NEWS
A Post-Colonoscopy Reflection
By Mara Shapiro (U.S.A.)
Colonoscopies and endoscopies or “scopes” as I like to refer to them, quickly become a part of our lives as inflammatory bowel disease (IBD) patients. Everyone and their doctors’ are different, but most of us will get scoped every year or two for the rest of our lives. For pediatric and young adult patients with IBD, that can be a daunting realization. Even though they aren’t a major surgical procedure, the prep is torture, and it is still a day or two we need to spend away from school or work at the hospital and then recovering. It’s a lot. Scopes can become a huge source of stress and anxiety, they certainly are for me.
I just got my yearly scopes and it was definitely an experience I won’t forget. Between chugging Suprep at 4 am, wearing a diaper for the drive to the hospital, and then going into an adrenal crisis at home following anesthesia, this was an experience for the books. Like with other recent parts of my chronic illness journey, I’ve been trying to be more mindful of all these difficult experiences and what I can learn about myself and about life as a result. Here are some of my reflections from my latest scopes and from where my Crohn’s disease is at in general. I hope these reflections can spark some new insights for you as well.
I am stronger than I think.
For me, chronic illness is a constant reminder that I can do hard things. I can do hard things that previously terrified me. Not only can I do these hard things, but I can excel and come out the other end a stronger and more confident person. I try to go into big appointments, procedures (big or small), and flare-ups with the mindset that I am stronger than I think and know that I have what it takes to make it through. This is how I try to be positive and optimistic. I’m not perfect! I oftentimes struggle with negative self-talk and we are all entitled to feel bad for ourselves on occasion, but the difference is knowing deep down that YOU CAN DO THIS and returning to a similar positive mantra especially when things are tough. I went into these scopes with the mantra that “I am stronger than I think” and “I can do hard things” and I survived and I’m proud of myself for getting through them with such a positive mindset.
It’s all about the mindset.
Over the past year, I have really focused a lot of my energy on my mindset and the narratives I am telling myself about what’s going on around me. I have found that being in control of my mindset, and how I feel and view what’s happening, has allowed me to create a much healthier relationship with my chronic illness(es). For example, I went into these procedures with the mindset that: This is going to be hard, I’m going to hate it, but I can do it because I can do hard things. I need to do this for my present and future health. This mindset that I am suffering for a few days for information that will help my doctors and I better control my IBD was very humbling for me and gave me that extra motivation to chug that last gulp of Suprep.
I know my body best.
In addition to having Crohn’s I also have Addison’s disease, a form of adrenal insufficiency where my adrenal glands don’t produce any cortisol (our body's natural stress hormone needed for most of our bodily function). Since January 2022 I have been on a cortisol pump which allows me to get a 24/7 continuous subcutaneously infusion of cortisol in a way that closely mimics the circadian rhythm pattern of a healthy person’s cortisol cycle. This treatment has been life-saving and given me my life back in remarkable ways that are hard to express. Having surgery or anytime my body is under intense periods of physical stress can be dangerous because my body does not naturally increase cortisol production in response to stress the same way a healthy person does. I need to manually try to guess how much extra cortisol I need and also increase my dose for a few days or longer. This was my first time going under anesthesia since having Addison’s disease. Long story short, the anesthesia team did not follow the protocol my endocrinologist wrote out and I ended up going into an adrenal crisis within an hour or two of returning home after the procedure. I am very thankful for my intuition and my dad’s help - we were able to quickly increase my cortisol pump rate and within a few hours, I stabilized. Thankful is the only way to describe how I feel, as this situation could have easily ended differently. Especially after this incident, I always know that I know my body best.
Remission is not a cure.
Thankful is also how I feel that my scopes showed no signs of active disease. Stelara is continuing to work wonders for my Crohn’s disease. However, even though I am in “endoscopic remission”, I am still not symptom-free and there’s a common misconception that being in remission means you’re cured and good as new. I hope in time I will become one of those patients who forget they have IBD, but for now, even though my ileal ulcers have begun to heal, I still have just as many bad days as good ones.
I have Crohn’s but it doesn’t have me.
This one is a bit cheesy but throughout the course of these procedures, I realized that I am in control of my disease. By in control, I mean that I have the power to decide how much my disease impacts my life regardless of how much power and control it tries to take from me. Even on the days when I’m in a lot of pain and not sure how I’ll be able to get more than a few feet from the bathroom, I am still in control of how I let that affect me. My disease is not my entire identity nor my self-worth, it is just a part of me. I have Crohn’s and it’s a huge part of who I am and how I interact with the world, but it is not my entire world. There’s a lot of strength to be found in being able to reclaim some of the power and control that this disease has previously had over me.
Featured photo by Scott Webb from Pexels.
My Ileostomy Story
By Carina Diaz (Texas, U.S.A.)
In May of 2021, I went to the ER for what felt like the millionth time. I had been struggling with cysts and abscesses forming in my vagina for the past three years and this time was no different. Or so I thought.
I had already been to the ER earlier that week and was seen by a male doctor who, in hindsight, wanted to quickly drain the cyst and get it over with to move on to the next patient. I told him that I wanted a CT scan, but he said it wasn’t necessary. For my second ER trip of the week, I was seen by a female doctor. I made a comment about this being my eighteenth time having to do this in the last three years and with a look of concern on her face, she said, “That’s not normal. Let’s do a CT scan.” To which I said, “Brilliant idea.”
The part that I hate most about going to the emergency room is having to wait. And wait. A nurse takes your vitals. Then you have to wait. Someone comes to get your insurance information. More waiting. You tell the doctor what’s wrong. Even more waiting. The doctor comes back with a nurse. They do what they need to do. And you wait some more for either discharge paper work or to be admitted.
After getting a scan, it was decided that I would need incision and drainage surgery. But guess what? My gynecologist only does surgery at one hospital and it wasn’t the one I was currently at. So I had the joy of, you guessed it, waiting for an ambulance to come to transport me to another location. Watching the night sky through the back windows wouldn’t have been so bad if I wasn’t strapped to an uncomfortable bed made of plastic.
This was the second time I’ve had to get incision and drainage surgery, so it wasn’t a new experience to me. What was new was being presented the choice of potentially having to get ileostomy surgery. It would give my colon a break and let the fistula heal (a surprise that was discovered during the surgery).
To be honest, getting an ostomy bag was the worst-case scenario in my head as someone with Crohn’s Disease. It sounded scary and uncomfortable. What clothes could I wear? Would people see it? Would I smell? Am I going to wake up in pain after the surgery? When the hell will I be allowed to eat?! I don’t want a poop bag strapped to me. All of these thoughts were floating in my head while three doctors stood in front of me explaining the process. The good thing was that it would be temporary.
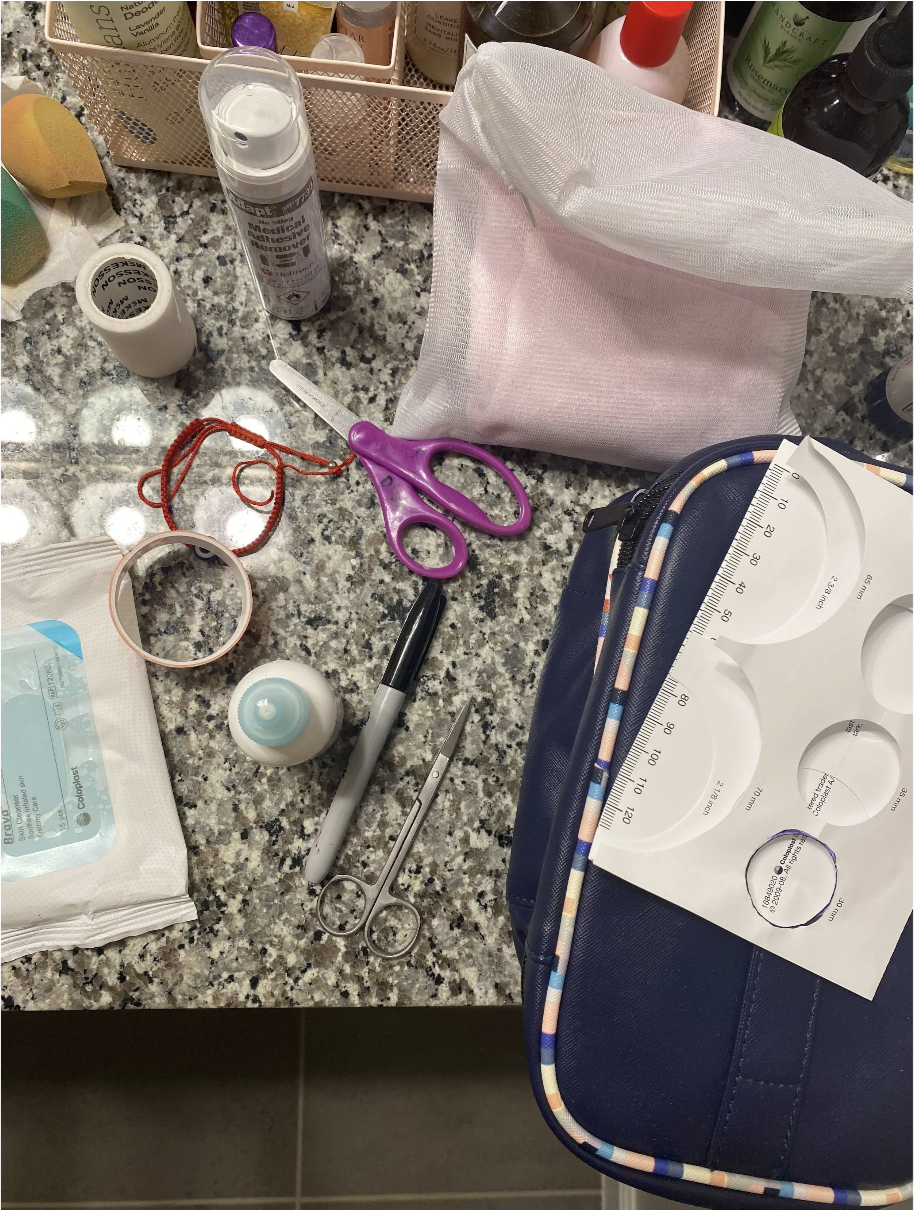
I let a doctor use a robot to cut me open and pull a bit of my intestine out. I didn’t wake up in pain, but I was scared to look at my body. The rest of the week was a blur of learning how to empty it, clean it, and how to live with this new change.
At the time of writing this, I’ve had an ostomy bag for ten months. While it has greatly improved my quality of life and lowered the severity of my symptoms, it has definitely been challenging. I have three different skin conditions, so my torso really hates having something taped to it. I have yet to find a bag that doesn’t irritate my skin. During my second month after surgery, I kept getting blowouts at night and barely got any sleep. It was painful and itchy. My ostomy nurse likes to describe me as “a real head scratcher.”
Having IBD makes me think a lot about the duality of life. I’m grateful that this surgery was an option for me because it has helped in many ways, but I still have to make sacrifices. I still have to deal with discomfort, and I’ve had to relearn my body yet again. That cycle will continue when I eventually (hopefully) get reversal surgery at some point.
Some people have positive experiences with ostomies and say that it has given them their life back. If that’s not the case for you and you’re also struggling with having an ostomy, try to remind yourself that you’re doing your best. Take it one day at a time and cry when you feel the tears forming. I recommend watching your favorite show if you’ve had a hard time changing your bag. Those stomas can be so unpredictable.