumstance and external agents.
In the ancient world, people believed that the sick were cursed by gods. Treatment consisted of praying and giving a sacrifice to the gods. The ill thought that they were cursed. They were killed when the gods didn’t pay any heed to prayers. You might think times have changed, but they haven’t. Too many of us have been told that our illness is punishment for our past sins. Many of us believe it also, so much so that a patient recently said to me that their experiences didn’t matter because they were not good experiences. India is a country where the concept of “invisible disability” is yet to be introduced. In such an atmosphere, people with chronic conditions and invisible disabilities are forced to compromise. After all, it’s practical and easier for everyone. Any ill person that “complains”, does not radiate positivity and inspiration is useless. The attitude in general, towards sick people in my country, reminds me of the phrase - “Ignorance is bliss.”
So if you’re chronically ill - not only do you have to make compromises in various aspects of your life, not because they should be made, but because it’s comfortable for everyone else, you also do not have access to communities where you can share your frustrations, your experiences with people facing similar, if not the same set of circumstances.
Some say that we should not highlight our disability. Some argue that many people are successful with Crohn’s Disease or Ulcerative Colitis, but they do not talk about it. Talking about it is just asking for pity. The people who are going to succeed will succeed despite it. Such thinking patterns stigmatise our illness and strengthen the notion that patients are the problem, not the illness. Patients are not doing enough; others are.
As with everything else, things will not change unless we accept that there is a problem and that there is a real need. The irony in India is that those with voices do not have the need, and those with needs do not have a voice. There is an urgent need to build communities that provide support and advocate for better solutions.
I often feel that I say the same things every month, but I also feel that these things haven’t been said enough times. So to my fellow patients and the people who understand our needs - keep speaking up and keep talking, until our voices are too loud to ignore.
Thank you. Stay safe.
Finding the Moments That You’re Thankful For
I became obsessed with the card game Hearts during my sophomore year of college. Simply put, if you have the least points when someone else reaches 100 points, you win the game. You do this by avoiding the hearts suit and the queen of spades. Each heart is one point and the mighty queen of spades is 13. However, if you end up with all of the hearts and the queen, you can shoot the moon, giving you zero points for that round and giving the other three players 26 each. And sometimes you shoot the moon after starting out with a hand that was destined to be a horrible round.
November always rolls around and I get excited about Thanksgiving with family in addition to the other things I love about fall - the leaves, hiking, cool runs, coffee on the porch, football, you name it! But, more importantly, November is a time for me to reflect more closely on my year...what’s been good, what’s been bad, and what goals do I have for myself now? It’s almost laughable to say that in 2020, but I do have much to be thankful for. I think about how, almost five years ago, I was just starting to get the hang of living life with ulcerative colitis (UC), but I was probably bitterly reflecting back on the hand I was dealt that year.
I wish I could go back and comfort 23 year-old me and let her know things would get better. That the hand of mismatches wouldn’t seem so awful in a few years. That, in time, she’d be thankful for the support that encouraged her to do something with all of her frustration, anger and sadness when she was ready. Thankful for her own grit in deciding to share her own story to educate others and provide a safe space for anyone who didn’t feel seen or heard. And that was only the beginning - listening to patient after patient while on clinical rotations as a physician assistant (PA) student, truly hearing their stories reminded me of the providers that heard me when I had mild, easily dismissable symptoms, but ones that were way out of the ordinary for me. I’m now thankful that I’ve been an IBD patient myself and that I can use this experience to truly empathize with others going through a similar diagnosis one day.
I’ve also been so thankful to learn about my CCYAN co-fellows’ experiences; if you’ve read or watched any of our content this year, you know how amazing and inspiring they are. Their stories help me grow as an advocate, but also help me reflect on some of my darker memories of my IBD journey. For some, you may not remember because you were so young, and for others it may be all you’ve ever known. Yet, for another group, the line between pre- and post-diagnosis could be so sharp that it now demarcates two distinct periods of your life. I know some have shared that it is almost too painful to look back at certain memories during life with IBD, and that’s ok. However, I think the same people would agree with me that there’s still a light brightening that darkness. There’s still a new sprout growing from those ashes. The physical and mental pain we have all lived through serves as a stepping stone for strength. Just as we can look back and see the growth that came from the positive experiences we’ve had, we wouldn’t be where we are now without our painful experiences either.
Lastly, I realize you may not be at a place where you are ready to reflect yet, but I hope you will get to a point one day where looking back on your IBD journey can be helpful and perhaps cathartic for you. I’ve learned so much in less than 5 years - about myself, about others, and from others - that I’ll carry with me for the rest of my life. I will be a more empathetic PA in my career because of it and will always strive to be an advocate for IBD patients. Even though I initially looked at the hand I was dealt and my heart sunk, I think I found my own way to shoot the moon.
A Capital Mistake
Disclaimer: These are my views and observations, based on my experience with online Inflammatory Bowel Disease support groups in India.
“It is a capital mistake to theorize before one has data. Insensibly one begins to twist facts to suit theories, instead of theories to suit facts.”
~ Sir Arthur Conan Doyle, Sherlock Holmes
When I began my fellowship at CCYAN, I was a stranger to patient advocacy. I had a very vague idea of what the word meant. A couple of months later, I began a local initiative to explore the possibility of building a patient advocacy group for the Indian IBD (Inflammatory Bowel Disease) population. I started by imitating and trying to replicate the actions of existing advocacy groups in the US and the UK. However, it didn’t work. I soon realized that there is a larger fundamental problem that has to be addressed before I speak up for anything. It is the problem of patient education and health information.
Patients in India are far less aware and informed about their condition than patients in the developed nations. A higher rate of illiteracy, language barriers, lack of counselors, and short consultation times are major reasons. While it may seem that this problem can be rectified easily by disseminating educational materials among patients in various ways, the reality is that the void created by a lack of information is not a void at all. My observation is that the void has been occupied by incorrect and unsubstantiated information that prejudice a patient’s mind when it comes to learning and accepting correct, evidence-based information about their condition. This “defect” in the knowledge that a patient has about their condition can lead to deterioration of their condition and, in some cases, prove to be fatal.
The lack of patient education itself is a mechanism through which misinformation spreads. Existing patients with defective knowledge pass it on to the newly diagnosed. In the absence of rectifying sources/agents, such information can propagate and spread among groups of patients - very much like a virus. One of the places where things go “viral” is social media. The networks that connect us all are one of the pathways through which information that has no factual basis propagates.
In India, we have a small, but a fair number of Facebook and WhatsApp groups of patients suffering from Inflammatory Bowel Disease. Members of these groups exchange information daily on various topics - meds, diets, exercise, doctors, etc. I observed that there is a small subset of people, not always, but usually the creators of these groups that influence these discussions. This subset of people also acts as a source of “information” and “knowledge” for the other members.
In my experience, the majority of the discussions revolve around food and alternative treatments. Sporadically, there might be a discussion on the unaffordability of biologics, the struggle of young adults with the condition to get a job, study, or get into a relationship. However, these discussions are limited to a few comments, and that’s it. Several topics are not discussed out of shame. Erectile dysfunction because of IBD/surgery, anal dilation, rectovaginal fistulas, marital problems, reproductive issues - these are just some of the few issues that people seldom discuss in these forums. A support group is supposed to be a safe space, but these groups don’t feel like one to me. Nobody feels safe about opening up on problems that affect them very much because of fear of judgment and shame. The “advocates” too, rarely take any initiative to remove the stigma and taboo. We, the patients of India, with our ignorance, play a major role in keeping the taboo and stigma associated with IBD intact. The creators and moderators of such groups rarely take care to protect the newly diagnosed from misinformation. Many even float their own theories and post uncorroborated information.
A year ago, the mother of a 31-year old patient called me. She was crying. She asked me to visit her son and counsel him. I received her call a couple of weeks after I had moved to Bangalore for my graduate studies. I was unsure, but I went to her home and visited her son. He was lying down on the bed, with a heavily bloated stomach and a hot pack on his abdomen. I started talking to him. He told me that he had been diagnosed with Crohn’s disease 7 years ago. Initially, he was prescribed Pentasa, which he took for two weeks only. He did not feel that he was responding to the drugs, and hence, he stopped taking the medication without consulting his doctor. He never visited his doctor again.
On the advice of “advocates” and “experts” on the internet, he began buying and consuming naturopathy products, special brands of water with a certain pH, and many other products that he claimed were alternative medicine. He was importing many of these items. When he ran out of money, he borrowed money from people on the pretence of treatment and bought the products. He hadn’t seen a GI in 6 years! He showed me the results of a 3-year-old imaging test. It mentioned internal fistulas. He could not even stand up. His old mother was caring for him. Sometimes, when he would be in a lot of pain, his relatives would take him to the emergency room where he would be advised immediate surgery. He had been refusing the option of surgery every time. I spent an hour trying to talk him into surgery and explaining that an ostomy is not the end of the world. He wouldn’t budge. I returned - disappointed and angry. A few days later, I received a message from him. It said that he did get a temporary ostomy, but he’ll be going back to naturopathy to save his colon. I wished him all the best and urged him to act responsibly. I never heard from him again.
This person was ready to die instead of accepting treatment from a doctor in a structured and safe manner. He spent his time lurking on the internet in such “support groups,” where he learned various expensive and ineffective remedies for his condition and went on to irrationally and blindly pursue them. He could have avoided the surgery, had these very “advocates” told him to get back to his doctor.
Let me clarify here that I’m not speaking against the use of alternative therapies, some of which in recent times have been supported by some studies as a good supplementary treatment option. I object to disseminating unsubstantiated information in a manner that evades judgment, analysis, and scrutiny. Science, rational thinking, reason, is how humanity has come so far. It’s the gift we have—our capacity for reason and imagination.
Modern medicine does not fully understand inflammatory bowel disease and many other conditions. This, in turn, has become an opportunity for some people to form and present their theories which are either completely unscientific or based on some science, but completely opaque to scrutiny. These baseless theories and cures are dangerous. Desperate patients often end up losing a significant amount of money, time, and health. Such theories and their preachers often evade accountability.
We can only fight something well if we know what we’re fighting against well. I feel that most IBD patients in India are fighting blindly. The larger population of IBD patients in India faces a wide variety of problems compared to the handful of patients who have the luxury to engage in comfortable discussions in closed spaces on social media. Those problems are rarely discussed and confronted.
Inflammatory Bowel Disease is a complex disease. Good communication is the first step towards helping patients navigate the physical and emotional roller coaster that comes with having an illness like IBD. We must develop a culture of sharing medically verified and factual information amongst ourselves. It’ll help create a community where everyone is aware and informed. The newly diagnosed, who are often confused, shall receive appropriate guidance and support. Only then can we begin to speak up as a collective voice for matters that can help improve the quality of life of Indian patients with Inflammatory Bowel Disease.
That’s all from my side this month. Stay safe :)
The Difficulty of Finding a Treatment
For the ordinary individual, health is accepted as a given. It’s a part of life that mostly runs in the background like a minimized window on a computer. It’s always running, keeping us alive, and impacting our physical and mental states. Yet again, for most people, it’s rare to directly confront it on a minute to minute, or even second to second basis. Instead, it emerges at the forefront of life either by active and deliberate personal choice, or when something goes wrong. When a previously silent computer program running in the background becomes unresponsive, what was once insignificant becomes a major issue. To a greater extent, when that disruptive program causes our computer to crash and lose all of our work, it’s catastrophic. In a similar way, the typical individual goes to the doctor only on the occasions when their health is compromised by infection, injury, or other issues. Plus, when our health is stable and we are well, the changes we make, like starting a fitness regime, new diet, or implementing mindfulness strategies to our lifestyle, are done by choice.
However, when you live with a chronic illness, health management becomes significantly more complex. For one, chronically-ill patients often do not have the benefit of having a lifestyle defined by stable health. Chronic illness is by its very nature unpredictable. Diseases like Crohn's disease and ulcerative colitis revolve around periods of peaks and valleys - remission and flares. Once again, living with a chronic condition transforms the nature of managing health. The process of searching for, utilizing, and adjusting to a treatment for inflammatory bowel disease, or other chronic conditions, is one of trial and error. Unlike treating the common cold or a broken bone, the path to recovery is much less clear cut. Personally, I have tried various medications across a variety of different medication classes only to discover that they were not effective for treating my particular case of ulcerative colitis. It takes constant monitoring of your symptoms, and a commitment to embracing change to successfully navigate the healthcare system as a chronically ill patient.
It’s a difficult reality that many patients struggle through countless medications, clinics, and treatments before finding relief. Simply put, when you live with a chronic illness, your health is never certain. It’s unlike managing short-lived, common conditions, because there’s no clear timeline. Patients are forced to adjust to a new normal. This new reality is a reality where an individual must persist despite burnout, despite anxiety, and despite certainty. It involves significant sacrifices in one’s lifestyle, and even identity. Confronting health is no longer a special event or a choice, instead it’s a part of the daily routine. I believe this is part of why accepting illness is full of so many emotions, and why fatigue can easily take over. Everyday, patients are fighting a difficult, and often invisible, battle while living normal lives full of other responsibilities. The process, and the challenges, involved with finding and managing treatment do not make this balancing act any easier. Thus, it’s important to recognize the difficult, frustrating, and exhausting experience of patients worldwide. After all, despite illness, set-backs, and struggles, we persist to live lives as friends, artists, and advocates.
How My Mental Health Was Affected by IBD
Mental health has been on my mind a lot lately. From hearing it in relation to the COVID-19 pandemic, to having conversations about the need for more resources for IBD patients, to dealing with my own experiences with depression and anxiety - mental health resources are perhaps one of the most underrated and underfunded sectors of healthcare. I realize this as I’ve gotten older, immersed myself in the medical field, and as I have utilized it for my own mental health after being diagnosed with ulcerative colitis (UC) in 2016.
I bet many of you have also dealt with IBD affecting your mental health whether you realize it or not. For most of us, we were the only person we knew who had IBD at the time we were diagnosed. Some of us may not have even heard of it until we were told after our colonoscopy or endoscopy. The world around you suddenly feels a lot busier and bigger, and you feel very small and alone. Alone, wrapped up in your thoughts, your pain, your exhaustion, your fear. None of us asked for this. What did we do to deserve this?! In the days after my colonoscopy, this thought permeated my mind and I wanted to curl up in a ball and wish it all away.
But, you can’t do that when you are a busy pre-med student working full time and taking classes! We are expected to stay strong and keep up our front that says “Everything’s fine,” when, in fact, we’re not. I had great people to talk to and that would listen to me, but I still went through a mourning process. I mourned my life before when I thought I “just had a sensitive stomach.” I mourned that fact that my diet would probably change and change again and that I maybe would have to be on immunosuppressive medication. I dreaded the future conversations that would come up when someone would ask why I had to go to the bathroom so much or why I couldn’t eat or drink something. Really, everything’s fine…
But, it’s not. CHRONIC is a word that I hoped never to hear in regard to my medical history. We now have a new label that we must carry for the rest of our lives, and it’s anything but predictable. We have to explain this diagnosis so many times we feel like it might actually define us. The reality of my UC diagnosis began to truly sink in and anxiety began to seep into my daily life. My energy and concentration was poured into reading about UC, finding a better “diet”, looking for tips on how to achieve and stay in remission, and finding some kind of outlet for my anger and frustration.
Honestly, I should have given myself a little more time to process and try to seek the help of a mental health professional. Now, I think, I should’ve thought about my IBD and mental health together rather than separately. I let myself have a little time to mourn my UC diagnosis, but I thought I needed to be strong and keep my diagnosis to myself, much like others had before me. If we don’t look sick, perhaps no one will know. Even when we try our best to be strong and adapt to this normal, our mental health often still ends up suffering.
I think it would make such a positive difference in the lives of so many if we are all equipped with a medical and mental health treatment plan after being diagnosed with IBD, because the fact of the matter is that the mental health symptoms are just as debilitating as the physical symptoms of IBD, and they’re often intertwined. We need this kind of support as we manage our diagnosis - which sometimes can land us in the hospital or needing major surgery. I can’t speak to these kinds of experiences, but they can be traumatic in their own ways. How many failed medications or pain does one endure until they receive a potentially life-changing surgery? Thinking of the mental health hurdles that my co-fellows have dealt with and shared so vulnerably leaves me in awe of their strength. When they share what they have lived through, it also makes me sad that there was not adequate mental health services available to some of them when it could have offered an outlet for some of their pain.
Even now, almost 5 years out from my diagnosis, I take medication for my depression/anxiety and have re-established a relationship with a counselor that has experience in treating clients with chronic illnesses. I still go through the peaks and valleys of life and IBD, but, now, I’m better equipped to handle the lows when they hit or when a flare affects my mood and interest in doing things. I want the mental health support that has been so instrumental to some of my healing to be more accessible and affordable for those with IBD in the near future.
I hope speaking candidly about mental health and sharing some of these reflections helps you feel less alone and more validated in what you’ve been going through. The process of untangling all of these emotions is normal when grappling with a chronic illness diagnosis and what that means for you and those you love. Everyone processes major life changes and trauma differently, but don’t be afraid to ask about mental health services when you see your GI or primary care provider. Finding the right mental health support could be the treatment you never knew you needed.
The Acceptance and Struggle of a Childhood IBD Diagnosis
Being a kid is supposed to be a whimsical experience that one treasures and wants to have back. We long for those easier, good old days. But, when you are diagnosed with Inflammatory Bowel Disease at the age of 8, those childhood hopes can get lost.
When I was diagnosed with Crohn’s disease, I did not know what it was. I remember telling my friends and them thinking I kept saying “Crow’s disease” (granted, I did have a speech impediment). Honestly, even I couldn't fully understand what was going on with my body. I felt alone, isolated, and trapped in my body. I felt frustrated because of the lack of support I felt from my peers and the lack of communication that I could provide to the people in my life. I felt confused as to whether I was being too dramatic or if I was really as sick as I thought I was. It becomes hard to trust your body and self when—for so long—your symptoms are not understood. Still today, these emotions can flood my body when I think about my diagnosis or even have to deal with unrelated health procedures. The body has a mysterious memory intact.
In response to these events, I have found that I tend to forget things related to it. To be honest, pretty much everything—specifically during my diagnosis phase of life—is most often a blur. Being diagnosed as a child really made me deeply struggle with the faults of reality and mortality and sickness early on. My body is easily triggered by hospitals or doctors. Whether my response bodily or emotional, I cannot immediately make sense of it all at the time.
I often struggle making sense of my diagnosis. Being diagnosed at such an early age, the disconnect between what was real and fake is hard. How could it have such a constant effect on my life when I forget most details surrounding it? It can be hard when you are surrounded by so many people who have such an understanding of their diagnosis and can write such beautiful lessons they have learned when most days I do not even remember what age I was diagnosed at. It is so easy to compare journeys, thinking your IBD is not as bad as the next, or that you feel alone with it. But what we can hold is that we don't have to be positive all the time. It can be painful and we can hold both the pain and the lessons we have learned. We do not have to make sense of our diagnoses. There does not always have to be a bright side to everything and that does not make you less of anything. Everyone has their bad days, whether you see them or not. Just remember that it is okay to struggle, it's okay if not everything makes sense, and we are so happy to have you here.
Planning with Crohn's
Stay with me for this one – I promise it won’t be as boring as it sounds! If you immediately switch off when you hear the world ‘plan’, or indeed ‘regime’ or ‘strategy’, you’re not the only one! There are, however, benefits to planning when you live with a chronic condition like Crohn’s Disease – and more importantly, if your plans become routines, then they’re more likely to become second nature, and you’ll find yourself doing those tasks subconsciously. Here, I will share some of my planning tips, which you may just find helpful. It’s all about finding what works for you so that you can manage to fit in all of the things you want to do, despite your health condition(s).
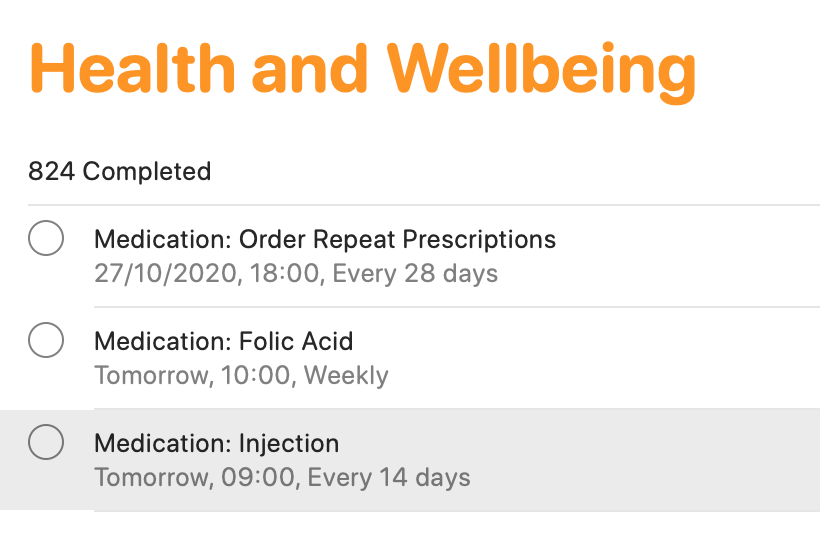
Smartphone apps
There are tons of smartphone apps available to help you keep lists, plan activities and so on! I keep it fairly simple, making use of macOS/iOS Calendar, Reminders and Notes (or the same apps on other operating devices). The calendar function is ideal for noting down all of your appointments. This helps for looking to the future, but also looking back at when and where different events occurred. The reminders app is an absolute lifeline for me. I have separate folders for different activities (e.g. university, health, work, voluntary commitments and so on). I add in activities, and a date/time (or location) reminder. This definitely helps me to keep track of everything that I need to do. If I didn’t, I would definitely forget! From a health tracking perspective, this is ideal as a reminder for booking in my next vitamin B12 injection which takes place every three months, as well as for when I need to ring up my doctor to arrange routine blood tests, when I need to self-inject my treatment, and when I need to order my repeat prescription. You may think that you’ll remember everything, but when you are busy with ‘life’, on top of ‘brain fog’ which many of us can relate to, it’s easy to forget. I know I have done that in the past, particularly when it came to self-injecting my treatment. I would remember that I need it on Tuesday for example, which would be the two-week dose period. However, I would have a busy day at college, would forget when I came home, and then in bed at night, I would suddenly remember, and think ‘I’ll have it tomorrow’. But then tomorrow became the weekend, and before I knew it, it may be a whole week later and I still hadn’t given myself my injection. I knew that was no good, but I just needed to do something about it – which I did!
Finally, Notes are brilliant! Again, I have different folders for a whole variety of different items. ‘Health’ is one of those. I use notes for keeping track of how I have been feeling, as well as for noting down points to discuss with my healthcare teams. I also use notes to keep track of discussions held with healthcare professionals, either face-to-face or over the phone. It’s just another good way to have information at your fingertips to help with your care, while the discussions are still ‘fresh’ in your head.
Scheduling in rest days
We all know what it’s like to live with a condition like Crohn’s – we have so much robbed away from us. As a result, when you are feeling on the better side, you will naturally try to fit in everything that you can. I know that I have been there! Though sometimes, it really doesn’t pay off. That’s why I try to give myself time and space to just ‘do nothing’ – because I know that’s what my body needs. In pre-pandemic times, I would avoid booking in too many back-to-back travels, so that I always had some time to recover. In the current climate, I do my best to block off certain days where I’ll have meetings, keeping overs ‘free’ to do work at my own pace, and also take it easy. It’s all about being in control, as much as possible, so that you give your body (and importantly, your mind) the time and space to breathe.
Leaving the house with everything that you need
Phone. Wallet/purse. Keys. Mask! The list goes on – but it’s really important to have everything that you need to hand. As well as the usual items that most of us require these days, I also have supplies in my backpack and car for every eventuality. This includes painkilling tablets and gel, anti-spasmodic tablets to help with cramps, laxative tablets if I notice a blockage, anti-diarrhoeal tablets if the opposite happens, lactase enzyme to help me digest products containing lactose and the RADAR key to access locked accessible toilets. This list can go on and will depend on personal circumstances. I always find it best to have everything stored in one bag, so you can ‘grab and go’. It may feel excessive, but you will thank yourself later on when you’re not caught short.
Knowing your triggers and avoiding them
Although everyone is different, we all have some kind of trigger which can worsen how we feel. For me, I know that stress is a key trigger for worsening symptoms. That’s why I try to minimise stress as much as is practically possible – although that is much easier said than done! That’s why you’ll generally see me planning to do work well in advance of deadlines, for example, and seemingly ‘being on top’ of everything. In reality, it’s much harder to do, and I do find myself rushing for deadlines still – but at least I have minimised that as much as is practically possible. I am also my own worst enemy. As a perfectionist, I place huge amounts of pressure on myself to succeed and to do everything to the very best of my abilities. While it’s a good quality to have, it isn’t when it impacts on your health. So, it’s really important to be kind to yourself, and to re-evaluate your workload if you find yourself totally swamped and feeling ill. Nothing is worth more than your health.
Do you have any other planning tips which help you to live with your condition whilst getting through life? Let us know in the comments and on social media!
There is No Right Way to Live with a Chronic Illness
I saw a quote the other day that said “There is no right way to live with a chronic illness,” and I immediately knew I needed to talk about it. Honestly, I want to get it tattooed on my forehead and shout it from the rooftops because everyone needs to hear it.
“Oh, you have a chronic illness and you eat that?”
“Oh, you have a chronic illness and you drink that?”
“Oh, you have a chronic illness and that’s how you workout?”
The answer to these questions?
There. Is. No. Right. Way. To. Live. With. A. Chronic. Illness.
There is no one right way to live. Period.
Unfortunately, yet realistically, there can be judgement within the chronic illness community at times. The same can be said for life in general.
And here’s what I have to say: IBD, and everything in life, is so incredibly individualized. What works for one person might not work for another. What works for me may not work for you. What works for you may not work for your neighbor Susan or your cousin Jack and vice versa.
Nobody should ever be shamed or put down or made to feel inferior or less than because of the decisions that they make in doing what’s best for THEM.
To think that there is one set way to live, one set way to eat, one set way to move your body, one set medication to take or not to take is to ignore an entire world that exists outside of your own.
When you really think about it, how cool is that life exists in so many different forms? How fascinating is it that I experienced this day differently than you? How awesome is it that we can find common threads that weave us together while still being uniquely ourselves?
So, the next time someone hits you with, “Oh, you have *insert condition here* and you do *x,y, and z*? I could never.”
Tell them how happy you are that they have found what works for them, how happy you are to have found what works for you, and how beautiful it is to simply be human.
Explaining Chronic Pain
This article is sponsored by Gali Health.
One of the most troubling and tricky feelings of the human condition is pain. It’s the body’s warning signal that something is wrong. It always seems to show up unexpectedly. It’s the world’s worst party guest. Seriously, it could at least bring a party gift, or an extra bag of chips and salsa to share. Instead, it interrupts the flow of midnight ragers and days of routine alike. Pain is the ultimate consumer. It takes, absorbs, and swells, without giving any of itself up. To make it even more complicated, pain comes in more hues, flavors, and shapes than can be counted. Pain is a universal experience, but the experience of pain is unique to each individual.
There is round, smooth, aching pain that rolls around the body all day. There’s sharp, jagged pain that cuts, stabs, and leaves a metallic taste on the tongue. There’s pain that shapeshifts. It howls like a werewolf, then sizzles like the sting from an insect. I could go on, but the list of the types of pain is again endless. That said, living with a chronic illness like IBD means tasting an entire buffet’s worth of pain types. Despite the fact that pain is so specific, and individual, people often try to measure and compare pain. As a chronically ill individual, it can be frustrating to have your pain compared, and rationalized by others. For instance, people will often compare the abdominal pain from ulcerative colitis, or Crohn’s disease to a stomach ache. In reality, chronic pain is much different from everyday pain.
When the pain from chronic illnesses is compared to pain from other illnesses, a large part of the context is ignored. Patients with chronic illnesses and pain have to confront pain oftentimes on a daily basis, and manage pain oftentimes without a totally effective treatment. The pain from a stomach ache, or a stubbed toe will eventually fade, and if it doesn’t, there is generally an effective treatment available. With a chronic illness, no such treatment necessarily exists. There is no timeline for recovery from the pain. Instead, it can be endless and unclear with multiple trials of various treatments required in order to find relief. In essence, chronic pain has no end deadline.
Despite this, the chronically ill often live normal lives everyday. Patients and pain sufferers go to college, go to work, and even to social events despite their pain. It’s especially important to remember this, because for all of its flavors, pain can be quite invisible. Dealing with pain is a challenge, and a burden, but millions of people around the world surmount the obstacle of pain everyday. Accommodations for patients make living with this weight easier, and enable us to be more active members in our communities. Still more work needs to be done to improve the quality of life for those dealing with pain. The compassionate way to treat the chronically ill, is the most inclusive way and the way that eliminates the disadvantages of the disabled. In the future, I hope all pain is treated with the utmost consideration and care for the individual. After all, if that was the case, there would be a lot less physical, and mental pain in this world.
This article is sponsored by Gali Health
Gali Health is an AI-based personal health assistant app helping people with inflammatory bowel diseases (IBD) proactively manage their condition. Gali gathers knowledge from daily interactions and health monitors to tailor support and information to your specific IBD experience.