NEWS
IBD, Mental Health, and Diet
Have you ever had a gut feeling before? Maybe you’ve had butterflies in your stomach when taking a risk, or felt something in the pit of your stomach when receiving bad news. Are these just idioms, or is there something else there? On my journey to become a registered dietitian, the connection between food and physical health is a common theme. Something we talk about much less is the connection between food and mental health. While Inflammatory Bowel Disease (IBD) is often thought of as a physical disease, the mental impact cannot be ignored. In my opinion, we don’t talk enough about the IBD and mental health connection, and we certainly don’t talk enough about how food can play a role in this aspect of our disease.
Mental Health and Gut Health
What does gut health have to do with mental health? Strap on your helmet, it's time for a crash course in the connection between gut health and the brain. The gut has over 500 million nerves, which serve as a two way communication system with the brain. If your gut isn’t happy, you better believe it is going to let its good friend the brain know about it. Our guts are also responsible for producing neurotransmitters, which help to regulate physical and mental functions of the body. One important neurotransmitter that regulates mood, serotonin, is produced 95% in the intestines! Another one, GABA, can be produced by the friendly bacteria in the gut, and can help reduce feelings of anxiety, depression, and fear.
Mental Health and IBD
As you can see, the gut and the brain are basically best buds. But what does that mean for people whose guts are broken more frequently than the McDonalds ice cream machine? Unfortunately, IBD patients are at an increased risk for developing anxiety and depression, and frankly, can you blame us? We are forced to bear the burden of a lifelong chronic disease, often being diagnosed during some of the most mentally vulnerable stages of our lives. High school is hard enough without explaining why you spend half of every class in the bathroom. It might seem like the connection between intestinal health and brain health is bad news, but there is a silver lining. If we can change the health of our gut, we can change the health of our brain.
Diet and Mental Health in Healthy Individuals
In healthy individuals, certain diets have been shown to increase feelings of wellbeing, reduce feelings of depression, and improve psychological health. Both individual foods such as fruits and vegetables, as well as dietary patterns such as the mediterranean diet, have been linked to these benefits. Some foods are also associated with worse mental health. Sugar has been linked with mood disorders and depression. Excess sugar consumption is also associated with dysbiosis, a shift in the composition of the gut bacteria from helpful to harmful species.
Diet and Mental Health in IBD
In a study presented at Digestive Disease Week 2020, researchers categorized IBD patients into two groups, a high sugar group (>100 grams per day) and a low sugar group (<100 grams per day). They found that those in the high sugar group had increased feelings of fatigue, trouble with social engagement, feelings of depression, and trouble relaxing compared to IBD patients in the low sugar group.
It is important to note that sugar containing whole foods such as fruit have been strongly linked to positive health outcomes, and should be considered differently than sugars from processed foods. Added sugars from processed foods such as soda or candy are associated with an unhealthy gut, and worse overall health.
I think this is such an important study, not only because it has practical implications for IBD patients, but also because it opens doors for patients to take control of their own mental health. I don’t think I've ever had a conversation with any GI doctor about mental health, despite the increased risk we carry with IBD. Until that changes, it is reassuring to know that we have the option to eat in a way that is associated with good gut health, and therefore good mental health.
References
Choi K, Chun J, Han K, et al. Risk of Anxiety and Depression in Patients with Inflammatory Bowel Disease: A Nationwide, Population-Based Study. J Clin Med. 2019;8(5):654. Published 2019 May 10. doi:10.3390/jcm8050654
Knüppel, A., Shipley, M.J., Llewellyn, C.H. et al. Sugar intake from sweet food and beverages, common mental disorder and depression: prospective findings from the Whitehall II study. Sci Rep 7, 6287 (2017). https://doi.org/10.1038/s41598-017-05649-7
Stranges S, Samaraweera PC, Taggart F, Kandala NB, Stewart-Brown S. Major health-related behaviours and mental well-being in the general population: the Health Survey for England. BMJ Open. 2014;4(9):e005878. Published 2014 Sep 19. doi:10.1136/bmjopen-2014-005878
Parletta N, Zarnowiecki D, Cho J, et al. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED). Nutr Neurosci. 2019;22(7):474-487. doi:10.1080/1028415X.2017.1411320
Brown K, DeCoffe D, Molcan E, Gibson DL. Diet-induced dysbiosis of the intestinal microbiota and the effects on immunity and disease [published correction appears in Nutrients. 2012 Oct;4(11)1552-3]. Nutrients. 2012;4(8):1095-1119. doi:10.3390/nu4081095
How to Start a Food Diary
Dear Diary,
Sometimes when I eat it feels like a herd of angry buffalo have taken up residence in my gut. The rumbling, the pain, and the regret are all too familiar at this point. Maybe I just shouldn’t eat at all. Maybe that would be best. I wish it could just stop…
Okay, I might not be talking about that type of diary, but I’ve had many days in my Crohn’s journey where that could have described me. Like many people with Inflammatory Bowel Disease (IBD), I have a frustrating mix of good days and bad days. It always baffled me how I could feel good one day, but terrible the next. I wanted to know why. This started my journey of paying closer attention to what I eat, and in turn, keeping a food diary.
Why a food diary?
Our environment is everything we come in contact with on a daily basis that isn’t us. The air we breath, the things we touch, and the food we eat all make up our outside environment. If nothing in our environment impacts a disease, it should feel the same every single day. For me, and many others with IBD, this just isn’t true. In this case, we must start looking at our environment as a source of triggers for our disease.
One of the largest parts about how we interact with our outside environment is what we eat. Every day we eat a variety of different foods, from a variety of different places, that have a variety of different health effects. For me, food was an easy place to start to try to figure out some of my disease triggers. I know what I am eating every day, so why not try to see if there is any connection between what I eat, and how I feel. This led me to food journaling, and it has been an invaluable resource in helping me navigate and manage my own disease. It has given me power.
Research also backs up this idea. In one study done in 2016, one group of Crohn's patients was told to exclude either the four food types they had the highest antibodies to, while the other excluded the four food types they had the lowest antibody to. The group that excluded the foods types to which they had the highest antibodies had significantly lower disease activity and significantly higher quality of life.1 We might not have access to antibody testing, but we can certainly try to figure out what foods are worsening our disease and quality of life.
How to write a food journal
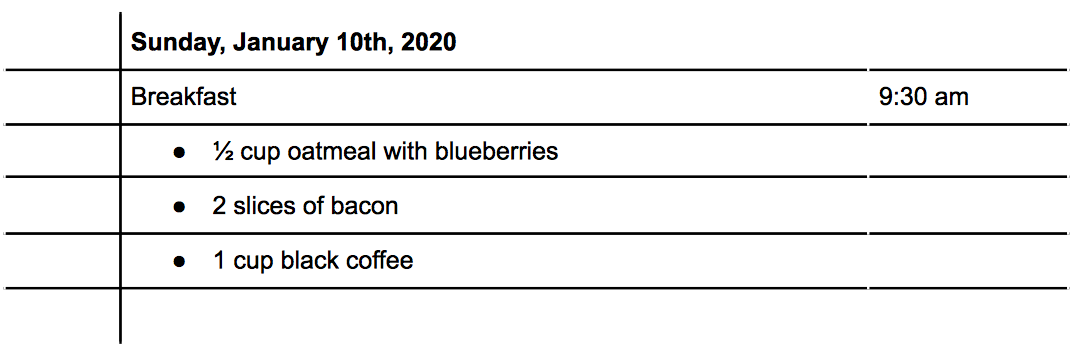
There are three main things to consider when writing a food journal: what you eat, the time you eat, and how much you eat. With these three written down, you will be able to better make connections between foods and symptoms. Let's do an example: For breakfast this morning, you ate a bowl of oatmeal with blueberries, some bacon, and a cup of coffee (I know, I know, coffee isn’t exactly known for its stellar track record in collaborating well with IBD, but it's a made up example!) How would that look?
Tracking Symptoms
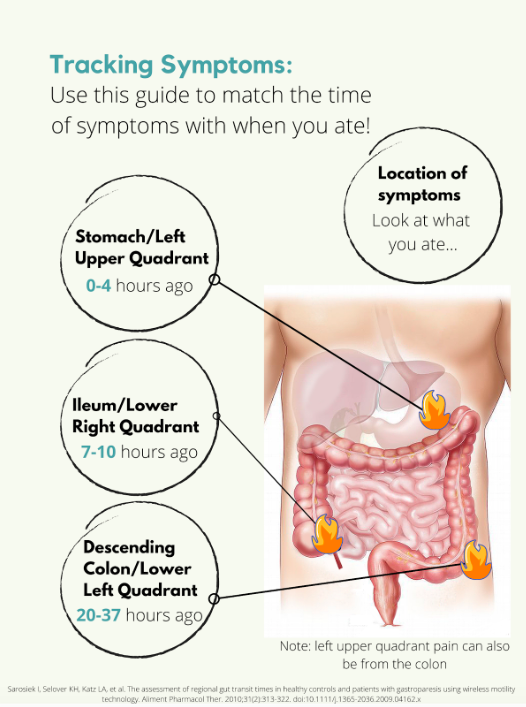
Symptoms are a little trickier. Say you have some pain in your lower right abdomen, how do you know what meal might have triggered you? Was it the meal you ate 5 minutes ago? 4 hours ago? The day before? For this we need to know a little bit about how long food takes to get to each different part of the intestines, also called the intestinal transit time. In a normal, healthy adult the following is accurate:
But what if you’re flaring? Diarrhea, inflammation, stricturing, and other aspects of a flare can all impact the amount of time it takes for food to get to the finish line. Some studies have been done on intestinal transit time in IBD patients, with most finding that the intestinal transit time is longer in IBD than in normal healthy subjects.2,3,4 In one patient with Crohn's disease, it took 156.2 hours for one meal to pass through. Talk about taking the scenic route! Like many other things with IBD, you are going to have to take an individual approach and problem solve to figure out how to best match symptoms and meals.
Resources
Tracking food can be done in something as simple as a spiral notebook, but there are also other options available. Here is a list of some apps you could use instead of a physical journal:
mySymptoms Food Diary & Symptom Tracker (Lite) by SkyGazer Labs LTD
Food Diary by WeCode Team
Cara Care by HiDoc Technologies
References
Gunasekeera V, Mendall MA, Chan D, Kumar D. Treatment of Crohn’s Disease with an IgG4-Guided Exclusion Diet: A Randomized Controlled Trial. Digestive Diseases and Sciences. 2016/04/01 2016;61(4):1148-1157.
Andersen K, Haase A, Agnholt J, et al. P-113 Gastrointestinal Transit Times and Abdominal Pain in Crohn's Disease. Inflammatory Bowel Diseases. 2017;23(suppl_1):S40-S41.
Fischer M, Siva S, Wo JM, Fadda HM. Assessment of Small Intestinal Transit Times in Ulcerative Colitis and Crohn's Disease Patients with Different Disease Activity Using Video Capsule Endoscopy. AAPS PharmSciTech. 2017;18(2):404-409. doi:10.1208/s12249-016-0521-3
Haase AM, Gregersen T, Christensen LA, et al. Regional gastrointestinal transit times in severe ulcerative colitis. Neurogastroenterology & Motility. 2016;28(2):217-224.
Navigating Diet Culture with IBD
By Amy Weider
Growing up food was always a celebration for my family. Food was how and why we would come together and build traditions. We would eat lobsters for every New Years to signify good luck and we'd come together to break the claws and soak them in butter. I remember watching my mother make us a classic midwestern casserole on a weeknight and the Food Network was never not on in the background. Food has always been such a critical part of my life. It brings me joy and memories. So when I started getting sick around 9 years old my relationship with it was forced to change. I began to have severe stomach pains and was unable to hold any food down. The first instinct when someone is having intestinal issues is to always investigate diet. My loving mother quickly made the switch to all-organic everything, bland food, and no more sugary drinks. At 10, I very quickly had to change what I ate and go on intense diets. It was hard for me, as food is such an important part of my life and a means of joy. But nevertheless, my family supported me through it and we went through the motions. Gluten-free for a bit, dairy-free, liquid-based only, we tried it all.
Alas, nothing worked. I was still, if not more, sick and constantly exhausted. Once the diets failed, I was given a colonoscopy and ultimately I was diagnosed with Crohn’s Disease. My Crohn's Disease was not fixed by a diet. In fact, no Inflammatory Bowel Disease (IBD)is caused or cured by food. Diet can help with inflammation or regulation of the disease, but diet also affects every IBD patient extremely differently. Most often, this is not how it’s portrayed and it’s hard for folks with IBD to carry the weight of the assumption that there is a one-size-fits-all cure. Ever since I first became sick, I have had people tell me constantly that if I ate a certain way I'd be fixed and that it is my fault I developed such nasty health problems. Hearing these things as a kid made me aware of diet culture very early on.
Diet culture is the world we live in. It is everywhere. Diet culture can be defined as the patrolling of people’s weight under the guise of health, while it is really about control, shame, and reinforcing eurocentric skinny body standards and eating trends. Concrete examples of diet culture are folks labeling certain foods as “good” or “bad”, or the shaming of others for not eating the “right things.” Diet culture and the weight-loss marketplace is a $70 billion industry. There is no way of avoiding these harmful tactics of major companies marketing off of your body’s imperfections and longing to achieve the societal standard of a femme body. It becomes very difficult to balance the thin line between diet culture and a change in your nutrition for your health’s sake. Specific diets that are used to help manage IBD are often glamorized as the “new, hot trend that will make you drop ten pounds quickly!” There needs to be a greater understanding of how privileged it is to merely treat these diets as fads. They are often highly inaccessible, expensive, and fail for those who are just casually attempting them. But for others, for example those who have Celiac, this isn’t an option for them. There is so much nuance that is frequently overlooked when prescribing diets and there needs to be more attention given to diet vs. health and nutrition. The mask that is diet culture can very quickly take over one’s life.
When you Google “Crohn’s Disease” you cannot miss the slew of diet suggestions for anti-inflammatory foods or titles like “Gluten-free Fixed My Life!” Hearing people make statements like “you could cure that by eating ‘blank’,” has become a huge trigger for me. My relationship with food has had its rocky times, but it’s still a place I find deep comfort. Comments like these stem directly from diet culture and the invalidation of lived experiences. There is no right way to have Crohn’s Disease. Everyone’s life experiences differ greatly and the main lessons I’ve taken away from mine are to be open, ask questions, and not push assumptions onto others. Open a space for folks to guide a conversation about their dietary restrictions and needs if that’s what they want. NEVER suggest a new diet to an IBD patient unless you are their medical provider. Trust me, we have heard everything.
Starting a Healthy Relationship with Food
By Erin Ard
What should I eat during a flare-up? What should I eat to stay trim? What should I eat to be healthy? What even CAN I eat? Every day I'm plagued with these questions. Even more aggravating, none of which have an easy, clear-cut answer. But having had experience fumbling over meal-planning and studying nutrition, I've learned how to better navigate my eating habits.
Planning and preparing healthy meals for yourself can be an exhausting, time-consuming, and sometimes expensive, process - especially for college students. Now if you throw in food allergies, intolerance, or chronic illness this process can get MORE complicated! Having inflammatory bowel disease (IBD), myself, I know how challenging it is to eat healthy within your own food restrictions; especially if you don't have a good understanding of nutrition, gastrointestinal disease, or what your restrictions are! My disease has been in remission for several years now, so my food limitations aren't as strict as someone having a flare-up, and I still have trouble. For those who are new to the game, IBD is a class of autoimmune diseases that causes inflammation along the GI tract when the disease is active, and can hinder nutrient absorption. With Crohn's disease, a common form of IBD, there is no specific diet to follow to control symptoms. This is probably the most annoying thing you've read today, but I better let you know now.. According to the Academy of Nutrition and Dietetics, we only know of foods to avoid - foods like dairy, high fiber grains, alcohol and certain spices, since these tend to aggravate an inflamed bowel.
Being the nutrition major I am, I get to learn about the Dietary Guidelines for Americans (DGAs). These are a great resource for curious readers wanting to eat healthy and live an active lifestyle. They lay out simple and easy recommendations to help prevent chronic illness, e.g. diabetes or obesity. These illnesses have become more and more prominent in the U.S. and have direct ties with diet. But what about the many other nutrition-related diseases with not-so straightforward ties? Unfortunately, the DGAs aren't designed for all bodies. The research used to develop the recommendations use “healthy” test subjects, of course, not those with chronic illness already. If you have a chronic illness, you’ll need to take extra care to find your ideal, health promoting diet. Better start doing some research yourself or see a registered dietitian! Or try out this idea you've probably never heard before, a food diary! …
Taking extra care in regards to your diet is especially important with IBD. In Crohn's disease specifically, inflammation along the digestive tract can cause nutrient deficiency. Inflammation hinders absorption of important nutrients, vitamins, and minerals; putting you at a higher risk of malnutrition than your healthy roommate. Eating the right nutrient-rich foods and eating enough of these foods can make-or-break living healthy with IBD. All of this in mind, the DGAs are still an easy “go-to” to help you learn about what makes up a balanced meal and why. In the rest of this article, I want to help you navigate the DGAs and share my own troubles with forming healthy eating habits.
Navigating the Dietary Guidelines for Americans with IBD
When comparing the DGAs and what is good or bad for a person with the common IBD form of Crohn’s disease, there are a few noteworthy similarities. For instance, limiting saturated or trans fats, simple or added sugars, sodium and alcohol are wise choices for everyone. They also seem to focus on getting a variety of vegetable and protein choices, emphasize fiber, and recommend lower fat options for dairy. Here you need to be careful. As noted before, certain sources of fiber can hurt a person with active disease. In other cases, fiber can be very beneficial for a person with Crohn’s to add fecal bulk, when the disease is in remission (i.e. under control or without symptoms). It's important for you to understand what foods are necessary for a well-balanced diet and what foods impact your disease management. The DGAs give a great outline, but your personal nutrition plan should have the final say in deciding what to make for dinner.
Dietary Guidelines for Americans 2015-2020
1. Follow a healthy eating pattern across the lifespan.
2. Focus on variety, nutrient density, and amount.
3. Limit calories from added sugars and saturated fats and reduce sodium intake.
4. Shift to healthier food and beverage choices.
5. Support healthy eating patterns for all.
My Relationship with Food
All of this information I have outlined is great and all, but I haven't touched on the emotional aspects of eating yet. Eating is heavily tied to the emotions I experience in a day. My mind bounces back and forth so much in a day when I think about food, eating, how I feel, how my gut feels, how much time I have before my next class, and whether I even have the energy to fix a meal up.
I eat when I’m sad and eat when I'm happy. I'll make a great meal to celebrate an accomplishment or make comfort food if my gut hurts. If I have an important event to attend, I will forego eating entirely to prevent symptoms. If I’m sad or stressed enough, I will also not eat, and wallow in my own pity. It’s confusing and raw, and I don’t understand my eating habits most of the time. Like I said, eating is a heavily influenced by my emotions, so how I feel about my Crohn's or about myself will impact what and if I eat anything. Unfortunately, I've discovered that a majority of emotions I experience will have me make bad decisions about food. But pausing to understand why I make these decisions and what fuels these emotions, has helped me to better understand myself. All of this aside, I love making food.
Striving for Progress
I used to have so many misconceptions about food. The biggest misconception I had to overcome was what I needed to eat to be healthy and what I should eat to look good. As a teen and throughout college, I was more absorbed in looking good, being thin, and keeping belly small. Not maximizing my nutrient intake by eating whole foods and managing my disease resurgence.
I used to be influenced by fads and testimonials - "stay away from dairy for clear skin", "stay away from breads and pasta and sugars to shrink your belly", etc. Everything affected me. Every headline I saw or piece of information I was told. Any advice I was given. Everything I interacted with tried to influence my thoughts, opinions, actions, and lifestyle. Here I thought I was being educated. I never realized I was depriving myself more than helping.
What I’ve been learning is that nutrition is not black and white. The world will try to convince you that there are foods you should not eat for X and foods you absolutely need for Y health benefits. Sadly, this isn’t true. There isn’t one perfect diet plan out there for everyone or for XYZ benefits. Nutrition is much more complicated than that.
With all of this in mind, I would say that right now, I have the healthiest relationship with food I've had in a long time. Studying nutrition was a major player, but I also must give credit to being mindful every day. Being mindful of my cravings and urges has helped me stay away from flare-triggering foods. And I make progress each day deconstructing any false beliefs on what I see as a "healthy" food for me.
My message to you is to educate yourself, learn about food, learn what foods you tolerate, and strive for a healthy relationship with food.
Bone Broth: Nature's Multivitamin
It seems that #guthealth has become popular in the wellness space over the past year or so. With more awareness of IBS, Leaky Gut, SIBO, and many other bacteria imbalances in the gut being displayed through the media, there has been an increase in remedies that are bound to “fix” all gut issues. I am an advocate for taking preventive, healing measures to get to the root cause and work towards better overall health - not necessarily relying only on medication. However, these so-called remedies are not a “cure-all.” While diet plays SUCH a significant role in gut health, but there are far too many factors that contribute to overall gut health that are often overlooked. In terms of IBD, chronic inflammation is exactly what it sounds like – chronic. Those who are facing this issue often try several things to help tame inflammation and improve their health, but there is not one “cure” that will work for everyone. Many things can trigger inflammation, and those are different for each person. Common examples include: food sensitivities / intolerance, stress, hormone imbalances, and mental strain. All of which can cause added irritation and stress to our system which results in inflammation and often the inability to turn off our “fight” mode.
While stress is a main component of a suppressed immune system there are plenty of other factors that influence the lining of the gut itself - factors such as prolonged exposure to antibiotics, inflammatory foods, toxins, etc. Eventually, if the impact of these factors pile up, the lining of the gut can suffer and result in permeability issues that may cause excessive inflammation due to malabsorption of food and minerals.
One thing I am currently working on in terms of my Crohn’s Disease is repairing the lining of the gut. Due to years of antibiotic treatment, inflammatory foods, and chronic stress, the lining of my gut has taken a toll and is not as impermeable as it should be. I am planning on writing a separate post about my current protocol, as well as the lifestyle changes I am implementing, but for now, I would like to talk about two things I have added into my routine and their role in digestive healing.
There is a chance that either in your research, scrolling through social media wellness accounts, or talking with your doctors, you have heard about bone broth. Many healing diets such as GAPS and the Specific Carbohydrate include this as part of the beginning protocol, and for a great reason! Nutrients and minerals in bone broth are essential to improve and heal the lining of the gut. These nutrients help decrease inflammation, balance good / bad bacteria ratios, and increase the immune response. Bone broth is nutrient-dense, easy to digest, rich in flavor and boosts healing within the entire body – what’s not to love!
What exactly is Bone broth?
You may think of broth that your mom used to have you sip when you were sick as a kid, typically what is used in homemade soups. However, bone broth is much different – it is nutrient-dense, thicker, and in my opinion, SO much better. Bone broth is the result of steeping the entire bone remains of the animal (beef, lamb, pork, chicken, etc.); including the bone, marrow, tendons, ligaments, etc. By including all of these components, the amount of nutrients found in this broth is significantly high compared to regular broths. Simmering using the “nose to tail” method of the animal protein source enables the bones and ligaments to release healing compounds like collagen, proline, glycine, and glutamine that are transformative for your health (1). Bone broths contain minerals and essential amino acids in forms that are easy for our body to absorb. Some of the minerals included are; calcium, magnesium, phosphorus, sulfate – all of which are often sold as pricey supplements and used to reduce inflammation, joint pain, and arthritis.
It is important to be mindful of the kind of bone broth you are consuming. Meaning, not all store-bought broth is created equal. If you’re not going to make your bone broth at home (from scratch), it is crucial to check the ingredients of what you are purchasing in the store! Like many other products, manufacturers like to sneak in monosodium glutamate (MSG), which is recognized as a meat flavor but is actually a neurotoxin – and as mentioned earlier, toxins affect the gut! When looking at the ingredients list, you should seek out whole, organic ingredients such as the bone broth (filtered water and animal bones), organic vegetables, and minimal spices. Try to stay away from added preservatives because to reap the full benefits of bone broth it is best to consume it in its most natural form – as our ancestors would have prepared it!
Overall, bone broth is a great place to find all of the valuable amino acids, collagen, gelatin, and trace minerals. There are dozens of different nutrients found within bone broth, many of which can’t be obtained easily from other commonly eaten foods! I am a firm believer in using food as medicine and consuming as much nutrient-dense food as possible. Broth is one of the easiest ways to check those nutrient boxes off without having to consume a massive pile of veggies in one sitting! By regularly drinking bone broth, or using it in recipes, you can promote healthy gut integrity while reducing inflammation and permeability. Now let’s dive into some other benefits from regularly consuming bone broth, shall we?
1. Protects Joints
I’ve already mentioned the anti-inflammatory properties that broth has due to the nutrients. But one of the BEST components found in this broth? Collagen. Bone broth is one of the world’s best sources of natural collagen – a protein found in vertebrae animals; in their bones, skin, cartilage, ligaments, tendons, and bone marrow. Collagen is very beneficial for the growth of hair, skin, nails, and bone health (2).
As we get older, our joints naturally experience depletion resulting in loss of flexibility. Supplementing with collagen matters because as we age, cartilage diminishes. As the broth simmers, animal parts release collagen and it becomes readily absorbable to help restore cartilage.
Another valuable component in the stock is gelatin. Gelatin acts like a soft cushion between bones that helps them move smoothly without friction. It provides the building blocks that are necessary to form and maintain strong bones. Significant amounts of both collagen and gelatin form and reform connective tissue to help take the pressure off of aging joints and supports healthy bone mineral density. It’s never too early to start taking preventive measures to make joint pain less problematic as you get older!
2. Boosts Detoxification
As I have previously mentioned, in our Western World, the average person is exposed to a variety of environmental toxins, pesticides, artificial ingredients and chemicals. The human body is amazing in terms of having its own means of detoxification from heaving metals and other toxins. However, it has a hard time keeping up when it is flooded with large amounts of chemicals. Much like if you were to procrastinate and become swamped with homework, you’re suddenly overwhelmed and may not perform your best on the task at hand. Bone broth is considered a powerful agent in detoxification because it helps the digestive system expel waste and promotes the liver’s ability to remove toxins. It also helps to maintain tissue integrity and improves the body’s use of antioxidants.
Stock contains potassium and glycine – both of which support cellular and liver detoxification. By supplying sulfur (especially with added vegetables, garlic, and herbs) and glutathione, an agent that lowers oxidative stress, detoxification is boosted. Glutathione helps with the elimination of fat-soluble compounds, especially heavy metals such as mercury and lead. It also aids in the use of antioxidants, the absorption of various nutrients, and with liver-cleansing functions! With the increased intake of essential minerals that bone broth stimulates, the minerals act to remove toxins by stopping heavy metals from attaching to mineral receptor sites. If they can’t bind, they can’t mess with our systems!
3. Supports Immune System Function
I have briefly mentioned at various times the permeability of the gut lining, inflammation, and a suppressed immune system. All of which contribute to multiple issues with what would generally be a healthy inflammation response.
Leaky gut syndrome occurs when undigested particles from foods seep through tiny openings in the weakened intestinal lining and enter the bloodstream. The immune system detects these invaders and becomes hyperactive to regulate the body. The hyperactivity increases inflammation and leads to dysfunctions all over, not just in the gut where the primary issue lies. The immune system releases high levels of antibodies that cause an autoimmune–like response and begins to attack healthy tissue. Individuals that already have a compromised autoimmune system, such as IBD patients, may suffer considerably more damage from a response because the system believes the particles in the bloodstream to be much more of an invader than a conventional system may.
Bone broth is observed to be one of the most beneficial foods to consume to restore gut health and therefore support immune system function and healthy inflammatory response. Collagen, gelatin, and the amino acids proline, glutamine, and arginine help seal the openings in the lining and support what is known as “gut integrity” – the intactness of the lining of the intestine to maintain its structure and function.
The amino acids and anti-inflammatory benefits create a perfect atmosphere for powerful immune-boosting to occur!
4. Good for the Gut
Bone broth stock is easily digested and soothing to the digestive system, unlike many other foods, which can be challenging to break down. Those with food sensitivities and intolerance (such as wheat or dairy) already have a hard time consuming many foods that may be considered “inflammatory.” Therefore, it is essential to look after the integrity of the gut, so vital nutrients are absorbed to support other bodily functions and overall health. After all, food is only useful if we have the means of absorbing its nutrients.
Bone broth has also been found to help heal the lining of the gastrointestinal tract. Critical components for digestion support that are found in bone broth include - collagen (proline / glycine), gelatin, and glutamine. Although there are many other beneficial minerals contained, these are most helpful to many IBD patients that have difficulty successfully digesting and passing bowel movements.
A healthy digestive tract consists of a single, tight layer of epithelial cells, a thick mucus layer, and a diverse group of microbes (bacteria in the gut). Gelatin is a significant component when it comes to the lining of the digestive tract because it supports a healthy lining of mucus within the system. The water is absorbed within to help maintain the layer of mucus that blocks gut microbes from the intestinal barriers. By drawing fluid into the intestine, the motility of the gut is improved, and healthy bowel movements are supported.
Collagen is another important component because it contains two essential amino acids: proline and glycine. Proline is necessary for the formation of collagen, and glycine works to improve digestion by increasing gastric acid secretion. Studies are currently being conducted and have shown that individuals with IBD, mainly Crohn's, are more likely to suffer from low stomach acid (3). Because the proper pH of the stomach signals the continuum of the digestive cascade, many people with low stomach acid face difficulty processing meals efficiently.
Summary
I know that was a lot of information, some of which may not have processed the first time reading it through - but that’s perfectly okay! Luckily you don’t need to know the names of all the essential amino acids found in bone broth to reap the benefits. I included this information because I know when I am learning about a new “supplement” that can improve my health, I’d like to know exactly how it works and why it is good. Many others like me enjoy doing their research to learn more, but others enjoy knowing the benefits, plain and simple!
So, another run down. When taken consistently, bone broth is exceptionally nutritious and works diligently to repair multiple components of your digestive tract. In addition to this, benefits are often seen through support in joint and bone health, hair / skin / nails, and detoxification processes of other organs within the body. It truly is impressive how functional this food is - hence, the nickname “nature’s multivitamin!”
I highly recommend giving this a try, whether you buy it from the store or experiment with making your own. I believe it’s wonderful! I drink mine first thing every morning, and it’s become something I look forward to - some people drink coffee, I drink bone broth (with an added scoop of collagen)! I hope you found this article informative and it piqued your interest to try something new, or reintroduce something back into your routine!
Stay Lovely,
Erin
Cooking with Crohn's - Gluten Free Strawberry Shortcake
Recipe for Shortcake
1 1/2 cups gluten free all purpose flour
2 3/4 teaspoons baking powder
1/4 teaspoon salt
2 tablespoons sugar
3/4 cup heavy or whipping cream
1 large egg
Instructions
Preheat the oven to 450°F. Line a baking sheet with parchment paper and set it aside.
Mix the flour, baking powder, salt, and sugar together in a large bowl.
In a separate bowl, beat together the cream and egg. Pour the wet ingredients into the dry ingredients and mix to form a cohesive dough.
Scoop the dough in 1 1/2-ounce balls onto the baking sheet; use the palm of your hand to gently flatten each to about 2" to 2 1/2" diameter.
Brush the tops of the shortcakes with cream, and sprinkle with coarse white sparkling sugar.
Bake the shortcakes for 10 to 12 minutes, until they're risen and baked all the way through; break one open to make sure.
Remove the shortcakes from the oven, split, and top with berries and whipped cream. Store, well-wrapped, at room temperature for several days; freeze for longer storage.
https://www.kingarthurflour.com/recipes/easy-gluten-free-shortcakes-recipe
Recipe for Whipped Topping
1 cup (8 fluid ounces) heavy whipping cream, chilled
1/2 cup (58 g) confectioners’ sugar
8 ounces cream cheese, at room temperature
1 teaspoon pure vanilla extract
1/8 teaspoon kosher salt
Instructions
Transfer 2 tablespoons of the cream to a small bowl and set it aside. In the bowl of a stand mixer fitted with the whisk attachment or a large bowl with a handheld mixer.
Place the remaining cream and beat on medium-high speed until soft peaks form.
Add the confectioners’ sugar, and continue to beat until stiff, glossy peaks form.
Transfer the whipped cream to a separate, large bowl and place in the refrigerator to chill.
In the same bowl, place the cream cheese, vanilla, salt and reserved 2 tablespoons cream.
With the whisk attachment, whip the cream cheese mixture on medium-high speed until light and fluffy.
Remove the whipped cream from the refrigerator and add half of the whipped cream mixture to the cream cheese mixture, and whisk to combine.
Add the remaining whipped cream, and fold it into the filling carefully until combined.
https://glutenfreeonashoestring.com/gluten-free-fruit-pizza/
IBD Diets: Gluten Free for Crohn's and Colitis
By Leah Clark
Because of the popularity of Hollywood fad diets, the term 'gluten-free' has become more and more popular over the past decade. While not necessarily intending to do so, this trend actually brought great change to individuals suffering from celiac disease, non-celiac gluten sensitivity, and inflammatory bowel diseases. With new food products coming to market and more menu items coming to restaurants, it has provided a new way for people that cannot eat gluten to experience food. As someone that was diagnosed with both celiac disease and #Crohn's disease ten years ago, I can confidently say I know my way around a nutrition label. That being said, not everyone that is on a gluten free diet, or that is planning on starting one, knows what to do. When discussing your treatment plans for your IBD with your doctor, discussing diet changes should not be forgotten. So, is going gluten free right for you?
Bacon, eggs, potatoes...who says living a gluten free lifestyle means giving up your favorite breakfast foods!
What is gluten?
With all these terms of gluten free, gluten sensitive, wheat-free, gluten-friendly, and more, it can be confusing to know what it all means! Isn't flour gluten, or is it any grain? To start with the basics of a gluten free diet, one has to know what to look for. Gluten is the proteins found in wheat, rye, and barley. So when on a gluten free diet, wheat, rye, and barely are the foods to avoid.
How to read labels
Okay, so know that I know what to avoid, what are the necessary steps to ensure that I don't eat the wrong foods? Check labels on everything. Even if you think something may be gluten free, it never hurts to read the nutrition labels. Certain foods don't have labels, such as fruits and vegetables; however, these foods do not consist of any other ingredients other than what they are called-apples, carrots, oranges, etc. Foods that are made with other ingredients, such as cereal, pasta, and crackers, are foods that need to be checked. Luckily, most companies are good about food labeling, so boxes will often say "Gluten Free" or "Contains: milk, soy, and wheat."
However, sometimes there are tricky labels that you need to look out for. For example, the cereal Rice Krispies is not #glutenfree. The ingredients include rice, sugar, salt, malt flavor, and vitamins and minerals. The key word here is malt. Although the other ingredients are okay, the malt flavor is not. Malt is a tricky word because it is not wheat, rye, or barely; however, malt is a derivative from barley. Therefore, Rice Krispies are not gluten free. Words like malt extract, malt flavoring, barley malt, wheat-germ, and non-gluten free oats, are words to look out for.
What foods can I eat?
A good rule of thumb is to stick to foods that are labeled gluten free, or are"natural" foods. By natural, I mean foods that are not made with large amounts of ingredients. A good starting gluten free grocery
list could include:
Fruit-apples, bananas, kiwi, oranges, grapes, strawberries, raspberries, blueberries, plums
Vegetables-carrots, corn, green beans, lettuce, spinach, broccoli, radishes, celery, zucchini
Milk-can be almond, dairy, soy, cashew
Protein-lean meats, chicken, eggs
Dairy products-cheese, gluten free yogurt, butter, cottage cheese
Grains-white or brown rice, gluten free oatmeal, gluten free breads and pastas
Gluten free pizza? Yes please! Restaurants have gotten better at properly preparing gluten free dishes, including delicious pizza, to make it easier for people to enjoying going out to eat.
Gluten free diet can not only be good for your gut, but also for other parts of your body because of how healthy a gluten free diet can be. Many of the foods listed are healthy in their nature, like lean meats, fruits, and vegetables. However, just because something says "gluten free," does not mean it is part of a healthy diet. Sure, chocolate is gluten free, but if all you ate was chocolate, would that be the best way to go on a gluten free diet? Probably not.
But I thought gluten free foods always tasted bad?
A common misconception about gluten free food is that it tastes gross. While yes, there are some bad gluten free food products out there, this is no different than there being bad gluten food. It all depends on your preferences and experimenting with different brands. Making home-made gluten free brownies is not as simple as using a Pillsbury box recipe of 'normal' brownies (although, there are some Pillsbury gluten free baking products that taste great). The point is to try new brands and baking techniques that work for you. I've spent the last ten years of my life finding my favorite brands of pastas, crackers, and bread, and I can honestly tell you, it wasn't I traveled to an entirely different country and tried their gluten free bread that I found my favorite. Gluten free food can taste just as good, if not better, than the food you're used to! It just takes some time and preparation.
How do I know if gluten free is right for me?
Honestly, it all depends on what you and your doctor think is best for you. I had to go gluten free because I was diagnosed with a disease that literally required me to. Yet, I know several people with Crohn's or colitis that have gluten free diets that do not also have celiac disease. In short, if eating certain foods make you feel bad, do not eat those foods! There are other foods I avoid even though they are gluten free, such as popcorn and caffeinated sodas, because I know they upset me. It truly depends on each person and if it is going to help with your treatment for IBD.