Mental health has been on my mind a lot lately. From hearing it in relation to the COVID-19 pandemic, to having conversations about the need for more resources for IBD patients, to dealing with my own experiences with depression and anxiety - mental health resources are perhaps one of the most underrated and underfunded sectors of healthcare. I realize this as I’ve gotten older, immersed myself in the medical field, and as I have utilized it for my own mental health after being diagnosed with ulcerative colitis (UC) in 2016.
I bet many of you have also dealt with IBD affecting your mental health whether you realize it or not. For most of us, we were the only person we knew who had IBD at the time we were diagnosed. Some of us may not have even heard of it until we were told after our colonoscopy or endoscopy. The world around you suddenly feels a lot busier and bigger, and you feel very small and alone. Alone, wrapped up in your thoughts, your pain, your exhaustion, your fear. None of us asked for this. What did we do to deserve this?! In the days after my colonoscopy, this thought permeated my mind and I wanted to curl up in a ball and wish it all away.
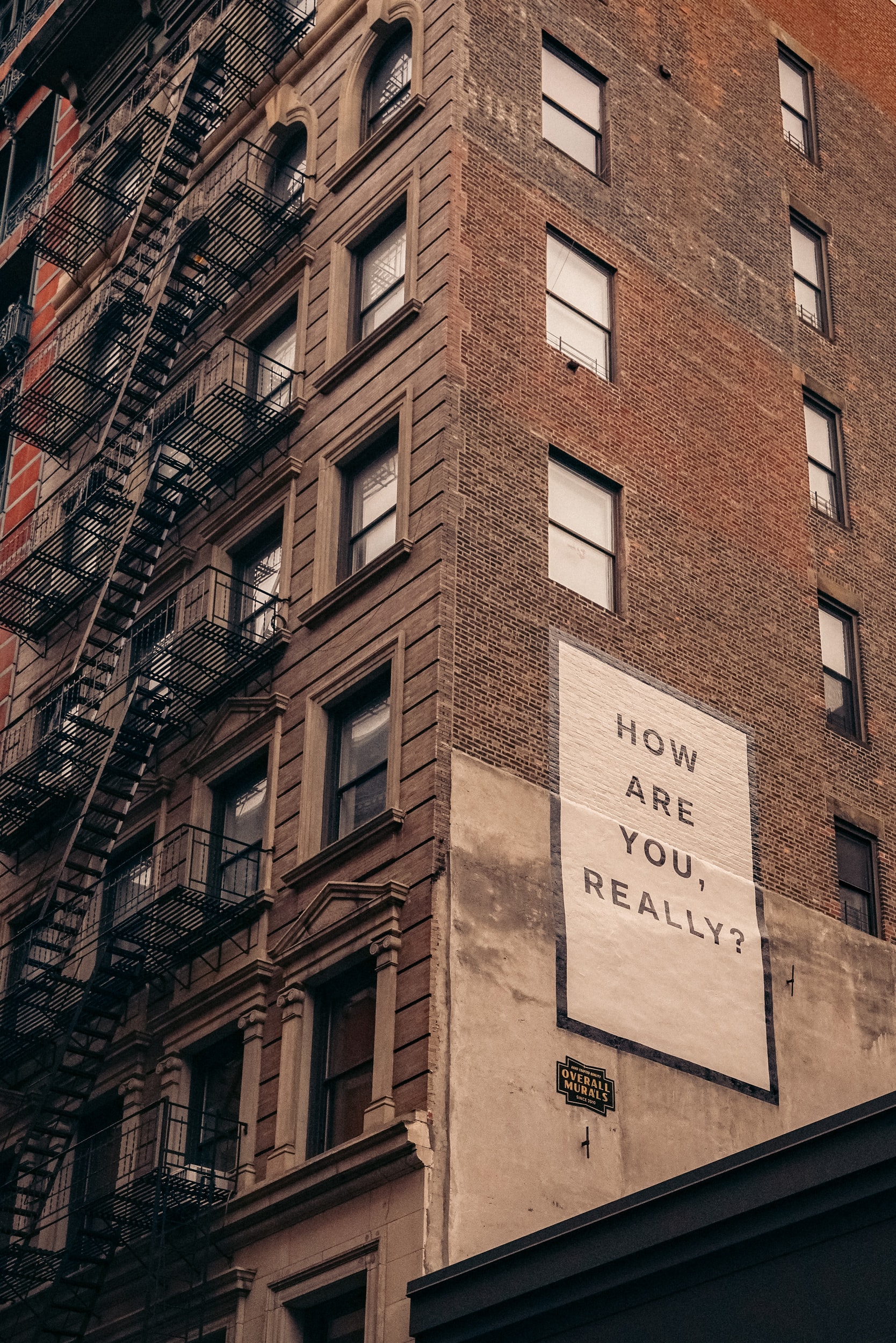
But, you can’t do that when you are a busy pre-med student working full time and taking classes! We are expected to stay strong and keep up our front that says “Everything’s fine,” when, in fact, we’re not. I had great people to talk to and that would listen to me, but I still went through a mourning process. I mourned my life before when I thought I “just had a sensitive stomach.” I mourned that fact that my diet would probably change and change again and that I maybe would have to be on immunosuppressive medication. I dreaded the future conversations that would come up when someone would ask why I had to go to the bathroom so much or why I couldn’t eat or drink something. Really, everything’s fine…
But, it’s not. CHRONIC is a word that I hoped never to hear in regard to my medical history. We now have a new label that we must carry for the rest of our lives, and it’s anything but predictable. We have to explain this diagnosis so many times we feel like it might actually define us. The reality of my UC diagnosis began to truly sink in and anxiety began to seep into my daily life. My energy and concentration was poured into reading about UC, finding a better “diet”, looking for tips on how to achieve and stay in remission, and finding some kind of outlet for my anger and frustration.
Honestly, I should have given myself a little more time to process and try to seek the help of a mental health professional. Now, I think, I should’ve thought about my IBD and mental health together rather than separately. I let myself have a little time to mourn my UC diagnosis, but I thought I needed to be strong and keep my diagnosis to myself, much like others had before me. If we don’t look sick, perhaps no one will know. Even when we try our best to be strong and adapt to this normal, our mental health often still ends up suffering.
I think it would make such a positive difference in the lives of so many if we are all equipped with a medical and mental health treatment plan after being diagnosed with IBD, because the fact of the matter is that the mental health symptoms are just as debilitating as the physical symptoms of IBD, and they’re often intertwined. We need this kind of support as we manage our diagnosis - which sometimes can land us in the hospital or needing major surgery. I can’t speak to these kinds of experiences, but they can be traumatic in their own ways. How many failed medications or pain does one endure until they receive a potentially life-changing surgery? Thinking of the mental health hurdles that my co-fellows have dealt with and shared so vulnerably leaves me in awe of their strength. When they share what they have lived through, it also makes me sad that there was not adequate mental health services available to some of them when it could have offered an outlet for some of their pain.
Even now, almost 5 years out from my diagnosis, I take medication for my depression/anxiety and have re-established a relationship with a counselor that has experience in treating clients with chronic illnesses. I still go through the peaks and valleys of life and IBD, but, now, I’m better equipped to handle the lows when they hit or when a flare affects my mood and interest in doing things. I want the mental health support that has been so instrumental to some of my healing to be more accessible and affordable for those with IBD in the near future.
I hope speaking candidly about mental health and sharing some of these reflections helps you feel less alone and more validated in what you’ve been going through. The process of untangling all of these emotions is normal when grappling with a chronic illness diagnosis and what that means for you and those you love. Everyone processes major life changes and trauma differently, but don’t be afraid to ask about mental health services when you see your GI or primary care provider. Finding the right mental health support could be the treatment you never knew you needed.